J Korean Thyroid Assoc.
2012 Nov;5(2):114-123. 10.11106/jkta.2012.5.2.114.
Problems in Diagnosis and Management of Follicular Neoplasm
- Affiliations
-
- 1Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. kimwb@amc.seoul.kr
- KMID: 2095100
- DOI: http://doi.org/10.11106/jkta.2012.5.2.114
Abstract
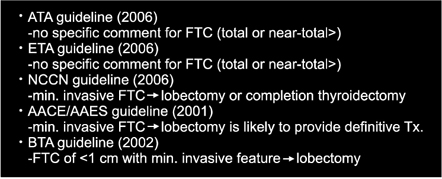
- Thyroid follicular adenoma and hyperplastic adenomatoid nodule may show overlapping cytologic pattern with thyroid follicular carcinoma and follicular variant of thyroid papillary carcinoma. Fine-needle aspiration cytology (FNAC) has limited role in differential diagnosis of those lesions showing high cellularity and absence of colloid. Those lesions are conventionally termed 'follicular neoplasm'. As diagnostic hallmarks of follicular carcinoma (vascular- and capsular invasion) cannot be detected by cytology, verification by histology after surgery is mandatory. However, only 20% of patients with thyroid nodules diagnosed cytologically as 'follicular neoplasm' are finally diagnosed as carcinoma after surgery. Therefore, there have been many trials to differentiate follicular adenoma (FA) from follicular carcinoma (FTC) in preoperative setting. Among those trials are 1) cell morphometry analysis by computer graphics, analysis of telomerase expression level, quantitation of specific protein markers, or intensive cytological analysis using FNAC specimens, 2) ultrasonographic evaluation, dynamic MRI, or MR spectroscopy for thyroid nodules and 3) gene expression profile analysis for thyroid nodules by microarray technique, all showing limited success or limitations hampering clinical application. Similarly, intra-operative frozen section analysis of thyroid nodule had been known to be of no diagnostic utility in a prospective, randomized trial. Current management strategy for 'follicular neoplasm' is initial surgery for diagnostic purpose to get pathologic diagnosis. If the nodule is diagnosed finally as FTC, completion thyroidectomy with or without radioactive iodine therapy is recommended in most cases. Minimally invasive FTC (without vascular invasion) is known to have excellent prognosis in most cases, so traditionally those patients had undergone unilateral operation without completion thyroidectomy. But, there had been reported cases showing distant metastasis and/or recurrence in patients with 'minimally invasive FTC'. One of problems in diagnosis of 'minimally invasive FTC' is lack of international standardization for pathologic diagnosis. Optimal surgical extent for cases with FTC is not known yet. It might have been due to lack of risk stratification of patients which is unique to FTC (not well differentiated thyroid cancer as a whole), lack of biomarker predicting prognosis of FTC, and lack of controlled trial for management of patients with FTC. In near future, application of molecular diagnostic markers is expected to improve our management strategy for thyroid nodules diagnosed as 'follicular neoplasm', if molecular pathogenesis of FA and of FTC are comprehensively understood.
MeSH Terms
-
Adenocarcinoma, Follicular
Adenoma
Biopsy, Fine-Needle
Carcinoma, Papillary
Colloids
Computer Graphics
Diagnosis, Differential
Frozen Sections
Humans
Iodine
Magnetic Resonance Spectroscopy
Neoplasm Metastasis
Pathology, Molecular
Prognosis
Recurrence
Telomerase
Thyroid Gland
Thyroid Neoplasms
Thyroid Nodule
Thyroidectomy
Transcriptome
Colloids
Iodine
Telomerase
Figure
Reference
-
1. DeLellis RA. Pathology and genetics of thyroid carcinoma. J Surg Oncol. 2006. 94(8):662–669.
Article2. Nikiforova MN, Lynch RA, Biddinger PW, Alexander EK, Dorn GW 2nd, Tallini G, et al. RAS point mutations and PAX8-PPAR gamma rearrangement in thyroid tumors: evidence for distinct molecular pathways in thyroid follicular carcinoma. J Clin Endocrinol Metab. 2003. 88(5):2318–2326.
Article3. Schmid KW, Farid NR. How to define follicular thyroid carcinoma? Virchows Arch. 2006. 448(4):385–393.
Article4. Lin JD, Chao TC. Follicular thyroid carcinoma: from diagnosis to treatment. Endocr J. 2006. 53(4):441–448.
Article5. Baloch ZW, Fleisher S, LiVolsi VA, Gupta PK. Diagnosis of "follicular neoplasm": a gray zone in thyroid fine-needle aspiration cytology. Diagn Cytopathol. 2002. 26(1):41–44.
