J Korean Med Sci.
2009 Jan;24(Suppl 1):S102-S108. 10.3346/jkms.2009.24.S1.S102.
Status of Initiating Pattern of Hemodialysis: A Multi-center Study
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. drsong@catholic.ac.kr
- KMID: 1778148
- DOI: http://doi.org/10.3346/jkms.2009.24.S1.S102
Abstract
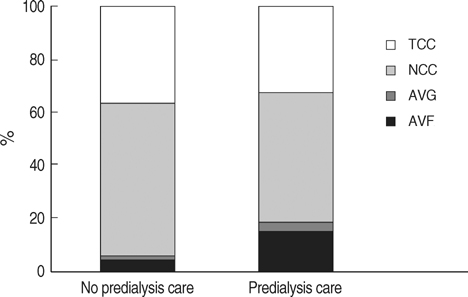
- This study was to evaluate the status of initiating pattern of hemodialysis (HD). Five hundred-three patients in 8 University Hospitals were included. Presentation mode (planned vs. unplanned), and access type (central venous catheters [CVC] vs. permanent access) at initiation of HD were evaluated, and the influence of predialysis care on determining the mode of HD and access type was also assessed. Most patients started unplanned HD (81.9%) and the most common initial access type was CVC (86.3%). The main reason for unplanned HD and high rate of CVC use was patient-related factors such as refusal of permanent access creation and failure to attend scheduled clinic appointments. Predialysis care was performed in 57.9% of patients and only 24.1% of these patients started planned HD and 18.9% used permanent accesses initially. Only a minority of patients initiated planned HD with permanent accesses in spite of predialysis care. To overcome this, efforts to improve the quality of predialysis care are needed.
MeSH Terms
Figure
Cited by 1 articles
-
Improvement of catheter-related outcomes after application of tunneled cuffed hemodialysis catheter insertion without fluoroscopy
Seok Hui Kang, Jun Young Do
Yeungnam Univ J Med. 2020;37(3):186-193. doi: 10.12701/yujm.2019.00465.
Reference
-
1. Vascular Access 2006 Work Group. Clinical practice guidelines for vascular access. Am J Kidney Dis. 2006. 48 Suppl 1:S176–S247.2. Fan PY, Schwab SJ. Vascular access: concepts for the 1990s. J Am Soc Nephrol. 1992. 3:1–11.
Article3. Churchill DN, Taylor DW, Cook RJ, LaPlante P, Barre P, Cartier P, Fay WP, Goldstein MB, Jindal K, Mandin H. Canadian hemodialysis morbidity study. Am J Kidney Dis. 1992. 19:214–234.
Article4. Twardowski ZJ. Percuatenous blood access for hemodialysis. Semin Dial. 1995. 8:175–186.5. Powe NR, Jaar B, Furth SL, Hermann J, Briggs W. Septicemia in dialysis patients: Incidence, risk factors, and prognosis. Kidney Int. 1999. 55:1081–1090.
Article6. Hernandez D, Diaz F, Rufino M, Lorenzo V, Perez T, Rodriguez A, De Bonis E, Losada M, Gonzalez-Posada JM, Torres A. Subclavian vascular access stenosis in dialysis patients: natural history and risk factors. J Am Soc Nephrol. 1998. 9:1507–1510.7. Lorenzo V, Martn M, Rufino M, Hernández D, Torres A, Ayus JC. Predialysis nephrologic care and a functioning arteriovenous fistula at entry are associated with better survival in incident hemodialysis patients: an observational cohort study. Am J Kidney Dis. 2004. 43:999–1007.
Article8. Astor BC, Eustace JA, Powe NR, Klag MJ, Sadler JH, Fink NE, Coresh J. Timing of nephrologist referral and arteriovenous access use: the CHOICE Study. Am J Kidney Dis. 2001. 38:494–501.
Article9. Stehman-Breen CO, Sherrard DJ, Gillen D, Caps M. Determinants of type and timing of initial permanent hemodialysis vascular access. Kidney Int. 2000. 57:639–645.
Article10. Astor BC, Eustace JA, Powe NR, Klag MJ, Fink NE, Coresh J. CHOICE Study. Type of vascular access and survival among incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol. 2005. 16:1449–1455.
Article11. Buck J, Baker R, Cannaby AM, Nicholson S, Peters J, Warwick G. Why do patients known to renal services still undergo urgent dialysis initiation? A cross-sectional survey. Nephrol Dial Transplant. 2007. 22:3240–3245.
Article12. Marrón B, Ortiz A, de Sequera P, Martín-Reyes G, de Arriba G, Lamas JM, Martínez Ocaña JC, Arrieta J, Martínez F. Spanish Group for CKD. Impact of end-stage renal disease care in planned dialysis start and type of renal replacement therapy-a Spanish multicentre experience. Nephrol Dial Transplant. 2006. 21 Supple 2:ii51–ii55.
