Microbiology and Epidemiology of Infectious Spinal Disease
- Affiliations
-
- 1Department of Neurosurgery, School of Medicine, Chungnam National University, Daejeon, Korea. swchoi@cnu.ac.kr
- 2Department of Neurosurgery, Konyang University Hospital, Daejeon, Korea.
- 3Department of Neurosurgery, The Catholic University of Korea College of Medicine, Daejeon St. Mary's Hospital, Daejeon, Korea.
- KMID: 2067072
- DOI: http://doi.org/10.3340/jkns.2014.56.1.21
Abstract
OBJECTIVE
Infectious spinal disease is regarded as an infection by a specific organism that affects the vertebral body, intervertebral disc and adjacent perivertebral soft tissue. Its incidence seems to be increasing as a result of larger proportion of the older patients with chronic debilitating disease, the rise of intravenous drug abuser, and the increase in spinal procedure and surgery. In Korea, studies assessing infectious spinal disease are rare and have not been addressed in recent times. The objectives of this study are to describe the epidemiology of all kind of spinal infectious disease and their clinical and microbiological characteristics as well as to assess the diagnostic methodology and the parameters related to the outcomes.
METHODS
A retrospective study was performed in all infectious spinal disease cases presenting from January 2005 to April 2010 to three tertiary teaching hospitals within a city of 1.5 million in Korea. Patient demographics, risk factors, clinical features, and outcomes were assessed. Risk factors entailed the presence of diabetes, chronic renal failure, liver cirrhosis, immunosuppressants, remote infection, underlying malignancy and previous spinal surgery or procedure. We comparatively analyzed the results between the groups of pyogenic and tuberculous spinal infection. SPSS version 14 statistical software was used to perform the analyses of the data. The threshold for statistical significance was established at p<0.05.
RESULTS
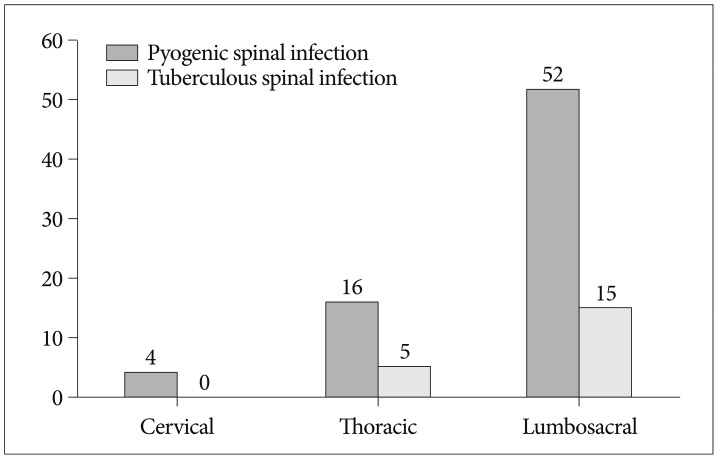
Ninety-two cases fulfilled the inclusion criteria and were reviewed. Overall, patients of tuberculous spinal infection (TSI) and pyogenic spinal infection (PSI) entailed 20 (21.7%) and 72 (78.3%) cases, respectively. A previous spinal surgery or procedure was the most commonly noted risk factor (39.1%), followed by diabetes (15.2%). The occurrence of both pyogenic and tuberculous spondylitis was predominant in the lumbar spine. Discs are more easily invaded in PSI. At initial presentation, white cell blood count and C-reactive protein levels were higher in PSI compared to TSI (p<0.05). Etiological agents were identified in 53.3%, and the most effective method for identification of etiological agents was tissue culture (50.0%). Staphyococcus aureus was the most commonly isolated infective agent associated with pyogenic spondylitis, followed by E. coli. Surgical treatment was performed in 31.5% of pyogenic spondylitis and in 35.0% of tuberculous spondylitis cases.
CONCLUSION
Many previous studies in Korea usually reported that tuberculous spondylitis is the predominant infection. However, in our study, the number of pyogenic infection was 3 times greater than that of tuberculous spinal disease. Etiological agents were identified in a half of all infectious spinal disease. For better outcomes, we should try to identify the causative microorganism before antibiotic therapy and make every effort to improve the result of culture and biopsy.
