Clin Nutr Res.
2015 Jan;4(1):46-55. 10.7762/cnr.2015.4.1.46.
A Better Diet Quality is Attributable to Adequate Energy Intake in Hemodialysis Patients
- Affiliations
-
- 1Department of Family Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul 110-746, Korea.
- 2Medical Research Center, Sungkyunkwan University School of Medicine, Suwon 440-746, Korea.
- 3Department of Medical Nutrition, Graduate School of East-West Medical Science, Kyung Hee University, Yongin 447-701, Korea. hjlim@khu.ac.kr, rwcho@khu.ac.kr
- 4Research Institute of Medical Nutrition, Kyung Hee University, Seoul 130-701, Korea.
- KMID: 2049162
- DOI: http://doi.org/10.7762/cnr.2015.4.1.46
Abstract
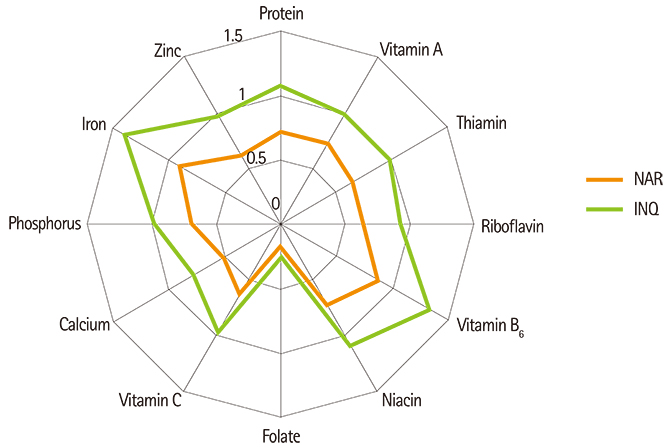
- Poor diet quality is one of strong predictors of subsequent increased mortality in hemodialysis patients. To determine diet quality and to define major problems contributing to poor diet quality in hemodialysis patients, a cross-sectional study was conducted between June 2009 and October 2010. Sixty-three hemodialysis patients (31 men, 32 women; aged 55.3 +/- 11.9 years) in stable condition were recruited from the Artificial Kidney Center in Kyung Hee University, Seoul, Korea. Three-day diet records were obtained for dietary assessment. Mean adequacy ratio (MAR) is the average of the ratio of intakes to Dietary Reference Intakes (DRI) for 12 nutrients. Index of nutritional quality (INQ) was determined as the nutritional density per 1,000 kcal of calories. Overall diet quality was evaluated using the Diet Quality Index-International (DQI-I). Statistics were used to determine diet quality, comparing dietary intake to DRI. Dietary calories (21.9 +/- 6.7 kcal/kg/day) and protein (0.9 +/- 0.3 g/kg/day) were found insufficient in the participants. The overall intake of 12 nutrients appeared to be also inadequate (0.66 +/- 0.15), but INQs of overall nutrients, except for folate (0.6) and calcium (0.8), were found relatively adequate (INQ > or = 1). As a result of diet quality assessment using DQI-I, dietary imbalance and inadequacy were found to be the most problematic in hemodialysis patients. This study suggests that the main reason for insufficient intake of essential nutrients is insufficient calorie intake. Hemodialysis patients should be encouraged to use various food sources to meet their energy requirements as well as satisfy overall balance and nutrient adequacy.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Nutritional Status and Dietary Management According to Hemodialysis Duration
Hee-Sook Lim, Hee-Seon Kim, Jin Kuk Kim, Mooyong Park, Soo Jeong Choi
Clin Nutr Res. 2019;8(1):28-35. doi: 10.7762/cnr.2019.8.1.28.
Reference
-
1. Krenitsky J. Nutrition in renal failure: myths and management. Pract Gastroenterol. 2004; 20:40–59.2. Stenvinkel P, Heimbürger O, Lindholm B, Kaysen GA, Bergström J. Are there two types of malnutrition in chronic renal failure? Evidence for relationships between malnutrition, inflammation and atherosclerosis (MIA syndrome). Nephrol Dial Transplant. 2000; 15:953–960.
Article3. Bergström J. Why are dialysis patients malnourished? Am J Kidney Dis. 1995; 26:229–241.
Article4. Fouque D, Kalantar-Zadeh K, Kopple J, Cano N, Chauveau P, Cuppari L, Franch H, Guarnieri G, Ikizler TA, Kaysen G, Lindholm B, Massy Z, Mitch W, Pineda E, Stenvinkel P, Treviño-Becerra A, Wanner C. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008; 73:391–398.
