J Korean Fract Soc.
2015 Jan;28(1):71-76. 10.12671/jkfs.2015.28.1.71.
Failure to Remove a Trochanteric Entry Femoral Nail and Its Cause in Adolescent Patients: Two Cases Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Daegu Fatima Hospital, Daegu, Korea. nso1020@naver.com
- KMID: 1774100
- DOI: http://doi.org/10.12671/jkfs.2015.28.1.71
Abstract
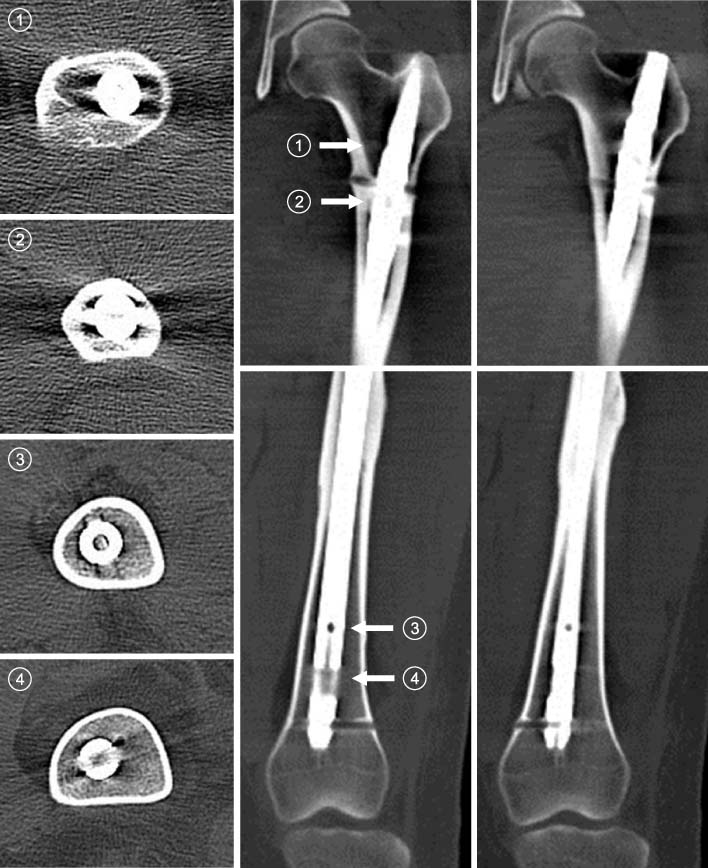
- Trochanteric entry femoral nails have been widely used for fixation of femoral shaft fractures because of easier identification of the entry point. Young patients usually request removal of the nail after healing of the fracture. We experienced a failure and difficulty in removal of the trochanteric entry nail in two adolescent patients. In the patient in which the nail could be removed with difficulty, dense compact bone was formed through the empty interlocking holes and the nail was held just like a latch. This finding was quite similar to the computed tomography findings of the patient in which the nail could not be removed. In order to remove the nail, the newly formed, dense compact bone in the interlocking holes must be broken and detached from the femur itself. We suggest that dense compact bone through the empty interlocking holes might be a clue for difficult removal of the trochanteric entry nail.
Keyword
MeSH Terms
Figure
Reference
-
1. Ricci WM, Schwappach J, Tucker M, et al. Trochanteric versus piriformis entry portal for the treatment of femoral shaft fractures. J Orthop Trauma. 2006; 20:663–667.
Article2. O'Malley DE, Mazur JM, Cummings RJ. Femoral head avascular necrosis associated with intramedullary nailing in an adolescent. J Pediatr Orthop. 1995; 15:21–23.3. Ansari Moein CM, Verhofstad MH, Bleys RL, van der Werken C. Soft tissue injury related to choice of entry point in antegrade femoral nailing: piriform fossa or greater trochanter tip. Injury. 2005; 36:1337–1342.
Article4. Ha SH, Kim WH, Lee GC. Results of intramedullary nailing of femoral shaft fracture: trochanteric entry portal (Sirus Nail) versus Piriformis Entry Portal (M/DN Nail). J Korean Fract Soc. 2014; 27:50–57.
Article5. Seligson D, Howard PA, Martin R. Difficulty in removal of certain intramedullary nails. Clin Orthop Relat Res. 1997; (340):202–206.
Article6. Stafford P, Norris BL, Nowotarski Im PJ. Hardware removal: tips & techniques in revision fracture surgery. Tech Orthop. 2002; 17:522–530.
Article7. Lottes JO. Medullary nailing of the tibia with the triflange nail. Clin Orthop Relat Res. 1974; (105):53–66.
Article8. Takakuwa M, Funakoshi M, Ishizaki K, Aono T, Hamaguchi H. Fracture on removal of the ACE tibial nail. J Bone Joint Surg Br. 1997; 79:444–445.
Article9. Yoo CH, Byun YS, Kim HT, Kim HM, Park YM, Jeon SY. Intraoperative fracture of the tibia associated with removal of the interlocking intramedullary nail: report of 5 cases. J Korean Soc Fract. 1999; 12:538–542.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Results of Intramedullary Nailing of Femoral Shaft Fracture: Trochanteric Entry Portal (Sirus Nail) versus Piriformis Entry Portal (M/DN Nail)
- Pseudoaneurysm of the Superficial Femoral Artery Following Gamma nail Fixation for Trochanteric Fracture: A Case Report
- The Treatment of IM Nailing of Femoral Shaft Fracture: Piriformis Fossa versus Trochanteric Entry Portal
- Comparison of Greater Trochanter Versus Piriformis Entry Nail for Treatment of Femur Shaft Fracture
- The Determination of Optimal Entry Point for Proximal Femoral Nail Antirotation-II by Fluoroscopic Simulation: A Cadaveric Study