Yonsei Med J.
2014 Sep;55(5):1310-1317. 10.3349/ymj.2014.55.5.1310.
Neck Circumference and Lowest Oxygen Saturation Are Independently Associated with High Coexistence of Hypertension in Obstructive Sleep Apnea
- Affiliations
-
- 1Department of Otorhinolaryngology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. hyungjucho@yuhs.ac
- 2Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. shpark0530@yuhs.ac
- 3The Airway Mucus Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1799496
- DOI: http://doi.org/10.3349/ymj.2014.55.5.1310
Abstract
- PURPOSE
Obstructive sleep apnea (OSA) is considered an independent risk factor for hypertension. However, it is still not clear which clinical factors are related with the presence of hypertension in OSA patients. We aimed to find different physical features and compare the sleep study results which are associated with the occurrence of hypertension in OSA patients.
MATERIALS AND METHODS
Medical records were retrospectively reviewed for patients diagnosed with OSA at Severance Cardiovascular Hospital between 2010 and 2013. Males with moderate to severe OSA patients were enrolled in this study. Clinical and polysomnographic features were evaluated to assess clinical variables that are significantly associated with hypertension by statistical analysis.
RESULTS
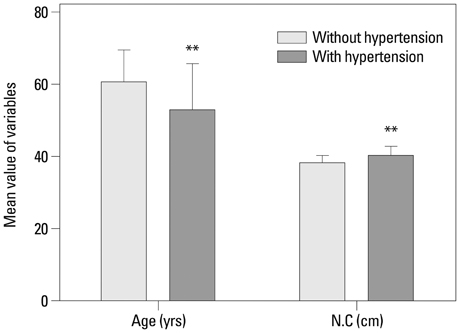
Among men with moderate to severe OSA, age was negatively correlated with hypertension (odds ratio=0.956), while neck circumference was positively correlated with the presence of hypertension (odds ratio=1.363). Among the polysomnographic results, the lowest O2 saturation during sleep was significantly associated with the presence of hypertension (odds ratio=0.900).
CONCLUSION
Age and neck circumference should be considered as clinically significant features, and the lowest blood O2 saturation during sleep should be emphasized in predicting the coexistence or development of hypertension in OSA patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Calhoun DA. Obstructive sleep apnea and hypertension. Curr Hypertens Rep. 2010; 12:189–195.
Article2. Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995; 155:701–709.
Article3. Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009; 338:b1665.
Article4. Drager LF, Genta PR, Pedrosa RP, Nerbass FB, Gonzaga CC, Krieger EM, et al. Characteristics and predictors of obstructive sleep apnea in patients with systemic hypertension. Am J Cardiol. 2010; 105:1135–1139.
Article5. Manolis AJ, Poulimenos LE, Kallistratos MS, Gavras I, Gavras H. Sympathetic overactivity in hypertension and cardiovascular disease. Curr Vasc Pharmacol. 2014; 12:4–15.6. White LH, Bradley TD. Role of nocturnal rostral fluid shift in the pathogenesis of obstructive and central sleep apnoea. J Physiol. 2013; 591(Pt 5):1179–1193.
Article7. White LH, Motwani S, Kasai T, Yumino D, Amirthalingam V, Bradley TD. Effect of rostral fluid shift on pharyngeal resistance in men with and without obstructive sleep apnea. Respir Physiol Neurobiol. 2014; 192:17–22.
Article8. Sharma SK, Agrawal S, Damodaran D, Sreenivas V, Kadhiravan T, Lakshmy R, et al. CPAP for the metabolic syndrome in patients with obstructive sleep apnea. N Engl J Med. 2011; 365:2277–2286.
Article9. Cuhadaroğlu C, Utkusavaş A, Oztürk L, Salman S, Ece T. Effects of nasal CPAP treatment on insulin resistance, lipid profile, and plasma leptin in sleep apnea. Lung. 2009; 187:75–81.
Article10. Lin QC, Zhang XB, Chen GP, Huang DY, Din HB, Tang AZ. Obstructive sleep apnea syndrome is associated with some components of metabolic syndrome in nonobese adults. Sleep Breath. 2012; 16:571–578.
Article11. Adedayo AM, Olafiranye O, Smith D, Hill A, Zizi F, Brown C, et al. Obstructive sleep apnea and dyslipidemia: evidence and underlying mechanism. Sleep Breath. 2014; 18:13–18.
Article12. Drager LF, Pereira AC, Barreto-Filho JA, Figueiredo AC, Krieger JE, Krieger EM, et al. Phenotypic characteristics associated with hypertension in patients with obstructive sleep apnea. J Hum Hypertens. 2006; 20:523–528.
Article13. Stranges S, Dorn JM, Cappuccio FP, Donahue RP, Rafalson LB, Hovey KM, et al. A population-based study of reduced sleep duration and hypertension: the strongest association may be in premenopausal women. J Hypertens. 2010; 28:896–902.
Article14. Lopez-Garcia E, Faubel R, Guallar-Castillon P, Leon-Muñoz L, Banegas JR, Rodriguez-Artalejo F. Self-reported sleep duration and hypertension in older Spanish adults. J Am Geriatr Soc. 2009; 57:663–668.
Article15. Wolk R, Shamsuzzaman AS, Somers VK. Obesity, sleep apnea, and hypertension. Hypertension. 2003; 42:1067–1074.
