J Korean Neurosurg Soc.
2014 Nov;56(5):431-435. 10.3340/jkns.2014.56.5.431.
Total En Bloc Thoracic and Lumbar Spondylectomy for Non-Small Cell Lung Cancer with Favorable Prognostic Indicators: Is It Merely Indicated for Solitary Spinal Metastasis?
- Affiliations
-
- 1Department of Neurosurgery, Spine Center, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. neurospine@snubh.org
- KMID: 2018104
- DOI: http://doi.org/10.3340/jkns.2014.56.5.431
Abstract
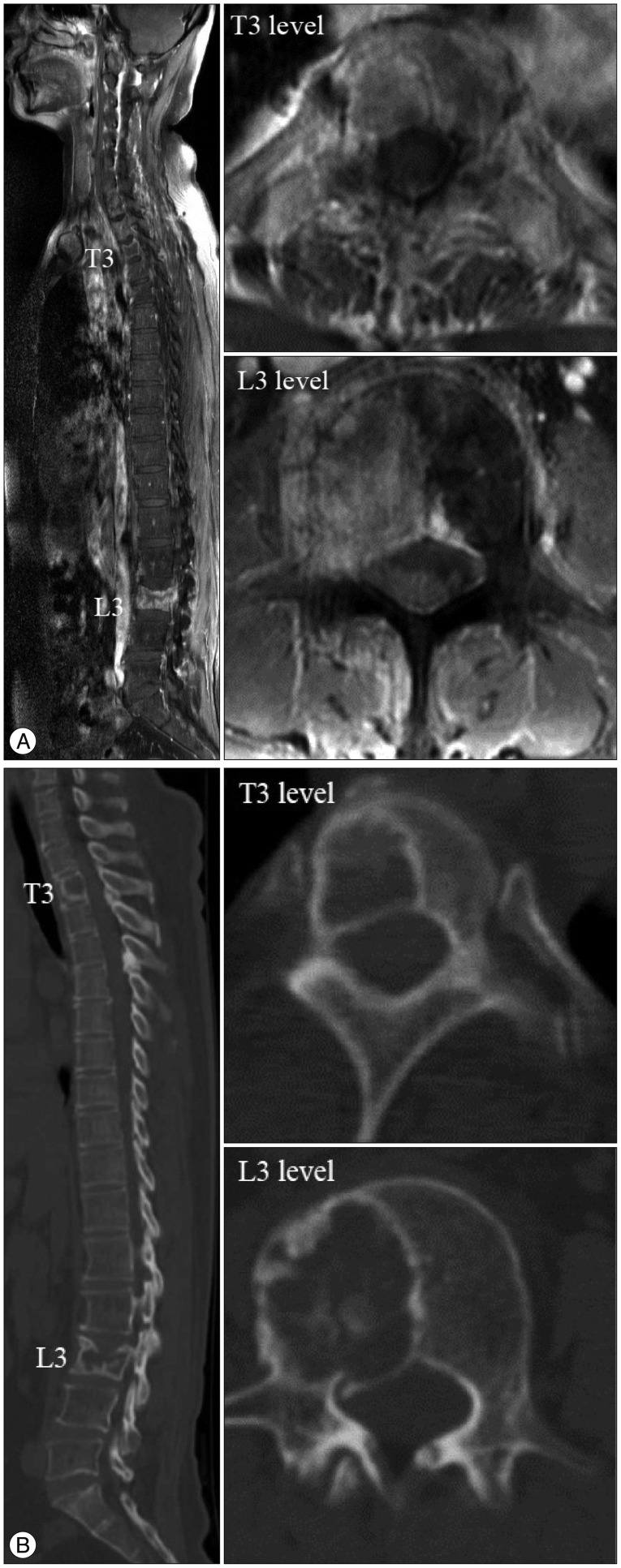
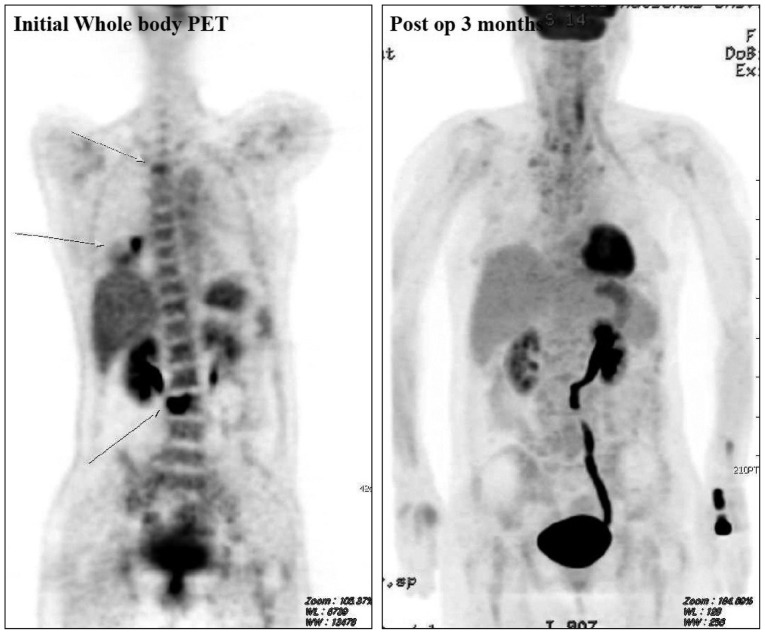
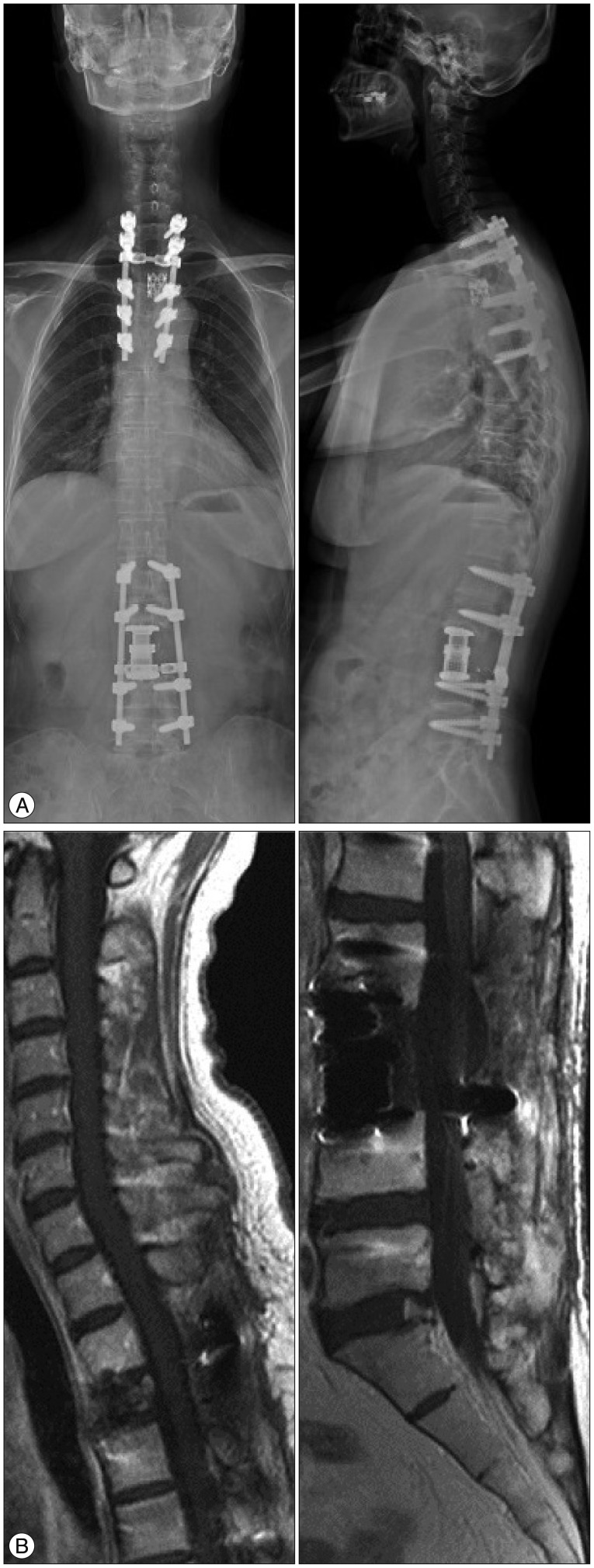
- A fifty-year-old female non-smoker with no other specific medical history visited our institute. She complained of axial back pain with no other neurological deficit. Chest X-ray, chest computed tomography (CT) scan, CT-guided needle aspiration biopsy, whole-body positron emission tomography, spine CT and spine magnetic resonance image findings suggested NSCLC with epidermal growth factor receptor (EGFR) mutation, multiple brain metastases, and two isolated metastases to the T3 and L3 vertebral bodies. She underwent chemotherapy with gefitinib (Iressa(TM)) for NSCLC and gamma knife surgery for multiple brain metastases. We performed a two-staged, total en bloc spondylectomy of the T3 and L3 vertebral bodies based on several good prognostic characteristics, such as the lack of metastases to the appendicular bone, good preoperative performance status, and being an excellent responder (Asian, never-smoker and adenocarcinoma histology) to EGFR inhibitors. Improved axial back pain after the surgery enabled her to walk with the aid of a thoracolumbosacral orthosis brace on the third postoperative day. Her Karnofsky performance status score (KPS) was 90 at the time of discharge and has been maintained to date 3 years after surgery. In selected NSCLC patients with good prognostic characteristics, we suggest that locally curative treatment such as total en bloc spondylectomy or radiosurgery should be emphasized to achieve longer term survival for the selected cases.
