Ann Hepatobiliary Pancreat Surg.
2020 Nov;24(4):533-538. 10.14701/ahbps.2020.24.4.533.
Portal bifurcation reconstruction using own hepatic vein grafts due to portal vein anomaly of the living donor for the patient with portal vein thrombosis
- Affiliations
-
- 1Department of Surgery, Iwate Medical University Hospital, Yahaba, Japan
- KMID: 2508865
- DOI: http://doi.org/10.14701/ahbps.2020.24.4.533
Abstract
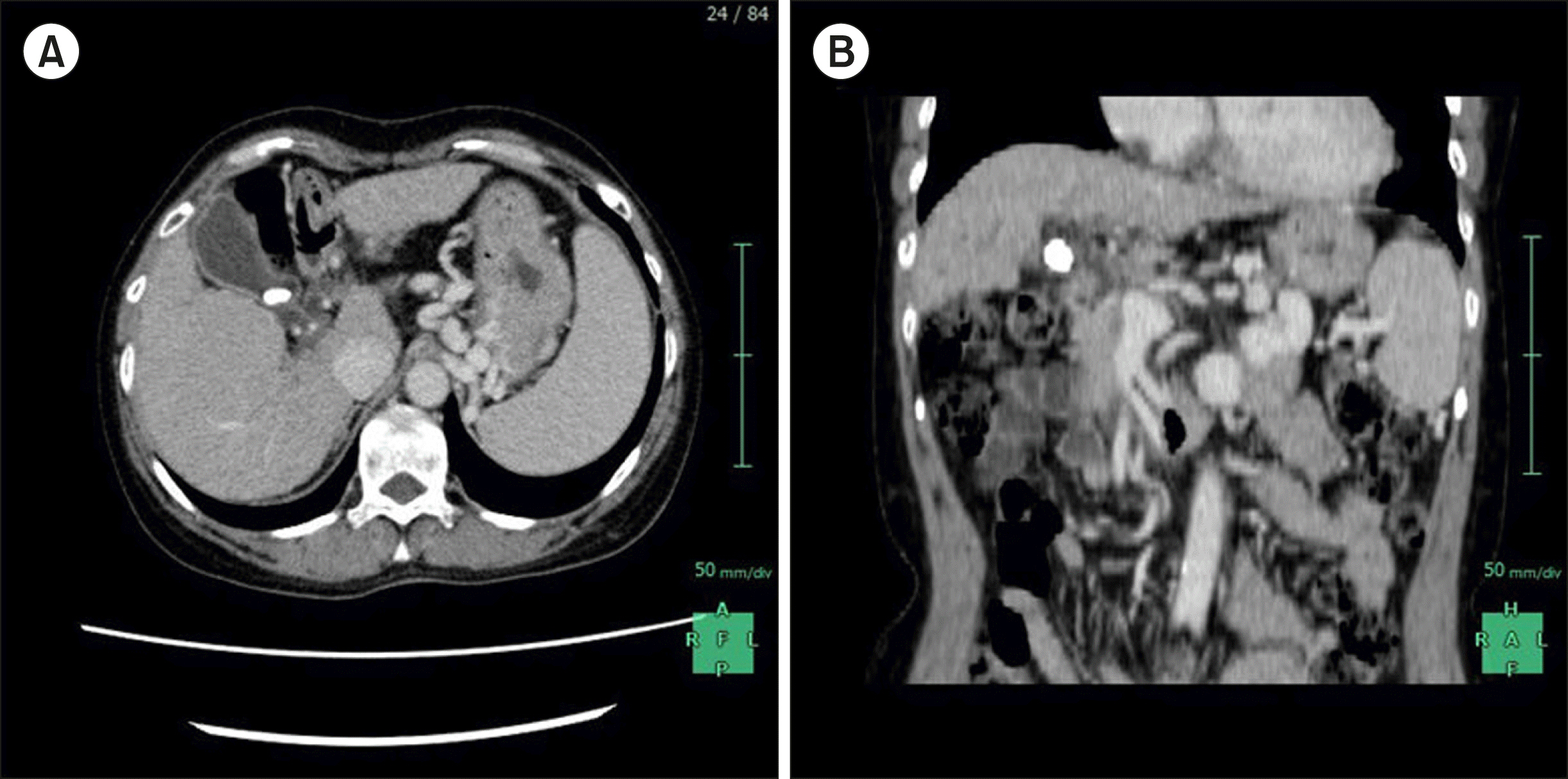
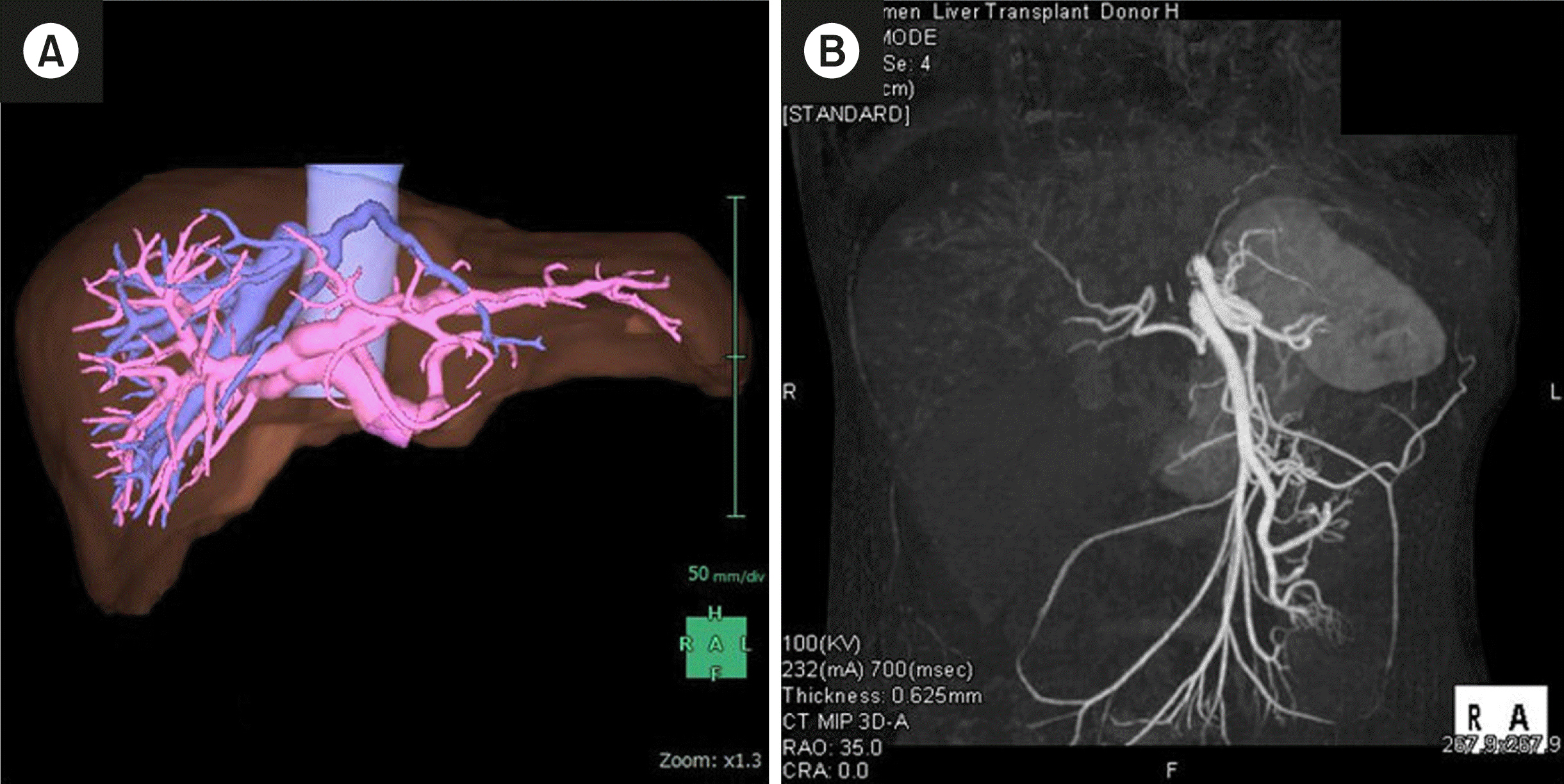
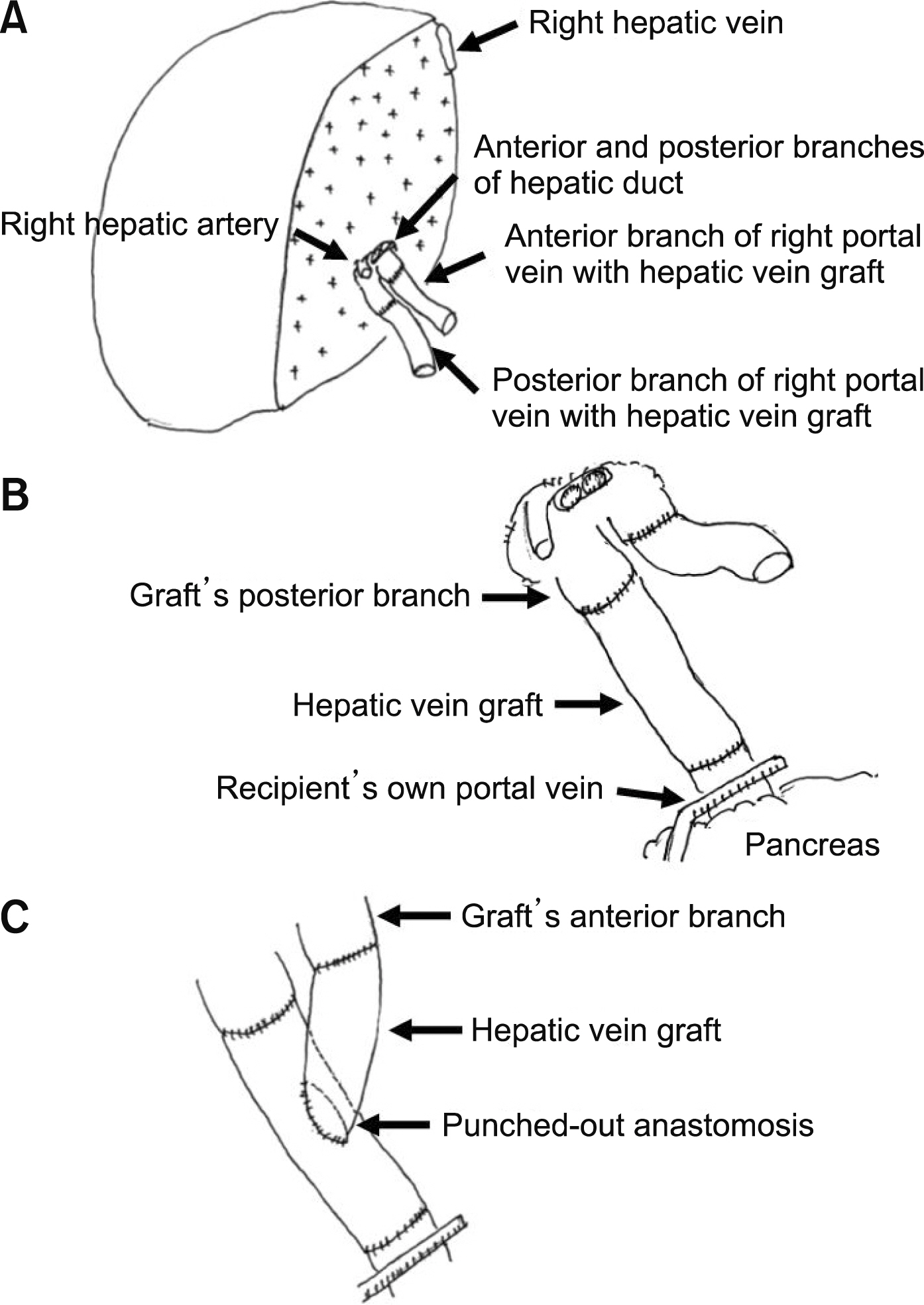
- A 57-year-old Japanese female was considered for living donor liver transplantation (LDLT) due to end-stage liver cirrhosis caused by primary biliary cholangitis with portal vein thrombosis (PVT) formation. A 26-year-old daughter of the patient was selected as a living donor; however, a computed tomography examination revealed trifurcated-type portal vein anomaly (PVA). Preoperative liver volumetry showed that the right lobe graft was necessary for the recipient; therefore, reconstruction of the portal vein bifurcation during LDLT was necessary. We planned to extract the recipient’s own hepatic vein grafts