Anat Cell Biol.
2014 Sep;47(3):210-213. 10.5115/acb.2014.47.3.210.
Absent portal vein bifurcation: a rare variant and its clinical significance
- Affiliations
-
- 1Deaprtment of Radiodiagnosis, IMS and SUM Hospital, Bhubaneswar, Odisha, India. darierdarier2000@gmail.com
- 2Deaprtment of Anatomy, IMS and SUM Hospital, Bhubaneswar, Odisha, India.
- KMID: 1882598
- DOI: http://doi.org/10.5115/acb.2014.47.3.210
Abstract
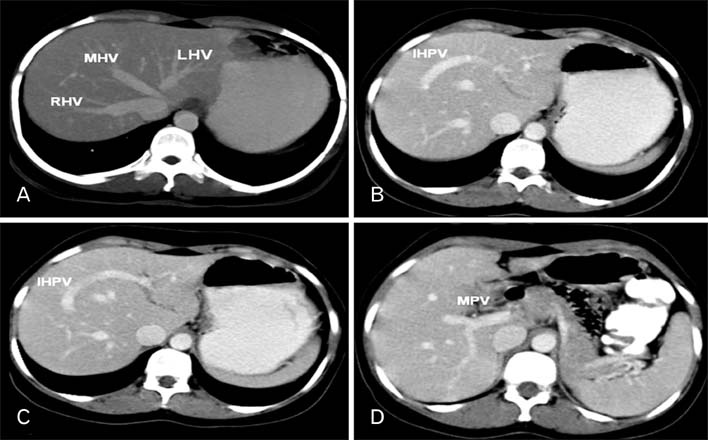
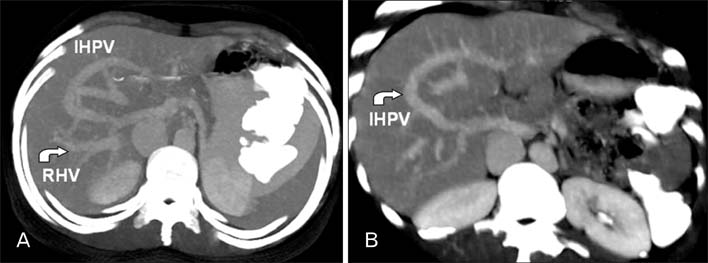
- Portal vein branching anomaly occurs due to aberration of normal anastomotic patterns and involution of vitelline veins during development of portal vein. Anatomical knowledge of portal vein and its branching pattern is important for hepatobiliary surgeon and gastrointestinal intervention radiologist. We are reporting a case of absence of portal vein bifurcation showing single main intrahepatic portal vein with gradual decreasing caliber distally, in a young female patient on contrast-enhanced computed tomography study of abdomen. Few cases of absence of portal bifurcation have been reported in literature so far.
Keyword
Figure
Cited by 1 articles
-
Study of surgical anatomy of portal vein of liver segments by cast method and its clinical implications
Vidya C. Shrikantaiah, Manjaunatha Basappa, Sangita Hazrika, Roopa Ravindranath
Anat Cell Biol. 2018;51(4):232-235. doi: 10.5115/acb.2018.51.4.232.
Reference
-
1. Varotti G, Gondolesi GE, Goldman J, Wayne M, Florman SS, Schwartz ME, Miller CM, Sukru E. Anatomic variations in right liver living donors. J Am Coll Surg. 2004; 198:577–582.2. Kamel IR, Kruskal JB, Pomfret EA, Keogan MT, Warmbrand G, Raptopoulos V. Impact of multidetector CT on donor selection and surgical planning before living adult right lobe liver transplantation. AJR Am J Roentgenol. 2001; 176:193–200.3. Marks C. Developmental basis of the portal venous system. Am J Surg. 1969; 117:671–681.4. Chaib E. Absence of bifurcation of the portal vein. Surg Radiol Anat. 2009; 31:389–392.5. Covey AM, Brody LA, Getrajdman GI, Sofocleous CT, Brown KT. Incidence, patterns, and clinical relevance of variant portal vein anatomy. AJR Am J Roentgenol. 2004; 183:1055–1064.6. Kouadio EK, Bessayah A, Valette PJ, Glehen O, Nloga J, Diabaté AS, Garcier JM, Cotton F. Anatomic variation: absence of portal vein bifurcation. Surg Radiol Anat. 2011; 33:459–463.7. Ito K, Matsunaga N, Mitchell DG, Fujita T, Honjo K, Awaya H, Nomura S, Higuchi M, Kada T, Fujita N, Ogawa Y. Imaging of congenital abnormalities of the portal venous system. AJR Am J Roentgenol. 1997; 168:233–237.8. Couinaud C. Liver anatomy: portal (and suprahepatic) or biliary segmentation. Dig Surg. 1999; 16:459–467.9. Atri M, Bret PM, Fraser-Hill MA. Intrahepatic portal venous variations: prevalence with US. Radiology. 1992; 184:157–158.10. Koh MK, Ahmad H, Watanapa P, Jalleh RP, Habib NA. Beware the anomalous portal vein. HPB Surg. 1994; 7:237–239.11. Koç Z, Oğuzkurt L, Ulusan S. Portal vein variations: clinical implications and frequencies in routine abdominal multidetector CT. Diagn Interv Radiol. 2007; 13:75–80.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Anuerysmal Dilatation of the Intrahepatic Portal Vein
- Portal bifurcation reconstruction using own hepatic vein grafts due to portal vein anomaly of the living donor for the patient with portal vein thrombosis
- Preduodenal Portal Vein Associated with Duodenal Obstruction: A case report
- Congenital Portal Vein Aneurysm: A case report
- Blood flow volume difference (P-SS) between the portal vein and thesum of splenic vein and superior mesenteric vein in portal hypertension