J Korean Soc Magn Reson Med.
2011 Aug;15(2):123-129. 10.13104/jksmrm.2011.15.2.123.
Follow-Up MR Imaging Assessment of Natural History of Lumbar Disc Herniation in Patients with Recurred Low Back Pain
- Affiliations
-
- 1Department of Radiology, Kyung Hee University Hospital, Kyung Hee University, Korea. gdluck@hitel.net
- 2Department of Radiology, Kyung Hee University Hospital at Gangdong, Kyung Hee University, Korea.
- KMID: 2000060
- DOI: http://doi.org/10.13104/jksmrm.2011.15.2.123
Abstract
- PURPOSE
To compare lumbar disc changes between initial lumbar spine (L-spine) MRI and follow-up (f/u) MRI that were performed due to recurred backaches.
MATERIALS AND METHODS
A total 50 patients who had undergone f/u L-spine MRI were retrospectively reviewed. Five discs (L1-S1) were surveyed in each f/u MRI. Lumbar disc changes were defined as no change, aggravations, or improvements compared to initial disc states. These states were defined on the basis of morphologic status and disc levels.
RESULTS
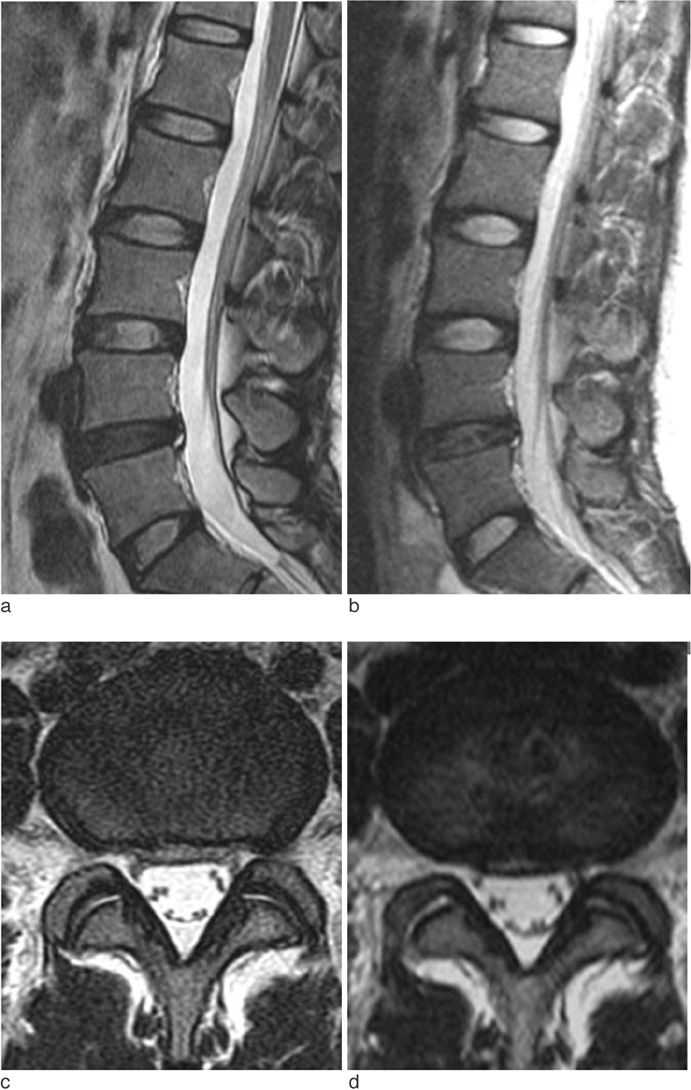
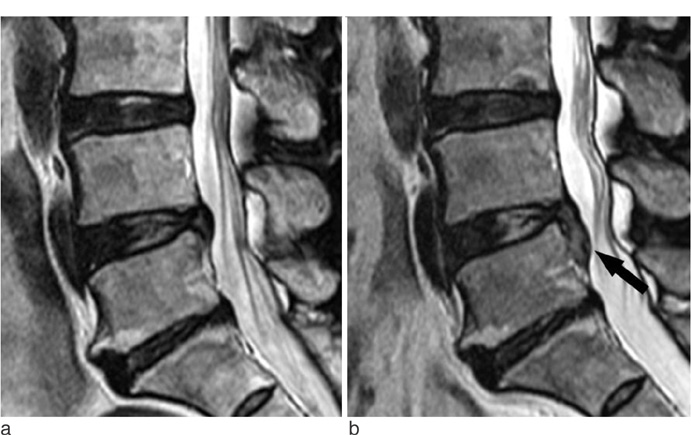
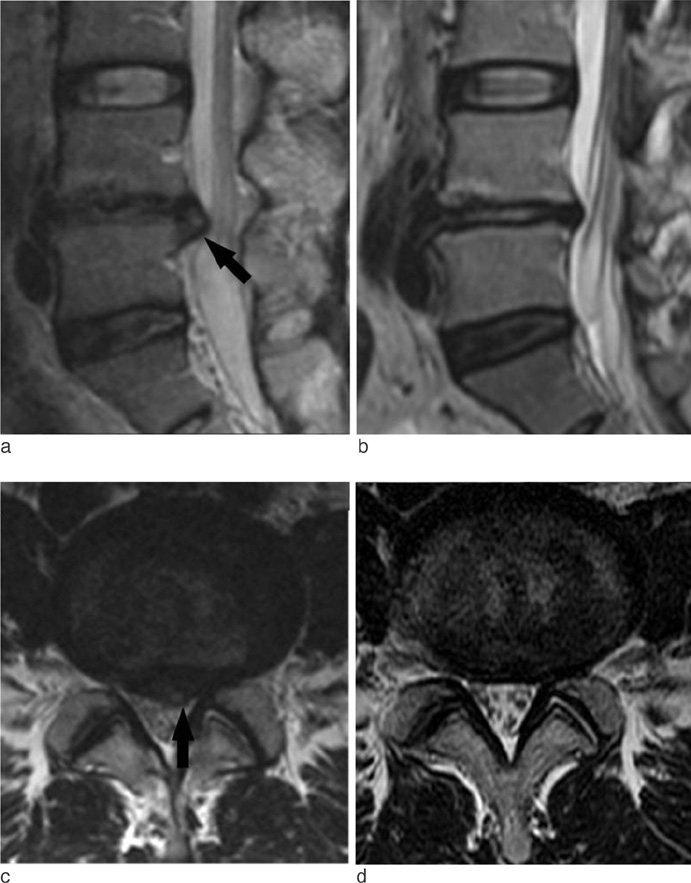
In a total of 250 discs in 50 patients, 31 discs (12.4%) showed morphologic changes of disc lesions, whereas 219 discs (87.6 %) showed no changes. Among the 31 disc lesions, 24 were aggravated and 7 were partially improved. And on the basis of disc status, initially abnormal discs revealed any morphologic changes of the degree of disc herniation. A total of 33.3% of the morphologic changes are noted in initially extruded discs. Fifteen morphologic changes of disc lesions were located at the L4-5 level.
CONCLUSION
Our results suggest that correlations between lumbar disc herniations and back pain symptoms are limited, and that evaluations of extra disc lesions are required.
MeSH Terms
Figure
Reference
-
1. Saal JA, Saal JS, Herzog RJ. The natural history of lumbar intervertebral disc extrusions treated nonoperatively. Spine. 1990. 15:683–686.2. Bozzao A, Gallucci M, Masciocchi C, Aprile I, Barile A, Passariello R. Lumbar disc herniation : MR imaging assessment of natural history in patients treated without surgery. Radiology. 1992. 185:135–141.3. Komori H, Shinomiya K, Nakai O, Yamaura I, Takeda S, Furuya K. The natural history of herniated nucleus pulposus with radiculopathy. Spine. 1996. 