Keyword
MeSH Terms
-
Biopsy
C-Reactive Protein
Communicable Diseases
Demography
Drug Users
Epidemiology*
Hospitals, Teaching
Humans
Immunosuppressive Agents
Incidence
Intervertebral Disc
Kidney Failure, Chronic
Korea
Liver Cirrhosis
Osteomyelitis
Retrospective Studies
Risk Factors
Spinal Diseases*
Spine
Spondylitis
Tuberculosis
C-Reactive Protein
Immunosuppressive Agents
Figure
Cited by 7 articles
-
Changes of Biomarkers before and after Antibiotic Treatment in Spinal Infection
Young Lee, Jeongwook Lim, Seung-Won Choi, Sanghyun Han, Bumsoo Park, Jin-Young Youm
Korean J Neurotrauma. 2019;15(2):143-149. doi: 10.13004/kjnt.2019.15.e19.Bone scintigraphy in patients with pain
Seung Hyeon Shin, Seong Jang Kim
Korean J Pain. 2017;30(3):165-175. doi: 10.3344/kjp.2017.30.3.165.Prospective Multicenter Surveillance Study of Surgical Site Infection after Spinal Surgery in Korea : A Preliminary Study
Tae Seok Jeong, Gi Taek Yee
J Korean Neurosurg Soc. 2018;61(5):608-617. doi: 10.3340/jkns.2018.0118.Change of Pyogenic and Tuberculous Spondylitis between 2007 and 2016 Year : A Nationwide Study
Yeon Jee Kim, Je Beom Hong, Yeo Song Kim, Jeeeun Yi, Jung Min Choi, Seil Sohn
J Korean Neurosurg Soc. 2020;63(6):784-793. doi: 10.3340/jkns.2020.0013.Clinical Value of Procalcitonin in Patients with Spinal Infection
Deok-Ki Jeong, Hyun-Woo Lee, Young-Min Kwon
J Korean Neurosurg Soc. 2015;58(3):271-275. doi: 10.3340/jkns.2015.58.3.271.Comparative Analysis of Spontaneous Infectious Spondylitis : Pyogenic versus Tuberculous
Yangwon Lee, Bum-Joon Kim, Se-Hoon Kim, Seung-Hwan Lee, Won-Hyung Kim, Sung-Won Jin
J Korean Neurosurg Soc. 2018;61(1):81-88. doi: 10.3340/jkns.2016.1212.005.Association between ischemic stroke and pyogenic spondylitis in Korea: Nationwide longitudinal cohort study
Soo Hyun Lee, Hakyung Kim, In-bo Han, Seung Hun Sheen, Je Beom Hong, Seil Sohn
J Cerebrovasc Endovasc Neurosurg. 2023;25(2):143-149. doi: 10.7461/jcen.2023.E2022.09.001.
Reference
-
1. Ahmed M, Modic MT. Degenerative disease and infection : role of imaging. In : Benzel EC, Francis TB, editors. Spine Surgery : Techniques, Complication Avoidance, and Management. ed 3. Philadelphia, PA: Elsevier/Saunders;2012. p. 1623–1646.2. Bhagat S, Mathieson C, Jandhyala R, Johnston R. Spondylodiscitis (disc space infection) associated with negative microbiological tests : comparison of outcome of suspected disc space infections to documented non-tuberculous pyogenic discitis. Br J Neurosurg. 2007; 21:473–477. PMID: 17852101.
Article3. Capelo J, Carragoso A, Albuquerque C, Mocho ML, Canto-Moreira N. [Infectious spondylodiscitis : a study of forty-one cases]. Acta Reumatol Port. 2007; 32:255–262. PMID: 17932476.4. Chang HG. Tuberculous infection of the spine. J Korean Soc Spine Surg. 1999; 6:237–246.5. Colmenero JD, Reguera JM, Fernández-Nebro A, Cabrera-Franquelo F. Osteoarticular complications of brucellosis. Ann Rheum Dis. 1991; 50:23–26. PMID: 1994863.
Article6. Cottle L, Riordan T. Infectious spondylodiscitis. J Infect. 2008; 56:401–412. PMID: 18442854.
Article7. D'Agostino C, Scorzolini L, Massetti AP, Carnevalini M, d'Ettorre G, Venditti M, et al. A seven-year prospective study on spondylodiscitis : epidemiological and microbiological features. Infection. 2010; 38:102–107. PMID: 20191397.8. Fuentes Ferrer M, Gutiérrez Torres L, Ayala Ramírez O, Rumayor Zarzuelo M, del Prado González N. Tuberculosis of the spine. A systematic review of case series. Int Orthop. 2012; 36:221–231. PMID: 22116392.
Article9. Fuursted K, Arpi M, Lindblad BE, Pedersen LN. Broad-range PCR as a supplement to culture for detection of bacterial pathogens in patients with a clinically diagnosed spinal infection. Scand J Infect Dis. 2008; 40:772–777. PMID: 18609207.
