Chonnam Med J.
2008 Aug;44(2):65-71. 10.4068/cmj.2008.44.2.65.
Usefulness of Plasma Von Willebrand Factor and Brachial Artery Endothelial Dysfunction to Predict Variant Angina
- Affiliations
-
- 1The Heart Center of Chonnam National University Hospital, Gwangju, Korea. myungho@chollian.net
- 2College of Nursing of Chonnam National University, Gwangju, Korea.
- 3Cardiovascular Research Institute of Chonnam National University, Gwangju, Korea
- KMID: 2045752
- DOI: http://doi.org/10.4068/cmj.2008.44.2.65
Abstract
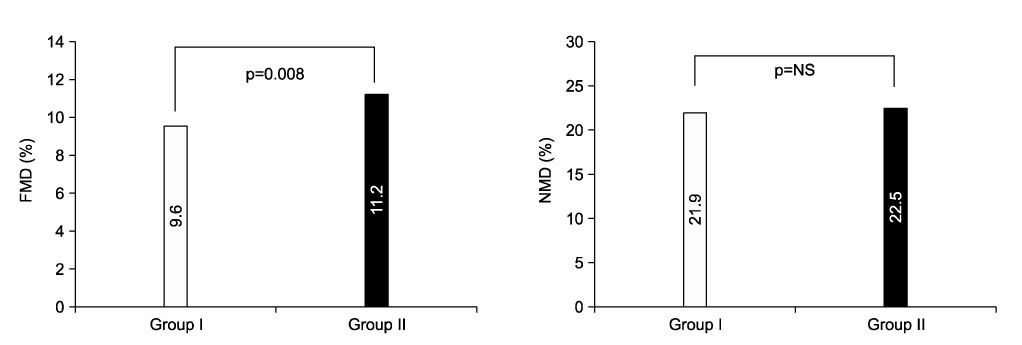
- Endothelial dysfunction and vascular inflammation may be associated with variant angina (VA). The aim of the present study was to investigate whether the level of von Willebrand factor (VWF) and flow-mediated dilation (FMD) are related to VA. This study included 74 patients (VA group: 52.1+/-11.9 years, 40 males) with normal coronary angiogram (CAG) and positive ergonovine provocation test (ERT), and 33 patients (control group:49.7+/-10.8 years, 23 males) and normal CAG with negative ERT. The level of VWF was significantly higher in VA than in control group (163.0+/-43.4% vs. 127.2+/-59.6%, p=0.008). FMD was significantly decreased in VA group compared with control group (9.0+/-4.0% vs. 11.2+/-3.1%, p=0.008). The levels of white blood cell counts was higher in VA than in control group (7509.4+/-2411.1/mm3 vs. 6303.1+/-2027.1/mm3, p=0.015). The level of total cholesterol was significantly higher in VA group compared with the control group (185.2+/-45.3 mg/dL vs.166.2+/-36.9 mg/dL, p=0.042). In multiple regression analysis, the VWF [odds ratio (OR), 11.14, 95% confidence interval (CI), 3.25-38.15: p<0.001) and FMD (OR, 4.42, 95% CI, 1.32-14.82: p=0.016)] were predictors of VA. On the basis of the receiver-operating characteristics analysis, the cutoff value of VWF > 140% and FMD <10% provided the best separation of patients with and without VA (sensitivity 0.73, 0.66; specificity 0.78, 0.69, respectively). The increased level of VWF and decreased FMD are independently associated with VA. Non-invasive evaluation of VWF and FMD may serve as useful markers for detecting endothelial dysfunction and screening the VA patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Kang JA, Lee YS, Jeong SH, Lee JW, Kim BY, Im DS, et al. Clinical characteristics of patients with variant angina. Korean J Med. 2002. 63:195–202.2. Beltrame JF, Sasayama S, Maseri A. Racial heterogeneity in coronary artery vasomo-tor reactiviety: differences between Japanese and Caucasian patients. J Am CollCardiol. 1999. 33:1442–1452.
Article3. Bertrand ME, LaBlanche JM, Tilmant PY, Thieuleux FA, Delforge MR, Carre AG, et al. Frequency of provoked coronary arterial spasm in 1089 consecutive patients undergoing coronary angiography. Circulation. 1982. 65:1299–1306.
Article4. Pristipino C, Beltrame JF, Finocchiaro ML, Hattori R, Fujita M, Mongiardo R, et al. Major racial differences in coronary constrictor response between Japanese and Caucasians with recent myocardial infarction. Circulation. 2000. 101:1102–1108.
Article5. Selwyn AP, Kinlay S, Creager M, Libby P, Ganz P. Cell dysfunction in atherosclerosis and the ischemic manifestations of coronary artery disease. Am J Cardiol. 1997. 79:17–23.
Article6. Grundy SM, Pasternak R, Greenland P, Smith S Jr, Fuster V. Assessment of cardiovascular risk by use of multiple-risk-factor assessment equations: a statement for health care professionals from the American Heart Association and the American College of Cardiology. Circulation. 1999. 100:1481–1492.
Article7. Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial ArteryReactivity Task Force. J Am Coll Cardiol. 2002. 39:257–265.
Article8. Patel SN, Rajaram V, Pandya S, Fiedler BM, Bai CJ, Neems R, et al. Emerging, noninvasive surrogate markers of atherosclerosis. Curr Atheroscler Rep. 2004. 6:60–68.