Article6. Sidawy MK, Del Vecchio DM, Knoll SM. Fine-needle aspiration of thyroid nodules: correlation between cytology and histology and evaluation of discrepant cases. Cancer. 1997. 81(4):253–259.7. Baloch ZW, Livolsi VA. Follicular-patterned lesions of the thyroid: the bane of the pathologist. Am J Clin Pathol. 2002. 117(1):143–150.8. Yang J, Schnadig V, Logrono R, Wasserman PG. Fine-needle aspiration of thyroid nodules: a study of 4703 patients with histologic and clinical correlations. Cancer. 2007. 111(5):306–315.
Article9. Tuttle RM, Lemar H, Burch HB. Clinical features associated with an increased risk of thyroid malignancy in patients with follicular neoplasia by fine-needle aspiration. Thyroid. 1998. 8(5):377–383.
Article10. Schlinkert RT, van Heerden JA, Goellner JR, Gharib H, Smith SL, Rosales RF, et al. Factors that predict malignant thyroid lesions when fine-needle aspiration is "suspicious for follicular neoplasm". Mayo Clin Proc. 1997. 72(10):913–916.
Article11. Frasoldati A, Flora M, Pesenti M, Caroggio A, Valcavil R. Computer-assisted cell morphometry and ploidy analysis in the assessment of thyroid follicular neoplasms. Thyroid. 2001. 11(10):941–946.
Article12. Saji M, Xydas S, Westra WH, Liang CK, Clark DP, Udelsman R, et al. Human telomerase reverse transcriptase (hTERT) gene expression in thyroid neoplasms. Clin Cancer Res. 1999. 5(6):1483–1489.13. Guerra LN, Miler EA, Moiguer S, Karner M, Orlandi AM, Fideleff H, et al. Telomerase activity in fine needle aspiration biopsy samples: application to diagnosis of human thyroid carcinoma. Clin Chim Acta. 2006. 370(1-2):180–184.
Article14. Saggiorato E, Cappia S, De Giuli P, Mussa A, Pancani G, Caraci P, et al. Galectin-3 as a presurgical immunocytodiagnostic marker of minimally invasive follicular thyroid carcinoma. J Clin Endocrinol Metab. 2001. 86(11):5152–5158.
Article15. Saggiorato E, De Pompa R, Volante M, Cappia S, Arecco F, Dei Tos AP, et al. Characterization of thyroid 'follicular neoplasms' in fine-needle aspiration cytological specimens using a panel of immunohistochemical markers: a proposal for clinical application. Endocr Relat Cancer. 2005. 12(2):305–317.
Article16. Cerutti JM, Latini FR, Nakabashi C, Delcelo R, Andrade VP, Amadei MJ, et al. Diagnosis of suspicious thyroid nodules using four protein biomarkers. Clin Cancer Res. 2006. 12(11 Pt 1):3311–3318.
Article17. Segev DL, Clark DP, Zeiger MA, Umbricht C. Beyond the suspicious thyroid fine needle aspirate. A review. Acta Cytol. 2003. 47(5):709–722.18. Lubitz CC, Faquin WC, Yang J, Mekel M, Gaz RD, Parangi S, et al. Clinical and cytological features predictive of malignancy in thyroid follicular neoplasms. Thyroid. 2010. 20(1):25–31.
Article19. Rago T, Di Coscio G, Basolo F, Scutari M, Elisei R, Berti P, et al. Combined clinical, thyroid ultrasound and cytological features help to predict thyroid malignancy in follicular and Hupsilonrthle cell thyroid lesions: results from a series of 505 consecutive patients. Clin Endocrinol (Oxf). 2007. 66(1):13–20.20. Kobayashi K, Fukata S, Miyauchi A. Diagnosis of follicular carcinoma of the thyroid: role of sonography in preoperative diagnosis of follicular nodules. J Med Ultrason. 2005. 32:153–158.
Article21. Kihara M, Ito Y, Hirokawa M, Masuoka H, Yabuta T, Tomoda C, et al. Role of ultrasonography in patients with cytologically follicular thyroid tumor. Auris Nasus Larynx. 2011. 38(4):508–511.
Article22. Kim JM, Ryu JS, Kim TY, Kim WB, Kwon GY, Gong G, et al. 18F-fluorodeoxyglucose positron emission tomography does not predict malignancy in thyroid nodules cytologically diagnosed as follicular neoplasm. J Clin Endocrinol Metab. 2007. 92(5):1630–1634.
Article23. Gupta N, Goswami B, Chowdhury V, Ravishankar L, Kakar A. Evaluation of the role of magnetic resonance spectroscopy in the diagnosis of follicular malignancies of thyroid. Arch Surg. 2011. 146(2):179–182.
Article24. Gupta N, Norbu C, Goswami B, Chowdhury V, RaviShankar L, Gulati P, et al. Role of dynamic MRI in differentiating benign from malignant follicular thyroid nodule. Auris Nasus Larynx. 2011. 38(6):718–723.
