J Korean Med Sci.
2009 Jun;24(3):398-402. 10.3346/jkms.2009.24.3.398.
Serum and Pleural Fluid Procalcitonin in Predicting Bacterial Infection in Patients with Parapneumonic Effusion
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, St. Martin De Porres Hospital, Chiayi, Taiwan. wwp750201@yahoo.com.tw
- 2Division of Infectious Disease, Department of Internal Medicine, St. Martin De Porres Hospital, Chiayi, Taiwan.
- 3Division of Laboratory Medicine, St. Martin De Porres Hospital, Chiayi, Taiwan.
- KMID: 1779154
- DOI: http://doi.org/10.3346/jkms.2009.24.3.398
Abstract
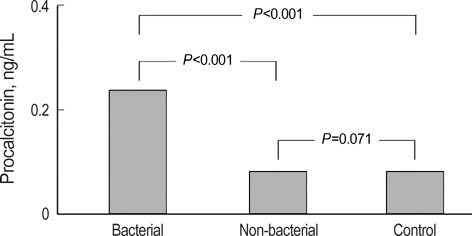
- This study evaluated the value of procalcitonin (PCT) levels in pleural effusion to differentiate the etiology of parapneumonic effusion (PPE). Forty-one consecutive PPE patients were enrolled and were divided into bacterial and non-bacterial PPE. Blood and pleural effusion samples were collected for PCT measurement on admission and analyzed for diagnostic evaluation. PCT of pleural fluid was significantly increased in the bacterial PPE group (0.24 ng/mL) compared to the non-bacterial PPE group (0.09 ng/mL), but there was no significant difference for serum PCT. A PCT concentration of pleural fluid >0.174 ng/mL (best cut-off value) was considered positive for a diagnosis of bacterial PPE (sensitivity, 80%; specificity, 76%; AUC, 0.84). Pleural effusion PCT in the bacterial PPE is significantly different from those of the non-bacterial PPE and control groups, so the diagnostic use of PCT still warrants further investigation.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Value of Procalcitonin and the SAPS II and APACHE III Scores in the Differentiation of Infectious and Non-infectious Fever in the ICU: A Prospective, Cohort Study
Eun Ju Jeon, Jae Woo Jung, Jae Chol Choi, Jong Wook Shin, In Won Park, Byoung Whui Choi, Ae Ja Park, Jae Yeol Kim
J Korean Med Sci. 2010;25(11):1633-1637. doi: 10.3346/jkms.2010.25.11.1633.
Reference
-
1. Light RW, Girard WM, Jenkinson SG, George RB. Parapneumonic effusions. Am J Med. 1980. 69:507–512.
Article2. Dupont H, Mentec H, Sollet JP, Bleichner G. Impact of appropriateness of initial antibiotic therapy on the outcome of ventilator-associated pneumonia. Intensive Care Med. 2001. 27:355–362.
Article3. Ugarte H, Silva E, Mercan D, De Mendonca A, Vincent JL. Procalcitonin used as a marker of infection in the intensive care unit. Crit Care Med. 1999. 27:498–504.
Article4. Wanner GA, Keel M, Steckholzer U, Beier W, Stocker R, Ertel W. Relationship between procalcitonin plasma levels and severity of injury, sepsis, organ failure, and mortality in injured patients. Crit Care Med. 2000. 28:950–957.
Article5. Gendrel D, Raymond J, Coste J, Moulin F, Lorrot M, Guérin S, Ravilly S, Lefèvre H, Royer C, Lacombe C, Palmer P, Bohuon C. Comparison of procalcitonin with C-reactive protein, interleukin 6 and interferon-alpha for differentiation of bacterial vs viral infections. Pediatr Infect Dis J. 1999. 18:875–881.
Article6. Snider RH Jr, Nylen ES, Becker KL. Procalcitonin and its component peptides in systemic inflammation: immunochemical characterization. J Investig Med. 1997. 45:552–560.7. Oberhoffer M, Bögel D, Meier-Hellmann A, Vogelsang H, Reinhart K. Procalcitonin in higher in non-survivors during the clinical course of sepsis, severe sepsis and septic shock. Intensive Care Med (Abstract). 1996. 22:A245.8. Giamarellos-Bourboulis EJ, Grecka P, Poulakou G, Anargyrou K, Katsilambros N, Giamarellou H. Assessment of procalcitonin as a diagnostic marker of underlying infection in patients with febrile neutropenia. Clin Infect Dis. 2001. 32:1718–1725.
