J Korean Neurosurg Soc.
2014 Aug;56(2):108-113. 10.3340/jkns.2014.56.2.108.
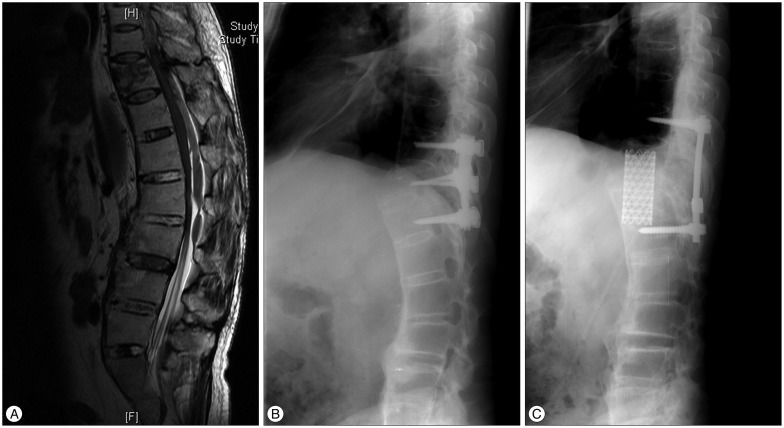
Surgical Outcomes after Traumatic Vertebral Fractures in Patients with Ankylosing Spondylitis
- Affiliations
-
- 1Department of Neurosurgery, The Spine and Spinal Cord Institute, Yonsei University College of Medicine, Gangnam Severance Hospital, Seoul, Korea. kuhsu@yuhs.ac
- 2Department of Neurosurgery, The Spine and Spinal Cord Institute, Yonsei University College of Medicine, Severance Hospital, Seoul, Korea.
- KMID: 1956512
- DOI: http://doi.org/10.3340/jkns.2014.56.2.108
Abstract
OBJECTIVE
Ankylosing spondylitis is an inflammatory rheumatic disease mainly affecting the axial skeleton. The rigid spine may secondarily develop osteoporosis, further increasing the risk of spinal fracture. In this study, we reviewed fractures in patients with ankylosing spondylitis that had been clinically diagnosed to better define the mechanism of injury, associated neurological deficit, predisposing factors, and management strategies.
METHODS
Between January 2003 and December 2013, 12 patients with 13 fractures with neurological complications were treated. Neuroimaging evaluation was obtained in all patients by using plain radiography, CT scan, and MR imaging. The ASIA Impairment Scale was used in order to evaluate the neurologic status of the patients. Management was based on the presence or absence of spinal instability.
RESULTS
A total of 9 cervical and 4 thoracolumbar fractures were identified in a review of patients in whom ankylosing spondylitis had been diagnosed. Of these, 7 fractures were associated with a hyperextension mechanism. 10 cases resulted in a fracture by minor trauma. Posttraumatic neurological deficits were demonstrated in 11 cases and neurological improvement after surgery was observed in 5 of these cases.
CONCLUSIONS
Patients with ankylosing spondylitis are highly susceptible to spinal fracture and spinal cord injury even after only mild trauma. Initial CT or MR imaging of the whole spine is recommended even if the patient's symptoms are mild. The patient should also have early surgical stabilization to correct spinal deformity and avoid worsening of the patient's neurological status.
MeSH Terms
Figure
Reference
-
1. Alaranta H, Luoto S, Konttinen YT. Traumatic spinal cord injury as a complication to ankylosing spondylitis. An extended report. Clin Exp Rheumatol. 2002; 20:66–68. PMID: 11892713.2. Anwar F, Al-Khayer A, Joseph G, Fraser MH, Jigajinni MV, Allan DB. Delayed presentation and diagnosis of cervical spine injuries in long-standing ankylosing spondylitis. Eur Spine J. 2011; 20:403–407. PMID: 21127920.
Article4. Caron T, Bransford R, Nguyen Q, Agel J, Chapman J, Bellabarba C. Spine fractures in patients with ankylosing spinal disorders. Spine (Phila Pa 1976). 2010; 35:E458–E464. PMID: 20421858.
Article5. Cornefjord M, Alemany M, Olerud C. Posterior fixation of subaxial cervical spine fractures in patients with ankylosing spondylitis. Eur Spine J. 2005; 14:401–408. PMID: 15148595.
Article6. Dean LE, Jones GT, MacDonald AG, Downham C, Sturrock RD, Macfarlane GJ. Global prevalence of ankylosing spondylitis. Rheumatology (Oxford). 2014; 53:650–657. PMID: 24324212.
Article7. Einsiedel T, Schmelz A, Arand M, Wilke HJ, Gebhard F, Hartwig E, et al. Injuries of the cervical spine in patients with ankylosing spondylitis : experience at two trauma centers. J Neurosurg Spine. 2006; 5:33–45. PMID: 16850954.