Article10. Gasbarrini A, Boriani L, Salvadori C, Mobarec S, Kreshak J, Nanni C, et al. Biopsy for suspected spondylodiscitis. Eur Rev Med Pharmacol Sci. 2012; 16(Suppl 2):26–34. PMID: 22655481.11. Helewa RM, Embil JM, Boughen CG, Cheang M, Goytan M, Zacharias JM, et al. Risk factors for infectious spondylodiscitis in patients receiving hemodialysis. Infect Control Hosp Epidemiol. 2008; 29:567–571. PMID: 18510467.
Article12. Hong YP, Kim SJ, Lew WJ, Lee EK, Han YC. The seventh nationwide tuberculosis prevalence survey in Korea, 1995. Int J Tuberc Lung Dis. 1998; 2:27–36. PMID: 9562108.13. Kayani I, Syed I, Saifuddin A, Green R, MacSweeney F. Vertebral osteomyelitis without disc involvement. Clin Radiol. 2004; 59:881–891. PMID: 15451346.
Article14. Kim BJ, Ko HS, Lim Y, Seo JG, Zoo SK, Jeon TH. The clinical study of the tuberculous spondylitis. J Korean Orthop Assoc. 1993; 28:2221–2232.
Article15. Kim CJ, Song KH, Jeon JH, Park WB, Park SW, Kim HB, et al. A comparative study of pyogenic and tuberculous spondylodiscitis. Spine (Phila Pa 1976). 2010; 35:E1096–E1100. PMID: 20838270.
Article16. Kim CW, Currier BL, Eismont FJ. Infections of the spine. In : Herkowitz HN, Balderston RA, editors. Rothman-Simeone the Spine. ed 5. Philadelphia: Saunders/Elsevier;2011. p. 1513–1570.17. Kim SW, Lee SM, Shin H. Preoperative gadolinium-enhanced magneticresonance images on infectious spondylitis. J Korean Neurosurg Soc. 2005; 38:355–358.18. Kim YH, Song JK, Shin H. A clinical analysis of surgically managed tuberculous spondylitis. J Korean Neurosurg Soc. 1997; 26:223–234.19. Lee KS, Doh JW, Bae HG, Yun IG. Primary infections disorders of the spine : report of 40 cases. J Korean Neurosurg Soc. 1996; 25:1655–1660.20. Lee KY, Sohn SK, Hwang KS. Comparison of pyogenic and tuberculous spondylitis. J Korean Soc Spine Surg. 1999; 6:443–450.21. Luzzati R, Giacomazzi D, Danzi MC, Tacconi L, Concia E, Vento S. Diagnosis, management and outcome of clinically-suspected spinal infection. J Infect. 2009; 58:259–265. PMID: 19268368.
Article22. McHenry MC, Easley KA, Locker GA. Vertebral osteomyelitis : long-term outcome for 253 patients from 7 Cleveland-area hospitals. Clin Infect Dis. 2002; 34:1342–1350. PMID: 11981730.
Article23. Merino P, Candel FJ, Gestoso I, Baos E, Picazo J. Microbiological diagnosis of spinal tuberculosis. Int Orthop. 2012; 36:233–238. PMID: 22252412.
Article24. Park JH, Kim KH. A clinical analysis of surgically managed primary spondylitis. J Korean Neurosurg Soc. 2001; 30:1163–1169.25. Pintado-García V. [Infectious spondylitis]. Enferm Infecc Microbiol Clin. 2008; 26:510–517. PMID: 19094866.26. Rivas-Garcia A, Sarria-Estrada S, Torrents-Odin C, Casas-Gomila L, Franquet E. Imaging findings of Pott's disease. Eur Spine J. 22(Suppl 4):2013; 567–578. PMID: 22684257.
Article27. Vollmer DG, Tandon N. Infection of the spine. In : Winn HR, editor. Youmans Neurological Surgical. ed 6. Philadelphia, PA: Saunders/Elsevier;2011. p. 3216–3232.28. Whee SM, Eoh W, Nam DH, Lee JI, Kim JS, Hong SC, et al. Clinical evaluation of surgical treatments for ten cases of tuberculous spondylitis. J Korean Neurosurg Soc. 2001; 30:1314–1319.29. Yee DK, Samartzis D, Wong YW, Luk KD, Cheung KM. Infective spondylitis in Southern Chinese : a descriptive and comparative study of ninety-one cases. Spine (Phila Pa 1976). 2010; 35:635–641. PMID: 20195195.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clostridium difficile Infection: A Worldwide Disease
- Etiologic and epidemiologic analysis of bacterial infectious upper respiratory disease in Thoroughbred horses at the Seoul Race Park
- National Infectious Diseases Surveillance data of South Korea
- The Epidemiology and Importance of Osteoporotic Spinal Compression Fracture in South Korea
- Legal Issues in Quarantine and Isolation for Control of Emerging Infectious Diseases