Yonsei Med J.
2013 Nov;54(6):1491-1497. 10.3349/ymj.2013.54.6.1491.
Comparative Study for Preventive Effects of Intra-Abdominal Adhesion Using Cyclo-Oxygenase-2 Enzyme (COX-2) Inhibitor, Low Molecular Weight Heparin (LMWH), and Synthetic Barrier
- Affiliations
-
- 1Department of Surgery, Ewha Womans University College of Medicine, Seoul, Korea. kimyi@ewha.ac.kr
- KMID: 1798148
- DOI: http://doi.org/10.3349/ymj.2013.54.6.1491
Abstract
- PURPOSE
Postoperative adhesion is the most frequent complication of abdominal surgery. Therefore, we investigated the individual effects of synthetic barrier [hyaluronic acid/carboxymethylcellulose (HA/CMC)] and pharmacologic agents [low molecular weight heparin (LMWH) cyclo-oxygenase-2 inhibitor (COX-2 inhibitor)] using animal model of intra-abdominal adhesion.
MATERIALS AND METHODS
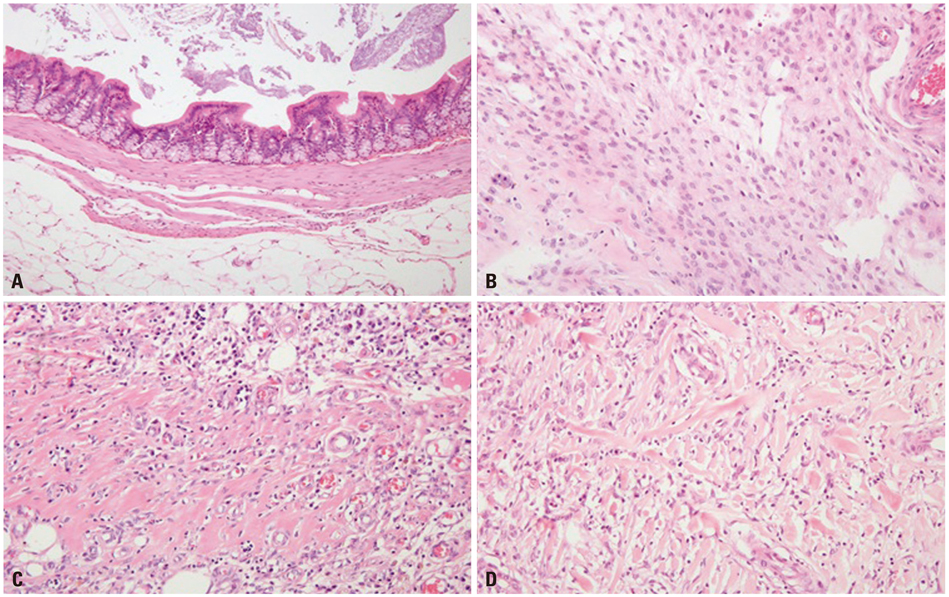
The cecum was rubbed with sterile alcohol wet gauze until subserosal haemorrhage and punctate bleeding developed under the general anesthesia. Five animal groups were prepared using the film HA/CMC, gel HA/CMC, LMWH and COX-2 inhibitor.
RESULTS
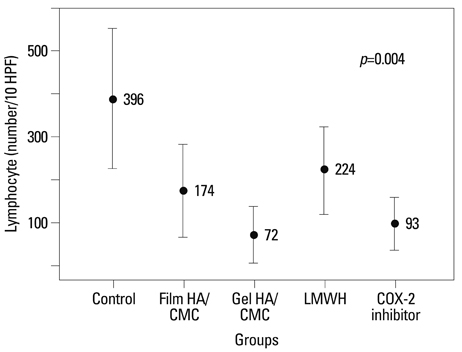
The grade of adhesion by modified Leach method for group I (control), II (film type HA/CMC), III (gel type HA/CMC), IV (LMWH) and V (COX-2 inhibitor) were 5.35+/-1.8, 6.15+/-1.3, 4.23+/-2.6, 5.05+/-0.7 and 5.50+/-0.9, respectively. Group III showed the least grade of adhesion and it is statistically significant in adhesion formation (p=0.028). The numbers of lymphocytes were significantly low in group III and group V compared to the control group (lymphocyte: p=0.004). The mast cell counts were generally low except for the control group (I: 1.05, II: 0.35, III: 0.38, IV: 0.20, V: 0.37), however, it was not statistically significant (p=0.066).
CONCLUSION
The gel barriers were shown to be partly efficient in inhibiting the formation of postoperative adhesions and might provide an option for abdominal surgery to reduce postoperative adhesions. The LMWH and COX-2 inhibitor had been known for their inhibitor effect of fibrin formation and anti-angiogenic/anti-fibroblastic activity, respectively. However, their preventive effects of adhesion and fibrosis were found to be obscure.
Keyword
MeSH Terms
Figure
Reference
-
1. Menzies D, Ellis H. Intestinal obstruction from adhesions--how big is the problem? Ann R Coll Surg Engl. 1990; 72:60–63.2. Menzies D. Peritoneal adhesions. Incidence, cause, and prevention. Surg Annu. 1992; 24(Pt 1):27–45.3. Vrijland WW, Jeekel J, van Geldorp HJ, Swank DJ, Bonjer HJ. Abdominal adhesions: intestinal obstruction, pain, and infertility. Surg Endosc. 2003; 17:1017–1022.