Article8. Feldtkeller E, Vosse D, Geusens P, van der Linden S. Prevalence and annual incidence of vertebral fractures in patients with ankylosing spondylitis. Rheumatol Int. 2006; 26:234–239. PMID: 15761730.
Article9. Foo D, Sarkarati M, Marcelino V. Cervical spinal cord injury complicating ankylosing spondylitis. Paraplegia. 1985; 23:358–363. PMID: 4080412.
Article10. Fox MW, Onofrio BM, Kilgore JE. Neurological complications of ankylosing spondylitis. J Neurosurg. 1993; 78:871–878. PMID: 8487068.
Article11. Garza-Mercado R. Traumatic extradural hematoma of the cervical spine. Neurosurgery. 1989; 24:410–414. PMID: 2927616.
Article12. Ghozlani I, Ghazi M, Nouijai A, Mounach A, Rezqi A, Achemlal L, et al. Prevalence and risk factors of osteoporosis and vertebral fractures in patients with ankylosing spondylitis. Bone. 2009; 44:772–776. PMID: 19442629.
Article13. Goldberg AL, Keaton NL, Rothfus WE, Daffner RH. Ankylosing spondylitis complicated by trauma : MR findings correlated with plain radiographs and CT. Skeletal Radiol. 1993; 22:333–336. PMID: 8372362.14. Graham B, Van Peteghem PK. Fractures of the spine in ankylosing spondylitis. Diagnosis, treatment, and complications. Spine (Phila Pa 1976). 1989; 14:803–807. PMID: 2781394.15. Harding JR, McCall IW, Park WM, Jones BF. Fracture of the cervical spine in ankylosing spondylitis. Br J Radiol. 1985; 58:3–7. PMID: 4063639.
Article16. Hitchon PW, From AM, Brenton MD, Glaser JA, Torner JC. Fractures of the thoracolumbar spine complicating ankylosing spondylitis. J Neurosurg. 2002; 97(2 Suppl):218–222. PMID: 12296682.
Article17. Jacobs WB, Fehlings MG. Ankylosing spondylitis and spinal cord injury : origin, incidence, management, and avoidance. Neurosurg Focus. 2008; 24:E12. PMID: 18290738.18. Karasick D, Schweitzer ME, Abidi NA, Cotler JM. Fractures of the vertebrae with spinal cord injuries in patients with ankylosing spondylitis : imaging findings. AJR Am J Roentgenol. 1995; 165:1205–1208. PMID: 7572504.
Article19. Lazaro BC, Deniz FE, Brasiliense LB, Reyes PM, Sawa AG, Theodore N, et al. Biomechanics of thoracic short versus long fixation after 3-column injury. J Neurosurg Spine. 2011; 14:226–234. PMID: 21184641.
Article20. Olerud C, Frost A, Bring J. Spinal fractures in patients with ankylosing spondylitis. Eur Spine J. 1996; 5:51–55. PMID: 8689417.
Article21. Serin E, Karakurt L, Yilmaz E, Belhan O, Varol T. Effects of two-levels, four-levels plus offset-hook posterior fixation techniques on protecting the surgical correction of unstable thoracolumbar vertebral fractures : a clinical study. Eur J Orthop Surg Traumatol. 2004; 14:1–6.
Article22. Sieper J, Braun J, Rudwaleit M, Boonen A, Zink A. Ankylosing spondylitis : an overview. Ann Rheum Dis. 2002; 61(Suppl 3):iii8–iii18. PMID: 12381506.23. Tezeren G, Kuru I. Posterior fixation of thoracolumbar burst fracture : short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech. 2005; 18:485–488. PMID: 16306834.24. Thumbikat P, Hariharan RP, Ravichandran G, McClelland MR, Mathew KM. Spinal cord injury in patients with ankylosing spondylitis : a 10-year review. Spine (Phila Pa 1976). 2007; 32:2989–2995. PMID: 18091492.25. Ticó N, Ramon S, Garcia-Ortun F, Ramirez L, Castelló T, Garcia-Fernández L, et al. Traumatic spinal cord injury complicating ankylosing spondylitis. Spinal Cord. 1998; 36:349–352. PMID: 9601116.
Article26. Weinstein PR, Karpman RR, Gall EP, Pitt M. Spinal cord injury, spinal fracture, and spinal stenosis in ankylosing spondylitis. J Neurosurg. 1982; 57:609–616. PMID: 7131059.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ankylosing Spondylitis: Prevention And Surgical Correction Of Deformity
- Spine Fracture in Tuberculous Kyphosis : A Case Report
- Delayed Traumatic Diaphragm Hernia after Thoracolumbar Fracture in a Patient with Ankylosing Spondylitis
- Spine Fractures in Patients with Ankylosing Spondylitis : Three Cases Report
- Complete Fusion of Three Lumbar Vertebral Bodies in Ankylosing Spondylitis