Article9. Kugiyama T, Motoyama T, Hirashima O, Ohgushi M, Soejima H, Misumi K, et al. Vitamin C attenuates abnormal vasomotor reactivity in spasm coronary arteries inpatients with coronary spastic angina. J Am Coll Cardiol. 1998. 32:103–109.
Article10. Motoyama T, Kawano H, Kugiyama K, Okumura K, Ohgushi M, Yoshimura M, et al. Flow-mediated, endothelium-dependent dilation of the brachial arteries is impaired inpatients with coronary spastic angina. Am Heart J. 1997. 133:263–267.
Article11. Kawano H, Ogawa H. Endothelial function and coronary spastic angina. Internal Med. 2005. 44:91–99.
Article12. Kugiyama K, Yasue H, Okumura K, Ogawa H, Fujimoto K, Nakao K, et al. Nitric oxide activity is deficient in spasm arteries of patients with coronary spastic angina. Circulation. 1996. 94:266–271.
Article13. Kugiyama K, Ohgushi M, Motoyama T, Sugiyama S, Ogawa H, Yoshimura M, et al. Nitric oxide-mediated flow-dependent dilation is impaired in coronary arteries inpatients with coronary spastic angina. J Am Coll Cardiol. 1997. 30:920–926.
Article14. Hung MJ, Cherng WJ, Yang NI, Cheng CW, Li LF. Relation of high-sensitivity C-reactive protein level with coronary vasospastic angina pectoris in patients without hemodynamically significant coronary artery disease. Am J Cardiol. 2005. 96:1484–1490.
Article15. Miyao Y, Kugiyama K, Kawano H, Motoyama T, Ogawa H, Yoshimura M, et al. Diffuse intimal thickening of coronary arteries in patients with coronary spastic angina. J Am Coll Cardiol. 2000. 36:432–437.
Article16. Suzuki H, Kawai S, Aizawa T, Kato K, Sunayama S, Okada R, et al. Histologicevalution of coronary plaque in patients with variant angina: relationship betweenvasospasm and neointimal hyperplasia in premary coronary lesions. J Am Coll Cardiol. 1999. 33:198–205.
Article17. Hung MJ, Cherng WJ, Cheng CW, Li LF. Comparison of serum levels of inflammatory markers in patients with coronary vasospasm without significant fixed coronary artery disease versus patients with stable angina pectoris and acute coronary syndromes with significant fixed coronary artery disease. Am J Cardiol. 2006. 97:1429–1434.
Article18. Maseri A, Severi S, Nes MD, L'Abbate A, Chierchia S, Marzilli M, et al. "Variant" angina: one aspect of a continuous spectrum of vasospastic myocardial ischemia. Pathologenetic mechanisms, estimated incidence and clinical and coronaryarteriographic findings in 138 patients. Am J Cardiol. 1978. 42:1019–1035.
Article19. Teragawa H, Kato M, Kurokawa J, Yamagata T, Matsuura H, Chayama K. Endothelial dysfunction in an independent factor responsible for vasospastic angina . Clin Sci (Lond). 2001. 101:707–713.
Article20. Vita JA, Treasure CB, Nabel EG, McLenachan JM, Fish RD, Yeung AC, et al. Coronary vasomotor response to acetylcholine relates to risk factors for coronary artery disease. Circulation. 1990. 81:491–497.
Article21. Saito S, Yamagishi M, Takayama T, Chiku M, Koyama J, Ito K, et al. Plaquemorphology at coronary sites with focal spasm in variant angina: study using intravascular ultrasound. Circ J. 2003. 67:1041–1045.
Article22. Yazici M, Demircan S, Durna K, Yasar E, Sahin M. Relationship between myocardialinjury and soluble P-selectin in non-ST elevation acute coronary syndromes. Circ J. 2005. 69:530–505.
Article23. Tanis B, Algra A, Van der Graaf Y, Helmerhorst F, Rosendaal F. Procoagulationfactors and the risk of myocardial infarction in young women. Eur J Haematol. 2006. 77:67–73.
Article24. Cho SH, Park IH, Jeong MH, Hwang SH, Yun NS, Hong SN, et al. Increased inflama-tory markers and endothelial dysfunction are associated with variant angina. Korean Circ J. 2007. 37:27–32.
Article25. Ogawa H, Yashe H, Oshima S, Okumura K, Matsuyama K, Obata K. Circadianvariation of plasma fibrinopeptide. A level in patientss with variant angina. Circulation. 1989. 80:1617–1626.
Article26. Vita JA, Keaney JF Jr. Exercise-toning up the endothelium? N Engl J Med. 2000. 342:503–505.27. Yamagishi M, Ito K, Tsutsui H, Miyazaki S, Goto Y, Nagaya N, et al. Lesion severity and hypercholesterolemia determine long-term prognosis of vasospastic angina treated with calcium channel antagonists. Circ J. 2003. 67:1029–1035.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laboratory assessment of von Willebrand factor for classification of von Willebrand disease
- Effect of immune-mediated vascular injury on the coagulation- regulatory mechanism of the human endothelial cells; changes of tissue-type plasminogen activator, plasminogen activator inhibitor- 1 and von Willebrand factor
- Cardiovascular Risk Factors Predicting Endothelial Dysfunction in Patients with Variant Angina
- Three cases of type I von Willebrand disease in a family
- Recombinant von Willebrand Factor for Pediatric Patient with von Willebrand Disease: First Report in Korea