MeSH Terms
-
Adenocarcinoma
Back Pain
Biopsy, Needle
Braces
Brain
Carcinoma, Non-Small-Cell Lung*
Drug Therapy
Female
Humans
Karnofsky Performance Status
Lung Neoplasms
Needles
Neoplasm Metastasis*
Orthotic Devices
Positron-Emission Tomography
Radiosurgery
Receptor, Epidermal Growth Factor
Spine
Thorax
Receptor, Epidermal Growth Factor
Figure
Cited by 1 articles
-
Surgical Impacts of Metastatic Non-small Cell Lung Cancer to the Thoracic and Lumbar Spine
Jong-myung Jung, Seung-Jae Hyun, Ki-Jeong Kim
J Korean Med Sci. 2021;36(7):e52. doi: 10.3346/jkms.2021.36.e52.
Reference
-
1. Aoude AA, Amiot LP. Surgical treatment of a patient with lung cancer metastasized to the spine with EGFR mutation : a case report. Int J Surg Case Rep. 2012; 3:510–512. PMID: 22858793.
Article2. Brown T, Boland A, Bagust A, Oyee J, Hockenhull J, Dundar Y, et al. Gefitinib for the first-line treatment of locally advanced or metastatic non-small cell lung cancer. Health Technol Assess. 2010; 14(Suppl 2):71–79. PMID: 21047494.
Article3. Herbst RS, Maddox AM, Rothenberg ML, Small EJ, Rubin EH, Baselga J, et al. Selective oral epidermal growth factor receptor tyrosine kinase inhibitor ZD1839 is generally well-tolerated and has activity in non-small-cell lung cancer and other solid tumors : results of a phase I trial. J Clin Oncol. 2002; 20:3815–3825. PMID: 12228201.
Article4. Hsieh PC, Li KW, Sciubba DM, Suk I, Wolinsky JP, Gokaslan ZL. Posterior-only approach for total en bloc spondylectomy for malignant primary spinal neoplasms : anatomic considerations and operative nuances. Neurosurgery. 2009; 65(6 Suppl):173–181. discussion 181. PMID: 19934992.5. Ibrahim A, Crockard A, Antonietti P, Boriani S, Bünger C, Gasbarrini A, et al. Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? An international multicenter prospective observational study of 223 patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral NervesNerves, March 2007. J Neurosurg Spine. 2008; 8:271–278. PMID: 18312079.
Article6. Komagata M, Nishiyama M, Imakiire A, Kato H. Total spondylectomy for en bloc resection of lung cancer invading the chest wall and thoracic spine. Case report. J Neurosurg. 2004; 100(4 Suppl Spine):353–357. PMID: 15070143.
Article7. Mitsudomi T, Kosaka T, Endoh H, Horio Y, Hida T, Mori S, et al. Mutations of the epidermal growth factor receptor gene predict prolonged survival after gefitinib treatment in patients with non-small-cell lung cancer with postoperative recurrence. J Clin Oncol. 2005; 23:2513–2520. PMID: 15738541.
Article8. Mountain CF. Revisions in the International System for Staging Lung Cancer. Chest. 1997; 111:1710–1717. PMID: 9187198.
Article9. Murakami H, Kawahara N, Demura S, Kato S, Yoshioka K, Tomita K. Total en bloc spondylectomy for lung cancer metastasis to the spine. J Neurosurg Spine. 2010; 13:414–417. PMID: 20887137.
Article10. Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, Gabriel S, et al. EGFR mutations in lung cancer : correlation with clinical response to gefitinib therapy. Science. 2004; 304:1497–1500. PMID: 15118125.
Article11. Sanford M, Scott LJ. Gefitinib : a review of its use in the treatment of locally advanced/metastatic non-small cell lung cancer. Drugs. 2009; 69:2303–2328. PMID: 19852530.12. Schirren J, Dönges T, Melzer M, Schönmayr R, Eberlein M, Bölükbas S. En bloc resection of non-small-cell lung cancer invading the spine. Eur J Cardiothorac Surg. 2011; 40:647–654. PMID: 21334220.
Article13. Sugiura H, Yamada K, Sugiura T, Hida T, Mitsudomi T. Predictors of survival in patients with bone metastasis of lung cancer. Clin Orthop Relat Res. 2008; 466:729–736. PMID: 18196360.
Article14. Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976). 2001; 26:298–306. PMID: 11224867.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Total Body Replacement with an Expandable Cage after en Bloc Lumbar Spondylectomy
- Total en bloc Spondylectomy for Solitary Metastatic Spinal Tumor
- Surgical Impacts of Metastatic Nonsmall Cell Lung Cancer to the Thoracic and Lumbar Spine
- Combined en Bloc Spondylectomy and Chest Wall Resection for Malignant Tumors Invading Spinal Column and Chest Wall
- Total En Bloc Lumbar Spondylectomy of Follicular Thyroid Carcinoma