Article5. K/DOQI, National Kidney Foundation. Clinical practice guidelines for nutrition in chronic renal failure. Am J Kidney Dis. 2000; 35:S1–S140.6. Lorenzo V, de Bonis E, Rufino M, Hernández D, Rebollo SG, Rodríguez AP, Torres A. Caloric rather than protein deficiency predominates in stable chronic haemodialysis patients. Nephrol Dial Transplant. 1995; 10:1885–1889.7. Dwyer JT, Cunniff PJ, Maroni BJ, Kopple JD, Burrowes JD, Powers SN, Cockram DB, Chumlea WC, Kusek JW, Makoff R, Goldstein DJ, Paranandi L. The HEMO Study Group. The hemodialysis pilot study: nutrition program and participant characteristics at baseline. J Ren Nutr. 1998; 8:11–20.
Article8. Burrowes JD, Cockram DB, Dwyer JT, Larive B, Paranandi L, Bergen C, Poole D. Cross-sectional relationship between dietary protein and energy intake, nutritional status, functional status, and comorbidity in older versus younger hemodialysis patients. J Ren Nutr. 2002; 12:87–95.
Article9. Locatelli F, Fouque D, Heimburger O, Drüeke TB, Cannata-Andía JB, Hörl WH, Ritz E. Nutritional status in dialysis patients: A European consensus. Nephrol Dial Transplant. 2002; 17:563–572.
Article10. Kim HJ, Kim SA, Sohn CM. Association of the nutritional status and essential amino acids intake in hemodialysis patients. Korean J Nutr. 2006; 39:617–623.11. Kawakami J, Suzuki Y, Sugino N. Evaluation of amino acid patterns in recipes for kidney disease patients. J Ren Nutr. 2003; 13:126–132.
Article12. Kalantar-Zadeh K, Kopple JD, Deepak S, Block D, Block G. Food intake characteristics of hemodialysis patients as obtained by food frequency questionnaire. J Ren Nutr. 2002; 12:17–31.
Article13. Dobell E, Chan M, Williams P, Allman M. Food preferences and food habits of patients with chronic renal failure undergoing dialysis. J Am Diet Assoc. 1993; 93:1129–1135.
Article14. Ohri-Vachaspati P, Sehgal AR. Correlates of poor appetite among hemodialysis patients. J Ren Nutr. 1999; 9:182–185.
Article15. Aguilera A, Codoceo R, Bajo MA, Iglesias P, Diéz JJ, Barril G, Cigarrán S, Alvarez V, Celadilla O, Fernández-Perpén A, Montero A, Selgas R. Eating behavior disorders in uremia: a question of balance in appetite regulation. Semin Dial. 2004; 17:44–52.
Article16. Zimmerer JL, Leon JB, Covinsky KE, Desai U, Sehgal AR. Diet monotony as a correlate of poor nutritional intake among hemodialysis patients. J Ren Nutr. 2003; 13:72–77.
Article17. Burrowes JD, Powers SN, Cockram DB, McLeroy SL, Dwyer JT, Cunniff PJ, Paranandi L, Kusek JW. Use of an appetite and diet assessment tool in the pilot phase of a hemodialysis clinical trial: Mortality and morbidity in hemodialysis study. J Ren Nutr. 1996; 6:229–232.
Article18. Burrowes JD, Larive B, Chertow GM, Cockram DB, Dwyer JT, Greene T, Kusek JW, Leung J, Rocco MV. Hemodialysis (HEMO) Study Group. Self-reported appetite, hospitalization and death in haemodialysis patients: findings from the Hemodialysis (HEMO) Study. Nephrol Dial Transplant. 2005; 20:2765–2774.
Article19. Kalantar-Zadeh K, Block G, McAllister CJ, Humphreys MH, Kopple JD. Appetite and inflammation, nutrition, anemia, and clinical outcome in hemodialysis patients. Am J Clin Nutr. 2004; 80:299–307.
