Infect Chemother.
2012 Aug;44(4):263-268. 10.3947/ic.2012.44.4.263.
The History of Antimicrobial Drug Development and the Current Situation
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. imfell@yuhs.acr
- KMID: 2045545
- DOI: http://doi.org/10.3947/ic.2012.44.4.263
Abstract
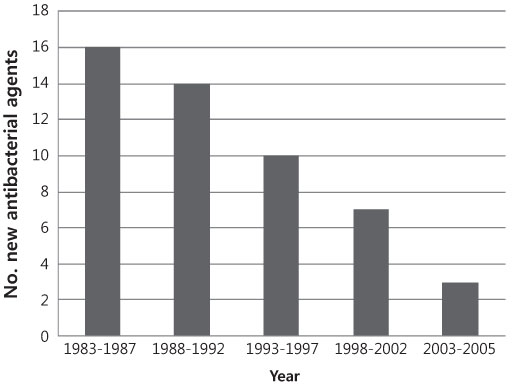
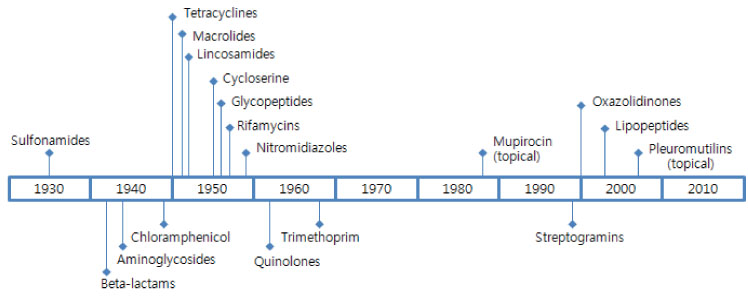
- Since development of the first antimicrobial agents in the 1940s, antimicrobial resistance has been an issue. Following the introduction of sulfonamides and penicillin, scientists discovered and developed a wide range of antimicrobials for treatment of bacterial diseases. Many new antimicrobials were discovered by systematic testing of soil microbes and many others were developed by chemical modification of existing agents. Discovery of new classes of antibacterial drugs slowed in the late 1960s. However, the speed with which bacteria develop resistance to antibiotics, in contrast with the slow development of new drugs, has led some experts to warn of a "post-antibiotic era." Judicious use of currently available antibiotics, through efforts such as public campaigns for 'appropriate antibiotic use', may help to conserve their effectiveness. However, even if we improve these practices, development of resistant bacteria will continue to occur, and new and better drugs will be needed. Clearly, a combination of traditional successful methods and modern technology will be needed for discovery and development of new classes of antibacterial drugs. In addition, policies that encourage and facilitate development of new antimicrobial agents are also needed.
MeSH Terms
Figure
Reference
-
1. Wenzel RP. The antibiotic pipeline - challenges, costs, and values. N Engl J Med. 2004. 351:523–526.
Article2. Skinner D, Keefer CS. Significance of bacteremia caused by Staphlyococcus aureus. Arch Intern Med. 1941. 68:851–875.3. Alanis AJ. Resistance to antibiotics: are we in the post-antibiotic era? Arch Med Res. 2005. 36:697–705.
Article4. Falagas ME, Bliziotis IA. Pandrug-resistant Gram-negative bacteria: the dawn of the post-antibiotic era? Int J Antimicrob Agents. 2007. 29:630–636.
Article5. Outterson K, Samora JB, Keller-Cuda K. Will longer antimicrobial patents improve global public health? Lancet Infect Dis. 2007. 7:559–566.
Article6. Talbot GH, Bradley J, Edwards JE Jr, Gilbert D, Scheld M, Bartlett JG. Bad bugs need drugs: an update on the development pipeline from the Antimicrobial Availability Task Force of the Infectious Diseases Society of America. Clin Infect Dis. 2006. 42:657–668.
Article7. Diekema DJ, BootsMiller BJ, Vaughn TE, Woolson RF, Yankey JW, Ernst EJ, Flach SD, Ward MM, Franciscus CLJ, Pfaller MA, Doebbeling BN. Antimicrobial resistance trends and outbreak frequency in United States hospitals. Clin Infect Dis. 2004. 38:78–85.
Article8. Spellberg B, Powers JH, Brass EP, Miller LG, Edwards JE Jr. Trends in antimicrobial drug development: implications for the future. Clin Infect Dis. 2004. 38:1279–1286.
Article9. Boucher HW, Talbot GH, Bradley JS, Edwards JE, Gilbert D, Rice LB, Scheld M, Spellberg B, Bartlett J. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis. 2009. 48:1–12.
Article10. DiMasi JA, Hansen RW, Grabowski HG. The price of innovation: new estimates of drug development costs. J Health Econ. 2003. 22:151–185.
Article11. Projan SJ. Why is big pharma getting out of antibacterial drug discovery? Curr Opin Microbiol. 2003. 6:427–430.
Article12. Powers JH. Development of drugs for antimicrobial-resistant pathogens. Curr Opin Infect Dis. 2003. 16:547–551.
Article13. Norrby SR, Nord CE, Finch R. European Society of Clinical Microbiology and Infectious Diseases. Lack of development of new antimicrobial drugs: a potential serious threat to public health. Lancet Infect Dis. 2005. 5:115–119.
Article14. Wenzel RP, Edmond MB. Managing antibiotic resistance. N Engl J Med. 2000. 343:1961–1963.
Article15. Hoel D, Williams DN. Antibiotics: past, present, and future. Unearthing nature's magic bullets. Postgrad Med. 1997. 101:114–118. 121–122.16. Lloyd NC, Morgan HW, Nicholson BK, Ronimus RS. The composition of Ehrlich's Salvarsan: Resolution of a century-old debate. Angew Chem Int Ed Engl. 2005. 44:941–944.
Article17. Lesch JE. Lesch JE, editor. Prontosil. The first miracle drugs: how the sulfa drugs transformed medicine. 2007. Oxford University Press;51.18. Schwentker FF, Gelman S, Long PH. The treatment of meningococcic meningitis. JAMA. 1937. 108:1407–1408.19. Powers JH. Antimicrobial drug development-the past, the present, and the future. Clin Microbiol Infect. 2004. 10:Suppl 4. 23–31.20. Fleming A. The antibacterial action of cultures of a Penicillium, with special reference to their use in the isolation of B. influenzae. Br J Exp Pathol. 1929. 10:226–236.21. Levy SB. Levy SB, editor. From tragedy the antibiotic era is born. The Antibiotic Paradox; How the misuse of antibiotics destroys their curative powers. 2002. 2nd ed. Cambridge, MA: Perseus Publishing;1–14.23. Lewis K. Recover the lost art of drug discovery. Nature. 2012. 485:439–440.
Article24. Fernandes P. Antibacterial discovery and development- the failure of success? Nat Biotechnol. 2006. 24:1497–1503.
Article25. Clatworthy AE, Pierson E, Hung DT. Targeting virulence: a new paradigm for antimicrobial therapy. Nat Chem Biol. 2007. 3:541–548.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Strategies to combat Gram-negative bacterial resistance to conventional antibacterial drugs: a review
- Pharmacokinetics/Pharmacodynamics models of veterinary antimicrobial agents
- Current status and future strategies of antimicrobial resistance in Korea
- Antimicrobial Resistance in Asia: Current Epidemiology and Clinical Implications
- New antimicrobials on the horizon