Article9. Meisner M, Lohs T, Huttemann E, Schmidt J, Hueller M, Reinhart K. The plasma elimination rate and urinary secretion of procalcitonin in patients with normal and impaired renal function. Eur J Anaesthesiol. 2001. 18:79–87.
Article10. Frederi D, Richard D, Guillaume M, Jacques B, Dominique C, Bernard AL. Alveolar and serum procalcitonin: diagnostic and prognostic value in ventilator-associated pneumonia. Anesthesiology. 2002. 96:74–79.11. Pugin J, Auckenthaler R, Mili N, Janssens JP, Lew PD, Suter PM. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic "blind" bronchoalveolar lavage fluid. Am Rev Respir Dis. 1991. 143:1121–1129.
Article12. Moulin F, Raymond J, Lorrot M, Marc E, Coste J, Iniguez JL, Kalifa G, Bohuon C, Gendrel D. Procalcitonin in children admitted to hospital with community acquired pneumonia. Arch Dis Child. 2001. 84:332–336.
Article13. Dujardin B, Van den Ende J, Van Gompel A, Unger J, Van der Stuyft P. Likelihood ratios: a real improvement for clinical decision making? Eur J Epidemiol. 1994. 10:29–36.
Article14. Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, Coley CM, Marrie TJ, Kapoor WN. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997. 336:243–250.
Article15. Clyne B, Olshaker JS. The C-reactive protein. J Emerg Med. 1999. 17:1019–1025.
Article16. Korppi M, Heiskanen-Kosma T, Leinonen M. White blood cells, C-reactive protein and erythrocyte sedimentation rate in pneumococcal pneumonia in children. Eur Respir J. 1997. 10:1125–1129.
Article17. Nohynek H, Eskola J, Kleemola M, Jalonen E, Saikku P, Leinonen M. Bacterial antibody assays in the diagnosis of acute lower respiratory tract infection in children. Pediatr Infect Dis J. 1995. 14:478–484.
Article18. Tabassian AR, Nylen E, Giron AE, Snider RH, Cassidy MM, Becker KL. Evidence for cigarette smoke-induced calcitonin secretion from lungs of man and hamster. Life Sci. 1988. 42:2323–2329.
Article19. Meisner M, Tschaikowsky K, Hutzler A, Schick C, Schuttler J. Postoperative plasma concentrations of procalcitonin after different types of surgery. Intensive Care Med. 1998. 24:680–684.
Article20. Gendrel D, Raymond J, Assicot M, Moulin F, Iniguez JL, Lebon P, Bohuon C. Measurement of procalcitonin levels in children with bacterial or viral meningitis. Clin Infect Dis. 1997. 24:1240–1242.
Article21. Christ-Crain M, Jaccard-Stolz D, Bingisser R, Gencay MM, Huber PR, Tamm M, Müller B. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blind intervention trial. Lancet. 2004. 363:600–607.22. Kuse ER, Langefeld I, Jaeger K, Kulpmann WR. Procalcitonin: a new diagnostic tool in complications following liver transplantation. Intensive Care Med. 2000. 26:Suppl 2. S187–S192.23. Cakir E, Deniz O, Ozcan O, Tozkoparan E, Yaman H, Akgul EO, Bilgi C, BilgicH , Ekiz K, Erbil MK. Pleural fluid and serum procalcitonin as diagnostic tools in tuberculous pleurisy. Clin Biochem. 2005. 38:234–238.
Article24. Nelson S, Bagby GJ, Bainton BG, Wilson LA, Thompson JJ, Summer WR. Compartmentalization of intraalveolar and systemic lipopolysaccharide-induced tumor necrosis factor and the pulmonary inflammatory response. J Infect Dis. 1989. 159:189–194.
Article25. Monton C, Torres A, El-Ebiary M, Filella X, Xaubet A, de la Bellacasa JP. Cytokines expression in severe pneumonia: a bronchoalveolar lavage study. Crit Care Med. 1999. 27:1745–1753.26. Zeni F, Viallon A, Assicot M, Tardy B, Vindimian M, Page Y, Lafond P, Bertrand JC, Bohuon C. Procalcitonin serum concentrations and severity of sepsis. Clin Intensive Care. 1994. 5:89–98.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Treatment of Complicated Pleural Effusion
- Diagnostic Value of Adenosine Deaminase(ADA) and its Isoenzyme in Pleural Effusion
- Diagnostic Value of Procalcitonin and C-Reactive Protein in Differentiation of Pleural Effusions
- Diagnostic Utility of Pleural Fluid Soluble Triggering Receptor Expressed on Myeloid Cells 1 Protein in Patients with Exudative Pleural Effusion
- Diagnostic Value of LDH and its Isoenzyme in Pleural Effusion