Article16. Chung F, Liao P, Sun Y, Amirshahi B, Fazel H, Shapiro CM, et al. Perioperative practical experiences in using a level 2 portable polysomnography. Sleep Breath. 2011; 15:367–375.
Article17. Mohsenin V. Gender differences in the expression of sleep-disordered breathing: role of upper airway dimensions. Chest. 2001; 120:1442–1447.
Article18. Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfield MJ, et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J Hypertens. 2009; 27:2121–2158.
Article19. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003; 289:2560–2572.
Article20. Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000; 342:1378–1384.
Article21. Gjevre JA, Taylor-Gjevre RM, Skomro R, Reid J, Fenton M, Cotton D. Comparison of polysomnographic and portable home monitoring assessments of obstructive sleep apnea in Saskatchewan women. Can Respir J. 2011; 18:271–274.
Article22. Fusetti M, Fioretti AB, Valenti M, Masedu F, Lauriello M, Pagliarella M. Cardiovascular and metabolic comorbidities in patients with obstructive sleep apnoea syndrome. Acta Otorhinolaryngol Ital. 2012; 32:320–325.23. Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Leiby BE, Vela-Bueno A, et al. Association of hypertension and sleep-disordered breathing. Arch Intern Med. 2000; 160:2289–2295.
Article24. Morrell MJ, Finn L, McMillan A, Peppard PE. The impact of ageing and sex on the association between sleepiness and sleep disordered breathing. Eur Respir J. 2012; 40:386–393.
Article25. Yu JC, Berger P 3rd. Sleep apnea and obesity. S D Med. 2011; Spec No:28-34.26. Slater G, Pengo MF, Kosky C, Steier J. Obesity as an independent predictor of subjective excessive daytime sleepiness. Respir Med. 2013; 107:305–309.
Article27. Narang I, Mathew JL. Childhood obesity and obstructive sleep apnea. J Nutr Metab. 2012; 2012:134202.
Article28. Broström A, Sunnergren O, Nilsen P, Fridlund B, Ulander M, Svanborg E. Gender differences in respiratory disturbance, sleep and daytime sleepiness in hypertensive patients with different degrees of obesity. Eur J Cardiovasc Nurs. 2013; 12:140–149.
Article29. Zen V, Fuchs FD, Wainstein MV, Gonçalves SC, Biavatti K, Riedner CE, et al. Neck circumference and central obesity are independent predictors of coronary artery disease in patients undergoing coronary angiography. Am J Cardiovasc Dis. 2012; 2:323–330.30. Medeiros CA, Bruin VM, Castro-Silva Cd, Araújo SM, Chaves Junior CM, Bruin PF. Neck circumference, a bedside clinical feature related to mortality of acute ischemic stroke. Rev Assoc Med Bras. 2011; 57:559–564.
Article31. Friedman O, Bradley TD, Chan CT, Parkes R, Logan AG. Relationship between overnight rostral fluid shift and obstructive sleep apnea in drug-resistant hypertension. Hypertension. 2010; 56:1077–1082.
Article32. Friedman O, Bradley TD, Logan AG. Influence of lower body positive pressure on upper airway cross-sectional area in drug-resistant hypertension. Hypertension. 2013; 61:240–245.
Article33. Ursavas A, Karadag M, Nalci N, Ercan I, Gozu RO. Self-reported snoring, maternal obesity and neck circumference as risk factors for pregnancy-induced hypertension and preeclampsia. Respiration. 2008; 76:33–39.
Article34. Fink B, Manning JT, Neave N. The 2nd-4th digit ratio (2D:4D) and neck circumference: implications for risk factors in coronary heart disease. Int J Obes (Lond). 2006; 30:711–714.
Article35. Mungan U, Ozeke O, Mavioglu L, Ertan C, Karaca IO, Keskin G, et al. The role of the preoperative screening of sleep apnoea by Berlin Questionnaire and Epworth Sleepiness Scale for postoperative atrial fibrillation. Heart Lung Circ. 2013; 22:38–42.
Article36. Sjöström C, Lindberg E, Elmasry A, Hägg A, Svärdsudd K, Janson C. Prevalence of sleep apnoea and snoring in hypertensive men: a population based study. Thorax. 2002; 57:602–607.
Article37. Dumitrascu R, Heitmann J, Seeger W, Weissmann N, Schulz R. Obstructive sleep apnea, oxidative stress and cardiovascular disease: lessons from animal studies. Oxid Med Cell Longev. 2013; 2013:234631.
Article38. Franco CM, Lima AM, Ataíde L Jr, Lins OG, Castro CM, Bezerra AA, et al. Obstructive sleep apnea severity correlates with cellular and plasma oxidative stress parameters and affective symptoms. J Mol Neurosci. 2012; 47:300–310.
Article39. Yamauchi M, Nakano H, Maekawa J, Okamoto Y, Ohnishi Y, Suzuki T, et al. Oxidative stress in obstructive sleep apnea. Chest. 2005; 127:1674–1679.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The relationship between the predictors of obstructive sleep apnea and difficult intubation
- Predictors for Presence and Severity of Obstructive Sleep Apnea in Snoring Patients: Significance of Neck Circumference
- Therapeutic Change of Sleep Structure and Function by Continuous Positive Airway Pressure Application in Obstructive Sleep Apnea Syndrome
- Validation of Embletta for Diagnosis of Obstructive Sleep Apnea
- Neurocognitive Function in Obstructive Sleep Apnea Patients