J Korean Med Sci.
2009 Oct;24(5):818-823. 10.3346/jkms.2009.24.5.818.
Short- and Long-Term Results of Triple Valve Surgery: A Single Center Experience
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Hanyang University Guri Hospital, College of Medicine, University of Hanyang, Guri, Korea.
- 2Department of Cardiovascular Surgery, Sejong General Hospital, Bucheon, Korea. ssoh97@sejongh.co.kr
- 3Department of Thoracic and Cardiovascular Surgery, Kangwon National University Hospital, College of Medicine, Kangwon National University, Chuncheon, Korea.
- 4Department of Thoracic and Cardiovascular Surgery, Korea University Guro Hospital, College of Medicine, University of Korea, Seoul, Korea.
- 5Department of Thoracic and Cardiovascular Surgery, Sanbon Medical Center, College of Medicine, University of Wonkwang, Gunpo, Korea.
- KMID: 1782000
- DOI: http://doi.org/10.3346/jkms.2009.24.5.818
Abstract
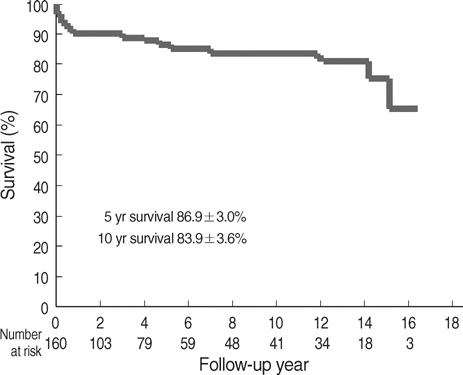
- Triple valve surgery is usually complex and carries a reported operative mortality of 13% and 10-yr survival of 61%. We examined surgical results based on our hospital's experience. A total of 160 consecutive patients underwent triple valve surgery from 1990 to 2006. The most common aortic and mitral valve disease was rheumatic disease (82%). The most common tricuspid valve disease was functional regurgitation (80%). Seventy-four percent of the patients were in New York Heart Association (NYHA) class III and IV. Univariate and multivariable analyses were performed to identify predictors of early and late survival. Operative mortality was 6.9% (n=11). Univariate factors associated with mortality included old age, preoperative renal failure, postoperative renal failure, pulmonary complications, and stroke. Of them, postoperative renal failure and stroke were associated with mortality on multivariable analysis. Otherwise, neither tricuspid valve replacement nor reoperation were statistically associated with late mortality. Survival at 5 and 10 yr was 87% and 84%, respectively. Ninety-two percent of the patients were in NYHA class I and II at their most recent follow-up. Ten-year freedom from prosthetic valve endocarditis was 97%; from anticoagulation-related hemorrhage, 82%; from thromboembolism, 89%; and from reoperation, 84%. Postoperative renal failure and stroke were significantly related with operative mortality. Triple valve surgery, regardless of reoperation and tricuspid valve replacement, results in acceptable long-term survival.
Keyword
MeSH Terms
-
Adult
Aged
Anticoagulants/adverse effects/therapeutic use
Aortic Valve/*surgery
Female
Heart Valve Diseases/complications/mortality/*surgery
Heart Valve Prosthesis Implantation/*methods
Hemorrhage/chemically induced/epidemiology
Humans
Intraoperative Complications/mortality
Kidney Failure/etiology
Male
Middle Aged
Mitral Valve/*surgery
Postoperative Complications/mortality
Reoperation
Risk Factors
Severity of Illness Index
Stroke/etiology
Survival Analysis
Thromboembolism/epidemiology
Tricuspid Valve/*surgery
Figure
Cited by 1 articles
-
Long-term Prognosis of Left Ventricular Lead
Seung-Jung Park, Il-Young Oh, Chang-Hwan Yoon, Hyo-Eun Park, Eue-Keun Choi, Gi-Byoung Nam, Kee-June Choi, You-Ho Kim, Yun-Shik Choi, Seil Oh
J Korean Med Sci. 2010;25(10):1462-1466. doi: 10.3346/jkms.2010.25.10.1462.
