Korean J Hepatobiliary Pancreat Surg.
2011 May;15(2):90-100. 10.14701/kjhbps.2011.15.2.90.
Outcome of Hepatectomy for Huge Hepatocellular Carcinoma
- Affiliations
-
- 1Department of Surgery, Dankook University College of Medicine, Korea. agapejsh@dankook.ac.kr
- KMID: 1980947
- DOI: http://doi.org/10.14701/kjhbps.2011.15.2.90
Abstract
- PURPOSE
In spite of the recent improved results of hepatectomy for huge hepatocellular carcinomas (HCC), the prognosis of patients with huge HCCs is still poor compared to that of patients with small HCCs. This study was performed to compare the results of hepatectomy between patients with huge HCCs and those with small HCCs, to identify the prognostic factors in patients with huge HCCs, and to determine the preoperative selection criteria.
METHODS
We retrospectively analyzed 51 patients who underwent hepatectomy, between July 1994 and February 2009 at Dankook University Hospital. Patients with HCC> or =10 cm were classified in large (L) group and others were classified in small (S) group. The clinicopathological features, operative procedures, and postoperative outcome were compared between both groups and various prognostic factors were investigated in group L.
RESULTS
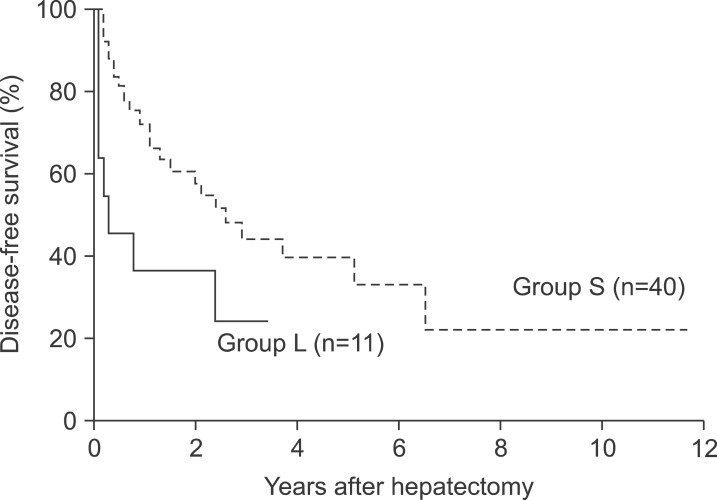
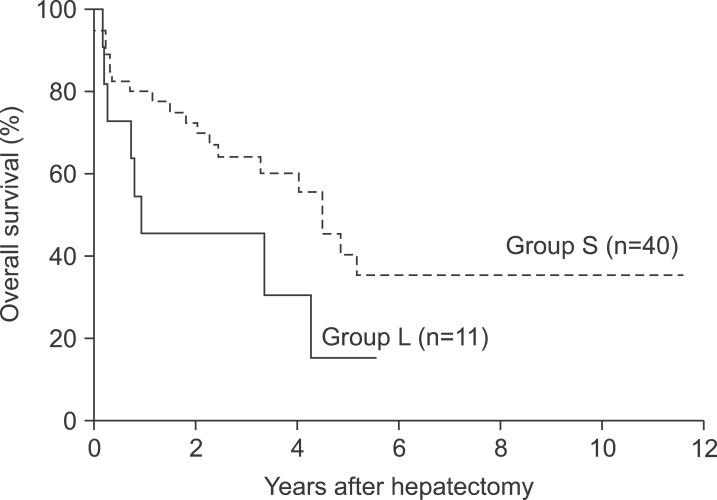
Eleven patients were classified in group L. Tumor size, vascular invasion, and tumor stage were higher in group L. Postoperative morbidity was higher in group L, but mortality was not different between the groups. Disease-free survivals were significantly lower in group L than in group S (36.4%, and 24.2% vs. 72.0%, and 44.0% for 1- and 3-year), but overall survival rates were similar in both groups (45.5%, and 15.2% in group L vs. 60.3%, and 41.3% in group S for 3- and 5-year). Presence of satellite nodules was the only prognostic factor in multivariate analysis after surgery for huge HCC.
CONCLUSION
Regardless of tumor size, huge HCCs deserve consideration for surgery in patients with preserved liver function. Furthermore, the effect of surgery could be maximized with appropriate selection criteria, such as huge HCC without satellite nodules.
Keyword
MeSH Terms
Figure
Reference
-
1. Korea Central Cancer Registry. 2008 Cancer Statistics in Korea. 2010. Ministry for Health, Welfare, and Family Affairs.2. Poon RT, Fan ST, Wong J. Selection criteria for hepatic resection in patients with large hepatocellular carcinoma larger than 10 cm in diameter. J Am Coll Surg. 2002; 194:592–602. PMID: 12022599.3. Hanazaki K, Kajikawa S, Shimozawa N, et al. Hepatic resection for hepatocellular carcinoma in diameter of >or=10 cm. Hepatogastroenterology. 2002; 49:518–523. PMID: 11995486.4. Zhou XD, Tang ZY, Ma ZC, et al. Surgery for large primary liver cancer more than 10 cm in diameter. J Cancer Res Clin Oncol. 2003; 129:543–548. PMID: 12898232.5. Nagano Y, Tanaka K, Togo S, et al. Efficacy of hepatic resection for hepatocellular carcinomas larger than 10 cm. World J Surg. 2005; 29:66–71. PMID: 15599739.
