Pediatr Gastroenterol Hepatol Nutr.
2013 Sep;16(3):178-184. 10.5223/pghn.2013.16.3.178.
Pre-diagnostic Clinical Presentations and Medical History Prior to the Diagnosis of Inflammatory Bowel Disease in Children
- Affiliations
-
- 1Department of Pediatrics, Hanyang University College of Medicine, Seoul, Korea. kyjoo@hanyang.ac.kr
- KMID: 2051331
- DOI: http://doi.org/10.5223/pghn.2013.16.3.178
Abstract
- PURPOSE
The clinical presentations of inflammatory bowel disease (IBD) prior to diagnosis are so diverse or vague that many of them waste time before final diagnosis. This study was undertaken to know the medical history of the pediatric patients until the final diagnosis could be reached.
METHODS
The medical records of all pediatric patients who were diagnosed with IBD (Crohn's disease [CD] in 14 children, ulcerative colitis [UC] in 17) during the last 13 years were reviewed. We investigated the length of the diagnostic time lag, chief clinical presentation, and any useful laboratory predictor among the routinely performed examinations. Indeterminate colitis was not included.
RESULTS
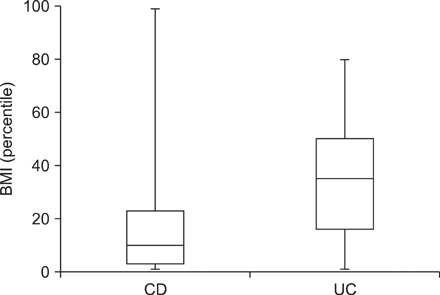
The mean ages of children at the final diagnosis was similar in both diseases. As for the pre-clinical past history of bowel symptoms in CD patients, 5 were previously healthy, 9 had had 1-3 gastrointestinal (GI) symptoms, weight loss, bloody stool, anemia and rectal prolapse. With UC, 9 were previously healthy, 8 had had 1-3 GI symptoms, bloody stool, anorexia. The average diagnostic time lag with CD was 3.36 months, and with UC 2.2 months. Body mass index (BMI) and the initial basic laboratory data (white blood cell, hemoglobin, mean corpuscular volume, serum albumin, and serum total protein) were lower in CD, statistically significant only in BMI.
CONCLUSION
IBD shows diverse clinical symptoms before its classical features, making the patients waste time until diagnosis. It is important to concern possibility of IBD even in the mildly sick children who do not show the characteristic symptoms of IBD.
Keyword
MeSH Terms
Figure
Reference
-
1. Porter CK, Cash BD, Pimentel M, Akinseye A, Riddle MS. Risk of inflammatory bowel disease following a diagnosis of irritable bowel syndrome. BMC Gastroenterol. 2012; 12:55.
Article2. Mearin F, Perelló A, Balboa A. Irritable bowel syndrome and inflammatory bowel disease: Is there a connection? Gastroenterol Hepatol. 2009; 32:364–372.3. García Rodríguez LA, Ruigómez A, Wallander MA, Johansson S, Olbe L. Detection of colorectal tumor and inflammatory bowel disease during follow-up of patients with initial diagnosis of irritable bowel syndrome. Scand J Gastroenterol. 2000; 35:306–311.
Article4. Porter CK, Tribble DR, Aliaga PA, Halvorson HA, Riddle MS. Infectious gastroenteritis and risk of developing inflammatory bowel disease. Gastroenterology. 2008; 135:781–786.
Article5. Dilauro S, Crum-Cianflone NF. Ileitis: when it is not Crohn's disease. Curr Gastroenterol Rep. 2010; 12:249–258.
Article6. Zhou ZY, Luo HS. Differential diagnosis between Crohn's disease and intestinal tuberculosis in China. Int J Clin Pract. 2006; 60:212–214.
Article7. Jin XJ, Kim JM, Kim HK, Kim L, Choi SJ, Park IS, et al. Histopathology and TB-PCR kit analysis in differentiating the diagnosis of intestinal tuberculosis and Crohn's disease. World J Gastroenterol. 2010; 16:2496–2503.
Article8. van Dijken TD, Vastert SJ, Gerloni VM, Pontikaki I, Linnemann K, Girschick H, et al. Development of inflammatory bowel disease in patients with juvenile idiopathic arthritis treated with etanercept. J Rheumatol. 2011; 38:1441–1446.
Article9. Kokkonen J, Arvonen M, Vähäsalo P, Karttunen TJ. Intestinal immune activation in juvenile idiopathic arthritis and connective tissue disease. Scand J Rheumatol. 2007; 36:386–389.
Article10. Saro Gismera C, Lacort Fernández M, Argüelles Fernández G, Antón Magarzo J, Navascues CA, Garcia López R, et al. Epidemiology of chronic inflammatory bowel disease in Gijón, Asturias. Gastroenterol Hepatol. 2001; 24:228–235.11. Saro Gismera C, Riestra Menéndez S, Sánchez Fernández R, Milla Crespo A, Lacort Fernández M, Argüelles Fernández G, et al. Epidemiology in inflammatory bowel disease in five areas of Asturias. Spain. An Med Interna. 2003; 20:232–238.12. Lee JH. Inflammatory bowel disease in pediatric age. Korean J Pediatr Gastroenterol Nutr. 2011; 14:Suppl 1. S34–S41.
Article13. Benchimol EI, Guttmann A, Griffiths AM, Rabeneck L, Mack DR, Brill H, et al. Increasing incidence of paediatric inflammatory bowel disease in Ontario, Canada: evidence from health administrative data. Gut. 2009; 58:1490–1497.
Article14. Yeşil A, Senateş E, Bayoğlu IV, Erdem ED, Demirtunç R, Kurdaş Övünç AO. Red cell distribution width: a novel marker of activity in inflammatory bowel disease. Gut Liver. 2011; 5:460–467.
Article15. Bager P, Befrits R, Wikman O, Lindgren S, Moum B, Hjortswang H, et al. The prevalence of anemia and iron deficiency in IBD outpatients in Scandinavia. Scand J Gastroenterol. 2011; 46:304–309.
Article16. Mijac DD, Janković GL, Jorga J, Krstić MN. Nutritional status in patients with active inflammatory bowel disease: prevalence of malnutrition and methods for routine nutritional assessment. Eur J Intern Med. 2010; 21:315–319.
Article17. Hébuterne X, Filippi J, Al-Jaouni R, Schneider S. Nutritional consequences and nutrition therapy in Crohn's disease. Gastroenterol Clin Biol. 2009; 33:Suppl 3. S235–S244.
Article18. Mullin GE. Micronutrients and inflammatory bowel disease. Nutr Clin Pract. 2012; 27:136–137.
Article19. Savoye G, Salleron J, Gower-Rousseau C, Dupas JL, Vernier-Massouille G, Fumery M, et al. Clinical predictors at diagnosis of disabling pediatric Crohn's disease. Inflamm Bowel Dis. 2012; 18:2072–2078.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Treatment of Inflammatory Bowel Disease
- Inflammatory Bowel Disease in Pediatric Age
- Diagnostic Tips for Making the Diagnosis of Inflammatory Bowel Disease
- Pediatric abdominal pain: the need for a careful differential diagnosis according to age
- The Pharmacotherapy of Inflammatory Bowel Disease in Child and Adolescence