Article4. Liakakos T, Thomakos N, Fine PM, Dervenis C, Young RL. Peritoneal adhesions: etiology, pathophysiology, and clinical significance. Recent advances in prevention and management. Dig Surg. 2001; 18:260–273.
Article5. Diamond MP, Wexner SD, diZereg GS, Korell M, Zmora O, Van Goor H, et al. Adhesion prevention and reduction: current status and future recommendations of a multinational interdisciplinary consensus conference. Surg Innov. 2010; 17:183–188.
Article6. Saed GM, Zhang W, Chegini N, Holmdahl L, Diamond MP. Transforming growth factor beta isoforms production by human peritoneal mesothelial cells after exposure to hypoxia. Am J Reprod Immunol. 2000; 43:285–291.
Article7. Ellis H, Moran BJ, Thompson JN, Parker MC, Wilson MS, Menzies D, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1999; 353:1476–1480.
Article8. Avsar FM, Sahin M, Aksoy F, Avsar AF, Aköz M, Hengirmen S, et al. Effects of diphenhydramine HCl and methylprednisolone in the prevention of abdominal adhesions. Am J Surg. 2001; 181:512–515.
Article9. Karaca T, Gözalan AU, Yoldaş Ö, Bilgin BÇ, Tezer A. Effects of tamoxifen citrate on postoperative intra-abdominal adhesion in a rat model. Int J Surg. 2013; 11:68–72.
Article10. Kement M, Censur Z, Oncel M, Buyukokuroglu ME, Gezen FC. Heparin for adhesion prevention: comparison of three different dosages with Seprafilm in a murine model. Int J Surg. 2011; 9:225–228.
Article11. Schreinemacher MH, Emans PJ, Gijbels MJ, Greve JW, Beets GL, Bouvy ND. Degradation of mesh coatings and intraperitoneal adhesion formation in an experimental model. Br J Surg. 2009; 96:305–313.
Article12. Beck DE, Cohen Z, Fleshman JW, Kaufman HS, van Goor H, Wolff BG, et al. A prospective, randomized, multicenter, controlled study of the safety of Seprafilm adhesion barrier in abdominopelvic surgery of the intestine. Dis Colon Rectum. 2003; 46:1310–1319.
Article13. Lalountas MA, Ballas KD, Skouras C, Asteriou C, Kontoulis T, Pissas D, et al. Preventing intraperitoneal adhesions with atorvastatin and sodium hyaluronate/carboxymethylcellulose: a comparative study in rats. Am J Surg. 2010; 200:118–123.
Article14. Diamond MP, Burns EL, Accomando B, Mian S, Holmdahl L. Seprafilm® adhesion barrier: (1) a review of preclinical, animal, and human investigational studies. Gynecol Surg. 2012; 9:237–245.
Article15. Dietrich A, Bouzidi M, Hartwig T, Schütz A, Jonas S. Rapamycin and a hyaluronic acid-carboxymethylcellulose membrane did not lead to reduced adhesion formations in a rat abdominal adhesion model. Arch Gynecol Obstet. 2012; 285:1603–1609.
Article16. Hashimoto D, Hirota M, Yagi Y, Baba H. Hyaluronate carboxymethylcellulose-based bioresorbable membrane (Seprafilm) reduces adhesion under the incision to make unplanned re-laparotomy safer. Surg Today. 2012; 42:863–867.
Article17. Yang EJ, Kang E, Jang JY, Kim D, Yom CK, Lim JY, et al. Effect of a mixed solution of sodium hyaluronate and carboxymethyl cellulose on upper limb dysfunction after total mastectomy: a double-blind, randomized clinical trial. Breast Cancer Res Treat. 2012; 136:187–194.
Article18. Imai A, Takagi H, Matsunami K, Suzuki N. Non-barrier agents for postoperative adhesion prevention: clinical and preclinical aspects. Arch Gynecol Obstet. 2010; 282:269–275.
Article19. Aksakal O, Yilmaz B, Gungor T, Sirvan L, Sut N, Inan I, et al. A randomised controlled trial on melatonin and rosiglitazone for prevention of adhesion formation in a rat uterine horn model. Arch Gynecol Obstet. 2010; 282:55–61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparative Study on the side Effects of Low Molecular Weight Heparin and Unfractionated Heparin Therapy in non-insulin-Dependent Diabetes Mellitus Patients
- Effect of Low Molecular Weight Heparin on Plasma Thrombin-Antithrombin Complex and Tissue Factor Pathway Inhibitor in Patients with Coronary Artery Disease
- Safety and Feasibility of Subcutaneous Low Molecular Weight Heparin for Cerebral Venous Sinus Thrombosis
- Effect of standard heparin and low molecular weight heparin on fibrinolytic activity
- Spontaneous Intramuscular Hematoma associated with Acute Compartment Syndrome after Treatment of Low Molecular Weight Heparin: A Report of Two Cases