21:225–229.4. Fardon DF, Milette PC. Nomenclature and classification of lumbar disc pathology. Recommendations of the combined task forces of the North American Spine Society, American Society of Spine Radioloty, and American Society of Neuroradiology. Spine. 2001. 26:E93–E113.5. Autio RA, Karppinen J, Niinimaki J, Ojala R, Kurunlahti M, Haapea M. Determinants of spontaneous resorption of intervertebral disc herniations. Spine. 2006. 31:1247–1252.6. Weber H. Lumbar disc herniation: a controlled, prospective study with ten years of observation. Spine. 1983. 8:131–140.7. Ryu SJ, Kim IS. Spontaneous regression of a large lumbar disc extrusion. J Korean Neurosurg Soc. 2010. 48:285–287.8. Teplick JG, Haskin ME. Spontaneous regression of herniated nucleus pulposus. AJR Am J Roentgenol. 1985. 145:371–375.9. Slavin KV, Raja A, Thornton J, Wagner FC Jr. Spontaneous regression of a large lumbar disc herniation: report of an illustrative case. Surg Neurol. 2001. 56:333–336.10. Lee HM. Pathophysiology of degenerative disease of the lumbar spine. J Korean Soc Spine Surg. 1999. 6:201–207.11. Minamide A, Hashizume H, Yoshida M, Kawakami M, Hayashi N, Tamaki T. Effect of basic fibroblast growth factor on spontaneous resorption of herniated intervertebral discs: an experimental study in the rabbit. Spine. 1999. 24:940–945.12. McCarron RF, Wimpee MW, Hudgins PG, Laros GS. The inflammatory effect of nucleus pulposus: a possible element in the pathogenesis of low back pain. Spine. 1987. 12:760–764.13. Lindahl O, Rexed B. Histologic changes in spinal nerve roots of operated cases of sciatica. Acta Orthop Scand. 1951. 20:215–225.14. Masui T, Yasutsugu Y, Nakamura S, et al. Natural history of patients with lumbar disc herniation observed by magnetic resonance imaging for minimum 7 years. J Spinal Disord Tech. 2005. 18:121–126.15. Matsubara Y, Kato F, Mimatsu K, Kajino G, Nakamura S, Nitta H. Serial changes on MRI in lumbar disc herniations treated conservatively. Neuroradiology. 1995. 37:378–383.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Natural History and Clinical Manifestations of Lumbar Disc Herniation
- Lumbar Disc Screening Using Back Pain Questionnaires: Oswestry Low Back Pain Score, Aberdeen Low Back Pain Scale, and Acute Low Back Pain Screening Questionnaire
- The Relationship between Lumbar Shape and Lumbar Disc Herniation
- Spinal Nerve Root Swelling Mimicking Intervertebral Disc Herniation in Magnetic Resonance Imaging: A Case Report
- Classification and Imaging Study of the Lumbar Disc Herniation