Korean J Ophthalmol.
2013 Jun;27(3):204-207. 10.3341/kjo.2013.27.3.204.
A Case of Muir-Torre Syndrome with Multiple Cancers of Bilateral Eyelids and Breast
- Affiliations
-
- 1Department of Ophthalmology Faculty of Medicine, Kagoshima University Graduate School of Medicine and Dental Sciences, Kagoshima, Japan. tsakamot@m3.kufm.kagoshima-u.ac.jp
- 2Department of Ophthalmology, Kyushu University School of Medicine, Fukuoka, Japan.
- KMID: 1798059
- DOI: http://doi.org/10.3341/kjo.2013.27.3.204
Abstract
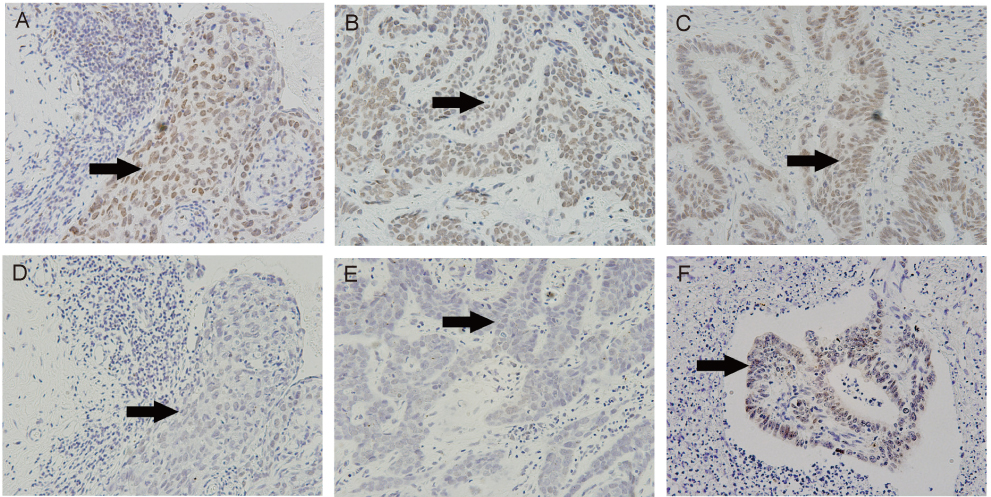
- We report a case of Muir-Torre syndrome (MTS) with a very rare combination of cancers, involving bilateral eyelid cancers and breast cancer. A 71-year-old female with a history of breast cancer from 18 years prior presented with bilateral eyelid tumors. One of her siblings had lung cancer, and another had pancreatic cancer. She underwent excisional biopsy of the eyelid tumors and histopathology revealed sebaceous carcinoma of the right eyelid and basal cell carcinoma of the left. She was diagnosed with MTS: a skin cancer associated with visceral malignancy. Immunohistochemical tests for mutS homolog 2 showed a lack of expression in both eyelid carcinomas.
MeSH Terms
Figure
Reference
-
1. Shalin SC, Lyle S, Calonje E, Lazar AJ. Sebaceous neoplasia and the Muir-Torre syndrome: important connections with clinical implications. Histopathology. 2010. 56:133–147.2. South CD, Hampel H, Comeras I, et al. The frequency of Muir-Torre syndrome among Lynch syndrome families. J Natl Cancer Inst. 2008. 100:277–281.3. Muir EG, Bell AJ, Barlow KA. Multiple primary carcinomata of the colon, duodenum, and larynx associated with kerato-acanthomata of the face. Br J Surg. 1967. 54:191–195.4. Torre D. Multiple sebaceous tumors. Arch Dermatol. 1968. 98:549–551.5. Ponti G, Ponz de Leon M. Muir-Torre syndrome. Lancet Oncol. 2005. 6:980–987.6. Kwak EL, Chung DC. Chung DC, Harbor DA, editors. Hereditary colon cancer: Lynch syndrome. Principles of clinical cancer genetics: a handbook from the Massachusetts General Hospital. 2010. New York: Springer;77–88.7. Akhtar S, Oza KK, Khan SA, Wright J. Muir-Torre syndrome: case report of a patient with concurrent jejunal and ureteral cancer and a review of the literature. J Am Acad Dermatol. 1999. 41(5 Pt 1):681–686.8. Marazza G, Masouye I, Taylor S, et al. An illustrative case of Muir-Torre syndrome: contribution of immunohistochemical analysis in identifying indicator sebaceous lesions. Arch Dermatol. 2006. 142:1039–1042.9. Abbas O, Mahalingam M. Cutaneous sebaceous neoplasms as markers of Muir-Torre syndrome: a diagnostic algorithm. J Cutan Pathol. 2009. 36:613–619.10. Ko CJ. Muir-Torre syndrome: facts and controversies. Clin Dermatol. 2010. 28:324–329.11. Takamura H, Yamashita H. Clinicopathological analysis of malignant eyelid tumor cases at Yamagata university hospital: statistical comparison of tumor incidence in Japan and in other countries. Jpn J Ophthalmol. 2005. 49:349–354.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Muir-Torre Syndrome Confirmed by Genetic Mutation Analysis
- A Case of Muir-Torre Syndrome: Extra-ocular Sebaceous Carcinoma in a Patient with Breast Cancer
- Sebaceous Carcinoma Associated with Breast Cancer, Stomach Cancer, and Colon Cancer: Muir-Torre Syndrome
- A Case of Muir-Torre Syndrome
- A Case of Sebaceous Carcinoma on the Extraocular Area Associated withB-cell Lymphoma, Esophageal Cancer and Gastric Cancer -A Case of Muir-Torre Syndrome-