after total hepatectomy, and these would be attached with anterior and posterior portal branches as jump grafts. We performed laparoscopic donor hepatectomy as usual, and the recipient’s hepatic vein grafts were anastomosed on the bench. Then, the liver graft was inserted, and the hepatic vein reconstruction was routinely performed. We confirmed the alignment between the recipient’s portal vein and the bridged hepatic vein graft of the liver graft’s posterior branch, and anastomosed these two vessels. Moreover, we confirmed the front flow and expansion of the reconstructed posterior branch by declamping only the suprapancreatic side of the portal vein. The decision regarding the punch-out location was crucial. We confirmed the alignment between the reconstructed posterior branch and the bridged hepatic vein graft of the anterior branch, and anastomosed these two vessels employing the punched-out technique. In LDLT, liver transplant surgeons occasionally encounter living donors with PVA or recipients with PVT. Our contrivance may be useful when the liver graft needs reconstruction of portal vein bifurcation.
Keyword
Figure
Reference
-
1. Song S, Kwon CH, Kim JM, Joh JW, Lee SK. 2016; Single-center experience of living donor liver transplantation in patients with portal vein thrombosis. Clin Transplant. 30:1146–1151. DOI: 10.1111/ctr.12803. PMID: 27411211.
Article2. Lendoire J, Raffin G, Cejas N, Duek F, Barros Schelotto P, Trigo P, et al. 2007; Liver transplantation in adult patients with portal vein thrombosis: risk factors, management and outcome. HPB (Oxford). 9:352–356. DOI: 10.1080/13651820701599033. PMID: 18345318. PMCID: PMC2225512.
Article3. Iqbal S, Iqbal R, Iqbal F. 2017; Surgical implications of portal vein variations and liver segmentations: a recent update. J Clin Diagn Res. 11:AE01–AE05. DOI: 10.7860/JCDR/2017/25028.9453. PMID: 28384848. PMCID: PMC5376876.4. Hibi T, Nishida S, Levi DM, Selvaggi G, Tekin A, Fan J, et al. 2014; When and why portal vein thrombosis matters in liver transplantation: a critical audit of 174 cases. Ann Surg. 259:760–766. DOI: 10.1097/SLA.0000000000000252. PMID: 24299686.5. Cheng YF, Huang TL, Lee TY, Chen TY, Chen CL. 1996; Variation of the intrahepatic portal vein; angiographic demonstration and application in living-related hepatic transplantation. Transplant Proc. 28:1667–1668.6. Hasegawa Y, Nitta H, Takahara T, Katagiri H, Kanno S, Sasaki A. 2019; Pure laparoscopic living donor hepatectomy using the Glissonean pedicle approach (with video). Surg Endosc. 33:2704–2709. DOI: 10.1007/s00464-019-06818-7. PMID: 31087174.
Article7. Song JL, Wu H, Yang JY. 2019; Laparoscopic donor right hepatectomy in a donor with type III portal vein anomaly: a case report. Medicine (Baltimore). 98:e16736. DOI: 10.1097/MD.0000000000016736. PMID: 31393384. PMCID: PMC6708953.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Portal vein fenestration: a case report of an unusual portal vein developmental anomaly
- Absent portal vein bifurcation: a rare variant and its clinical significance
- Successful laparoscopic living donor right hepatectomy in a case with challenging portal vein variation
- The paracholedochal vein: a feasible option as portal inflow in living donor liver transplantation
- Renoportal Anastomosis in Living Donor Liver Transplantation; An Effective Technique for Patient with Diffuse Portal Vein Thrombosis and Large Splenorenal Shunts