Article20. Masud T. Trave elements and vitamins in renal disease. In : Mitch WE, Klahr S, editors. Handbook of nutrition and the kidney. 4th ed. Philadelphia(PA): Lippincott Williams & Wilkins;2002. p. 233–252.21. Wiggins KL. Guidelines for nutrition care of renal patients. 3rd ed. Chicago(IL): American Dietetic Association;2002.22. The Korean Nutrition Society. Dietary reference intakes for Koreans. Seoul: The Korean Nutrition Society;2005.23. Hatløy A, Torheim LE, Oshaug A. Food variety--a good indicator of nutritional adequacy of the diet? A case study from an urban area in Mali, West Africa. Eur J Clin Nutr. 1998; 52:891–898.
Article24. Guthrie HA, Scheer JC. Validity of a dietary score for assessing nutrient adequacy. J Am Diet Assoc. 1981; 78:240–245.
Article25. Ries CP, Daehler JL. Evaluation of the Nutrient Guide as a dietary assessment tool. J Am Diet Assoc. 1986; 86:228–233.
Article26. Coles GA, Peters DK, Jones JH. Albumin metabolism in chronic renal failure. Clin Sci. 1970; 39:423–435.
Article27. Hansen RG, Wyse BW. Expression of nutrient allowances per 1,000 kilocalories. J Am Diet Assoc. 1980; 76:223–227.
Article28. Kim S, Haines PS, Siega-Riz AM, Popkin BM. The Diet Quality Index-International (DQI-I) provides an effective tool for cross-national comparison of diet quality as illustrated by China and the United States. J Nutr. 2003; 133:3476–3484.
Article29. Bergström J. Nutrition and mortality in hemodialysis. J Am Soc Nephrol. 1995; 6:1329–1341.
Article30. Marcén R, Teruel JL, de la Cal MA, Gámez C. The impact of malnutrition in morbidity and mortality in stable haemodialysis patients. Spanish Cooperative Study of Nutrition in Hemodialysis. Nephrol Dial Transplant. 1997; 12:2324–2331.31. Facchini F, Schoenfeld P, Dixon B, Giambra G, Coulston A. ESRD patients consume an atherogenic diet. J Am Soc Nephrol. 1997; 7:S133.32. Block G, Mangels AR, Norkus EP, Patterson BH, Levander OA, Taylor PR. Ascorbic acid status and subsequent diastolic and systolic blood pressure. Hypertension. 2001; 37:261–267.
Article33. Clermont G, Lecour S, Lahet J, Siohan P, Vergely C, Chevet D, Rifle G, Rochette L. Alteration in plasma antioxidant capacities in chronic renal failure and hemodialysis patients: a possible explanation for the increased cardiovascular risk in these patients. Cardiovasc Res. 2000; 47:618–623.
Article34. Reid DJ, Barr SI, Leichter J. Effects of folate and zinc supplementation on patients undergoing chronic hemodialysis. J Am Diet Assoc. 1992; 92:574–579.
Article35. Agarwal S, Rao AV. Carotenoids and chronic diseases. Drug Metabol Drug Interact. 2000; 17:189–210.
Article36. Rissanen T, Voutilainen S, Nyyssönen K, Salonen R, Salonen JT. Low plasma lycopene concentration is associated with increased intima-media thickness of the carotid artery wall. Arterioscler Thromb Vasc Biol. 2000; 20:2677–2681.
Article37. Lim PS, Chan EC, Lu TC, Yu YL, Kuo SY, Wang TH, Wei YH. Lipophilic antioxidants and iron status in ESRD patients on hemodialysis. Nephron. 2000; 86:428–435.
Article38. Carrero JJ, Qureshi AR, Axelsson J, Avesani CM, Suliman ME, Kato S, Bárány P, Snaedal-Jonsdottir S, Alvestrand A, Heimbürger O, Lindholm B, Stenvinkel P. Comparison of nutritional and inflammatory markers in dialysis patients with reduced appetite. Am J Clin Nutr. 2007; 85:695–701.
Article39. Ikizler TA. Protein and energy intake in advanced chronic kidney disease: how much is too much? Semin Dial. 2007; 20:5–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quality of Diet and Nutritional Intake and Mortality Risk among South Korean Adults Based on 12-year Follow-up Data
- Evaluation of dietary intake in Korean adults according to energy intake from eating-out: Based on 2013~2014 Korea National Health and Nutrition Examination Survey
- Diabetes and Dietary Fats
- Evaluation of Diet Quality Determined by Dietary Patterns of Elderly Koreans Living Alone: Data Retrieved from the 2016∼2018 Korea National Health and Nutrition Examination Survey
- Accuracy of 24-hour Diet Recalls for Estimating Energy Intake in Elderly Men using the Doubly Labeled Water Method