Article25. Petric R, Perhavec A, Gazic B, Besic N. Preoperative serum thyroglobulin concentration is an independent predictive factor of malignancy in follicular neoplasms of the thyroid gland. J Surg Oncol. 2012. 105(4):351–356.
Article26. Duh QY. What's new in general surgery: endocrine surgery. J Am Coll Surg. 2005. 201(5):746–753.
Article27. Barden CB, Shister KW, Zhu B, Guiter G, Greenblatt DY, Zeiger MA, et al. Classification of follicular thyroid tumors by molecular signature: results of gene profiling. Clin Cancer Res. 2003. 9(5):1792–1800.28. Cerutti JM, Delcelo R, Amadei MJ, Nakabashi C, Maciel RM, Peterson B, et al. A preoperative diagnostic test that distinguishes benign from malignant thyroid carcinoma based on gene expression. J Clin Invest. 2004. 113(8):1234–1242.
Article29. Weber F, Shen L, Aldred MA, Morrison CD, Frilling A, Saji M, et al. Genetic classification of benign and malignant thyroid follicular neoplasia based on a three-gene combination. J Clin Endocrinol Metab. 2005. 90(5):2512–2521.
Article30. Carling T, Udelsman R. Follicular neoplasms of the thyroid: what to recommend. Thyroid. 2005. 15(6):583–587.
Article31. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2006. 16(2):109–142.
Article32. Udelsman R, Westra WH, Donovan PI, Sohn TA, Cameron JL. Randomized prospective evaluation of frozen-section analysis for follicular neoplasms of the thyroid. Ann Surg. 2001. 233(5):716–722.
Article33. Pacini F, Schlumberger M, Dralle H, Elisei R, Smit JW, Wiersinga W. European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol. 2006. 154(6):787–803.
Article34. National Comprehensive Cancer Network. Thyroid carcinoma. cited 2012 Nov 3. Available from: URL: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.35. Cobin RH, Gharib H, Bergman DA, Clark OH, Cooper DS, Daniels GH, et al. American Association of Clinical Endocrinologists. American College of Endocrinology. AACE/AAES medical/surgical guidelines for clinical practice: management of thyroid carcinoma. Endocr Pract. 2001. 7(3):202–220.
Article36. British Thyroid Association and Royal College of Physicians. Guidelines for the management of thyroid cancer in adults. 2002. London: RCP.37. D'Avanzo A, Treseler P, Ituarte PH, Wong M, Streja L, Greenspan FS, et al. Follicular thyroid carcinoma: histology and prognosis. Cancer. 2004. 100(6):1123–1129.38. Hedinger CE, Williams ED, Sobin LH. Hedinger CE, editor. Histological typing of thyroid tumours. International histological classification of tumors. 1988. vol. 11. Berlin: Springer-Verlag;7–68.
Article39. Rosai J, Carcangiu ML, DeLellis RA. Rosai J, Sobin LH, editors. Tumours of the thyroid gland. Atlas of tumor pathology, 3rd series, fascicle 5. 1992. Washington, DC: Armed Forces Institute of Pathology;49–63.40. Lang W, Choritz H, Hundeshagen H. Risk factors in follicular thyroid carcinomas. A retrospective follow-up study covering a 14-year period with emphasis on morphological findings. Am J Surg Pathol. 1986. 10(4):246–255.41. Thompson LD, Wieneke JA, Paal E, Frommelt RA, Adair CF, Heffess CS. A clinicopathologic study of minimally invasive follicular carcinoma of the thyroid gland with a review of the English literature. Cancer. 2001. 91(3):505–524.
Article42. Delbridge L, Parkyn R, Philips J, Barraclough B, Robinson B. Minimally invasive follicular thyroid carcinoma: completion thyroidectomy or not? ANZ J Surg. 2002. 72(11):844–845.
Article43. Goldstein NS, Czako P, Neill JS. Metastatic minimally invasive (encapsulated) follicular and Hurthle cell thyroid carcinoma: a study of 34 patients. Mod Pathol. 2000. 13(2):123–130.
Article44. Dralle H, Machens A. Surgical approaches in thyroid cancer and lymph-node metastases. Best Pract Res Clin Endocrinol Metab. 2008. 22(6):971–987.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Dilemma of a Follicular Lesions/Neoplasm in Thyroid Fine Needle Aspiration Cytology
- Diagnostic Effects of Fine Needle Aspiration Cytology and Frozen Section for Follicular Neoplasm of the Thyroid
- Definition and Prognostic Factor of Minimally Invasive Follicular Thyroid Carcinoma
- Morphometric Study on Fine Needle Aspirates from Follicular Adenoma and Follicular Carcinoma of the Thyroid
- Discrepancy between Preoperative Fine Needle Aspiration Cytology and Postoperative Histologic Diagnosis in Follicular Tumors of the Thyroid