Reference
-
1. Gersh BJ, Schaff HV, Vatterott PJ, Danielson GK, Orszulak TA, Piehler JM, Puga FJ, Pluth JR, McGoon DC. Results of triple valve replacement in 91 patients: perioperative mortality and long-term follow-up. Circulation. 1985. 72:130–137.
Article2. Carrier M, Pellerin M, Bouchard D, Perrault LP, Cartier R, Hebert Y, Basmadjian A, Page P, Poirier NC. Long-term results with triple valve surgery. Ann Thorac Surg. 2002. 73:44–47.
Article3. Alsoufi B, Rao V, Borger MA, Maganti M, Armstrong S, Feindel CM, Scully HE, David TE. Short- and long-term results of triple valve surgery in the modern era. Ann Thorac Surg. 2006. 81:2172–2177.
Article4. Brown PS Jr, Roberts CS, McIntosh CL, Swain JA, Clark RE. Late results after triple-valve replacement with various substitute valves. Ann Thorac Surg. 1993. 55:502–508.5. Mullany CJ, Gersh BJ, Orszulak TA, Schaff HV, Puga FJ, Ilstrup DM, Pluth JR, Danielson GK. Repair of tricuspid valve insuffiency in patients undergoing double (aortic and mitral) valve replacement. Perioperative mortality and long-term (1 to 20 years) follow-up in 109 patients. J Thorac Cardiovasc Surg. 1987. 94:740–748.6. Akay TH, Gultekin B, Ozkan S, Aslim E, Saritas B, Sezgin A, Aslamaci S. Triple-valve procedures: impact of risk factors on midterm in a rheumatic population. Ann Thorac Surg. 2006. 82:1729–1734.
Article7. Galloway AC, Grossi EA, Baumann FG, LaMendola CL, Crooke GA, Harris LJ, Colvin SB, Spencer FC. Multiple valve operation for advanced valvular heart disease: results and risk factors in 513 patients. J Am Coll Cardiol. 1992. 19:725–732.
Article8. Yilmaz M, Ozkan M, Boke E. Triple valve surgery: a 25-year experience. Anadolu Kardiyol Derg. 2004. 4:205–208.9. Wei J, Chang CY, Lee FY, Lai WY. De Vega's semicircular annuloplasty for tricuspid valve regurgitation. Ann Thorac Surg. 1993. 55:482–485.
Article10. Kaul TK, Mercer JL. Tricuspid valve replacement: factors influencing early and late mortality. Thorac Cardiovasc Surg. 1990. 38:229–235.
Article11. Scully HE, Armstrong CS. Tricuspid valve replacement. Fifteen years of experience with mechanical prosthesis and bioprosthesis. J Thorac Cardiovasc Surg. 1995. 109:1035–1041.12. Emery RW, Krogh CC, Arom KV, Emery AM, Benyo-Albrecht K, Joyce LD, Nicoloff DM. The St. Jude Medical cardiac valve prosthesis: a 25-year experience with single valve replacement. Ann Thorac Surg. 2005. 79:776–782.
Article13. Vesey JM, Otto CM. Complications of prosthetic heart valves. Curr Cardiol Rep. 2004. 6:106–111.
Article14. Edmunds LH Jr, Clark RE, Cohn LH, Grunkemeier GL, Miller DC, Weisel RD. Guidelines for reporting morbidity and mortality after cardiac valvular operations. Ann Thorac Surg. 1996. 62:932–935.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-term Experience with the Bjork-Shiley Monostrut Tilting Disc Valve
- Long Term Clinical Results of Triple Valve Replacement
- Triple High Dose Chemotherapy Followed by Autologous Stem Cell Transplantation for Pediatric Neuroblastoma
- Long-term Results after 1,144 CarboMedics Mechanical Valve Implantation
- Single and Multiple Valve Surgery in Native Valve Infective Endocarditis