Article6. Liau KH, Ruo L, Shia J, et al. Outcome of partial hepatectomy for large (>10 cm) hepatocellular carcinoma. Cancer. 2005; 104:1948–1955. PMID: 16196045.7. Shah SA, Wei AC, Cleary SP, et al. Prognosis and results after resection of very large (>or=10 cm) hepatocellular carcinoma. J Gastrointest Surg. 2007; 11:589–595. PMID: 17393258.8. Baer HU, Gertsch P, Matthews JB, et al. Resectability of large focal liver lesions. Br J Surg. 1989; 76:1042–1044. PMID: 2597946.
Article9. Ueno S, Tanabe G, Nuruki K, et al. Prognostic performance of the new classification of primary liver cancer of Japan (4th edition) for patients with hepatocellular carcinoma: a validation analysis. Hepatol Res. 2002; 24:395–403. PMID: 12479938.
Article10. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.11. Pawlik TM, Delman KA, Vauthey JN, et al. Tumor size predicts vascular invasion and histologic grade: Implications for selection of surgical treatment for hepatocellular carcinoma. Liver Transpl. 2005; 11:1086–1092. PMID: 16123959.
Article12. Yang LY, Fang F, Ou DP, Wu W, Zeng ZJ, Wu F. Solitary large hepatocellular carcinoma: a specific subtype of hepatocellular carcinoma with good outcome after hepatic resection. Ann Surg. 2009; 249:118–123. PMID: 19106686.13. Mok KT, Wang BW, Lo GH, et al. Multimodality management of hepatocellular carcinoma larger than 10 cm. J Am Coll Surg. 2003; 197:730–738. PMID: 14585406.
Article14. Yeh CN, Lee WC, Chen MF. Hepatic resection and prognosis for patients with hepatocellular carcinoma larger than 10 cm: two decades of experience at Chang Gung memorial hospital. Ann Surg Oncol. 2003; 10:1070–1076. PMID: 14597446.
Article15. Chen XP, Qiu FZ, Wu ZD, Zhang BX. Chinese experience with hepatectomy for huge hepatocellular carcinoma. Br J Surg. 2004; 91:322–326. PMID: 14991633.
Article16. Pandey D, Lee KH, Wai CT, Wagholikar G, Tan KC. Long term outcome and prognostic factors for large hepatocellular carcinoma (10 cm or more) after surgical resection. Ann Surg Oncol. 2007; 14:2817–2823. PMID: 17690940.
Article17. Taniai N, Yoshida H, Tajiri T. Adaptation of hepatectomy for huge hepatocellular carcinoma. J Hepatobiliary Pancreat Surg. 2008; 15:410–416. PMID: 18670843.
Article18. Choi GH, Han DH, Kim DH, et al. Outcome after curative resection for a huge (>or=10 cm) hepatocellular carcinoma and prognostic significance of gross tumor classification. Am J Surg. 2009; 198:693–701. PMID: 19268907.19. Chen XP, Qiu FZ, Wu ZD, Zhang BX. Hepatectomy for huge hepatocellular carcinoma in 634 cases. World J Gastroenterol. 2006; 12:4652–4655. PMID: 16937434.
Article20. Lee SG, Hwang S, Jung JP, Lee YJ, Kim KH, Ahn CS. Outcome of patients with huge hepatocellular carcinoma after primary resection and treatment of recurrent lesions. Br J Surg. 2007; 94:320–326. PMID: 17205495.
Article21. Shimada K, Sakamoto Y, Esaki M, Kosuge T. Role of a hepatectomy for the treatment of large hepatocellular carcinomas measuring 10 cm or larger in diameter. Langenbecks Arch Surg. 2008; 393:521–526. PMID: 18188585.
Article22. Liu CL, Fan ST, Cheung ST, Lo CM, Ng IO, Wong J. Anterior approach versus conventional approach right hepatic resection for large hepatocellular carcinoma: a prospective randomized controlled study. Ann Surg. 2006; 244:194–203. PMID: 16858181.23. Ishizawa T, Kokudo N, Makuuchi M. Right hepatectomy for hepatocellular carcinoma: is the anterior approach superior to the conventional approach? Ann Surg. 2008; 247:390–391. PMID: 18216549.24. Belghiti J. Editorial perspective: resection of large hepatocellular carcinoma using combination of liver hanging maneuver and anterior approach. World J Surg. 2010; 34:1879–1880. PMID: 20414776.
Article25. Wang CC, Jawade K, Yap AQ, Concejero AM, Lin CY, Chen CL. Resection of large hepatocellular carcinoma using the combination of liver hanging maneuver and anterior approach. World J Surg. 2010; 34:1874–1878. PMID: 20414779.
Article26. Liu CL, Fan ST, Lo CM, Tung-Ping Poon R, Wong J. Anterior approach for major right hepatic resection for large hepatocellular carcinoma. Ann Surg. 2000; 232:25–31. PMID: 10862191.
Article27. Kim TH, Lee SG, Song GW, et al. Right hemihepatectomy using an anterior approach technique for a hepatocellular carcinoma >10 cm in size. Korean J Hepatobiliary Pancreat Surg. 2008; 12:232–237.28. Eggel H. Uber des primare Carcinom des Leber. Beitrage zur Pathologischen Anatomie und zur Allgemeinen Pathologie. 1901; 30:506–604.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Associating microwave ablation and portal vein ligation for staged hepatectomy for the treatment of huge hepatocellular carcinoma with cirrhosis
- Two-Stage Hepatectomy for Bilateral Hepatocellular Carcinoma with Bile Duct Tumor Thrombi
- Impact of tumor size on hepatectomy outcomes in hepatocellular carcinoma: a nationwide propensity score matching analysis
- Prognostic Factors and Clinicopathologic Features after Resection of Small Hepatocellular Carcinoma (< or =2 cm)
- The risk factors of early recurrence after hepatectomy in hepatocellular carcinoma