Article13. Chesser AM, Baker LR. Temporary vascular access for first dialysis is common, undesirable and usually avoidable. Clin Nephrol. 1999. 51:228–232.14. Lee YM, Lee HK, Kwon OK, Jang DS, Lee SY, Lee SJ, Na KR, Lee KW, Shin YT. The clinical impact of the referral pattern to nephrologist in patients with chronic renal failure. Korean J Int Med. 2004. 67:625–634.15. Kang WH, Oh HY, Shin YJ, Seol J, Kang M, Tak EY, Lee NS, Lee M, Ryu R, Song YH, Huh W, Kim YG, Kim DJ. Impact of early nephrology referral on factors correlated with hemodialysis patients' survival. Korean J Nephrol. 2006. 25:243–250.16. Shin SJ, Kim HW, Chung S, Chung HW, Lee SJ, Kim YS, Bang BK, Chang YS, Park CW. Late referral to a nephrologist increases the risk of uremia-related cardiac hypertrophy in patients on hemodialysis. Nephron Clin Pract. 2007. 107:c139–c146.
Article17. Kim SY, Jin DC, Bang BK. Current status of dialytic therapy in Korea. Nephrology (Carlton). 2003. 8 Suppl:S2–S9.
Article18. Lenz O, Sadhu S, Fornoni A, Asif A. Overutilization of central venous catheters in incident hemodialysis patients: reasons and potential resolution strategies. Semin Dial. 2006. 19:543–550.
Article19. Mendelssohn DC, Ethier J, Elder SJ, Saran R, Port FK, Pisoni RL. Haemodialysis vascular access problems in Canada: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS II). Nephrol Dial Transplant. 2006. 21:721–728.
Article20. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimated glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999. 130:461–470.21. Ethier J, Mendelssohn DC, Elder SJ, Hasegawa T, Akizawa T, Akiba T, Canaud BJ, Pisoni RL. Vascular access use and outcomes: an international perspective from the dialysis outcomes and practice patterns study. Nephrol Dial Transplant. 2008. 23:3219–3226.
Article22. Kinchen KS, Sadler J, Fink N, Brookmeyer R, Klag MJ, Levey AS, Powe NR. The timing of specialist evaluation in chronic kidney disease and mortality. Ann Intern Med. 2002. 137:479–486.
Article23. Marrón B, Martínez Ocaña JC, Salgueira M, Barril G, Lamas JM, Martín M, Sierra T, Rodríguez-Carmona A, Soldevilla A, Martínez F. Spanish Group for CKD. Analysis of patient flow into dialysis: role of education in choice of dialysis modality. Perit Dial Int. 2005. 25 Suppl 3:S56–S59.
Article24. McGill RL, Marcus RJ, Healy DA, Brouwer DJ, Smith BC, Sandroni SE. AV fistula rates: changing the culture of vascular access. J Vasc Access. 2005. 6:13–17.
Article25. Goldstein M, Yassa T, Dacouris N, McFarlane P. Multidisciplinary predialysis care and morbidity and mortality of patients on dialysis. Am J Kidney Dis. 2004. 44:706–714.
Article26. Curtis BM, Ravani P, Malberti F, Kennett F, Taylor PA, Djurdjev O, Levin A. The short- and long-term impact of multi-disciplinary clinics in addition to standard nephrology care on patient outcomes. Nephrol Dial Transplant. 2005. 20:147–154.
Article27. Xue JL, Dahl D, Ebben JP, Collins AJ. The association of initial hemodialysis access type with mortality outcomes in elderly Medicare ESRD patients. Am J Kidney Dis. 2003. 42:1013–1019.
Article28. Mendelssohn DC, Toffelmire EB, Levin A. Attitudes of Canadian nephrologists toward multidisciplinary team-based CKD clinic care. Am J Kidney Dis. 2006. 47:277–284.
Article29. Pisoni RL, Young EW, Dykstra DM, Greenwood RN, Hecking E, Gillespie B, Wolfe RA, Goodkin DA, Held PJ. Vascular access use in Europe and the United States: results from the DOPPS. Kidney Int. 2002. 61:305–316.
Article30. Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK. Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int. 2001. 60:1443–1451.
Article31. Pastan S, Soucie JM, McClellan WM. Vascular access and increased risk of death among hemodialysis patients. Kidney Int. 2002. 62:620–626.
Article32. Polkinghorne KR, McDonald SP, Atkins RC, Kerr PG. Vascular access and all-cause mortality: a propensity score analysis. J Am Soc Nephrol. 2004. 15:477–486.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric Hemodialysis
- Study on the Factors Affecting the Sleep Disorder of Hemodialysis Patients
- A Study on the Correlation between Self-efficacy and Self-care in Hemodialysis Patients
- When is the Best Time for the First Hemodialysis after Arteriovenous Fistula?
- A Concept Analysis of Stress in Hemodialysis Patients