J Korean Fract Soc.
2014 Oct;27(4):287-293. 10.12671/jkfs.2014.27.4.287.
Comparison of Greater Trochanter Versus Piriformis Entry Nail for Treatment of Femur Shaft Fracture
- Affiliations
-
- 1Department of Orthopedic Surgery, Korea University Anam Hospital, Seoul, Korea. oshan@korea.ac.kr
- KMID: 2015484
- DOI: http://doi.org/10.12671/jkfs.2014.27.4.287
Abstract
- PURPOSE
The purpose of this study was to compare the clinical outcome of femoral shaft fracture treatment with intramedullary nailing performed using a greater trochanter and a piriformis entry nail.
MATERIALS AND METHODS
A total of 57 patients treated by antegrade nailing for a femoral shaft fracture between January 2008 and April 2013 were included in this study. We evaluated postoperative radiographs of 57 femoral shaft fractures stabilized with femoral intramedullary nailing at a single institutional center. The cases included 25 piriformis fossa entry nails and 32 greater trochanter entry nails. Outcome measures included the alignment, union rate and duration of union, complications, operation time, intra-operative bleeding, and a pain rating scale.
RESULTS
The alignment, union rate, and duration of union did not differ significantly between the groups with piriformis fossa and trochanteric nailing. In addition, no significant differences regarding complications and operation time were observed between the two groups. Less intra-operative bleeding was observed in the trochanteric nailing group. This difference was statistically significant (p=0.044).
CONCLUSION
Use of a femoral nail specially designed for the trochanteric insertion resulted in equally high union rates, duration of union, and low complication rates. Thus, greater trochanter entry nails were similar to conventional antegrade femoral nailing through the piriformis fossa.
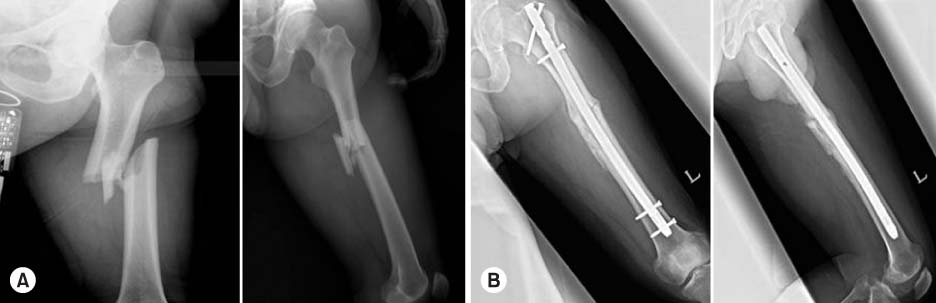
Figure
Reference
-
1. Brumback RJ, Uwagie-Ero S, Lakatos RP, Poka A, Bathon GH, Burgess AR. Intramedullary nailing of femoral shaft fractures. Part II: fracture-healing with static interlocking fixation. J Bone Joint Surg Am. 1988; 70:1453–1462.
Article2. Ricci WM, Gallagher B, Haidukewych GJ. Intramedullary nailing of femoral shaft fractures: current concepts. J Am Acad Orthop Surg. 2009; 17:296–305.
Article3. Winquist RA, Hansen ST Jr, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am. 1984; 66:529–539.
Article4. Gausepohl T, Pennig D, Koebke J, Harnoss S. Antegrade femoral nailing: an anatomical determination of the correct entry point. Injury. 2002; 33:701–705.
Article5. Harper MC, Carson WL. Curvature of the femur and the proximal entry point for an intramedullary rod. Clin Orthop Relat Res. 1987; (220):155–161.
Article6. Miller SD, Burkart B, Damson E, Shrive N, Bray RC. The effect of the entry hole for an intramedullary nail on the strength of the proximal femur. J Bone Joint Surg Br. 1993; 75:202–206.
Article7. Mileski RA, Garvin KL, Crosby LA. Avascular necrosis of the femoral head in an adolescent following intramedullary nailing of the femur. A case report. J Bone Joint Surg Am. 1994; 76:1706–1708.
Article8. Shon OJ, Kim JW, Kim BJ. Updated basic principles of internal fixation of fracture. J Korean Fract Soc. 2013; 26:81–91.
Article9. Karadimas EJ, Papadimitriou G, Theodoratos G, Papanikolaou A, Maris J. The effectiveness of the antegrade reamed technique: the experience and complications from 415 traumatic femoral shaft fractures. Strategies Trauma Limb Reconstr. 2009; 4:113–121.
Article10. Christie J, Court-Brown C, Kinninmonth AW, Howie CR. Intramedullary locking nails in the management of femoral shaft fractures. J Bone Joint Surg Br. 1988; 70:206–210.
Article11. Giannoudis PV, Furlong AJ, Macdonald DA, Smith RM. Reamed against unreamed nailing of the femoral diaphysis: a retrospective study of healing time. Injury. 1997; 28:15–18.
Article12. Tornetta P 3rd, Tiburzi D. Reamed versus nonreamed anterograde femoral nailing. J Orthop Trauma. 2000; 14:15–19.
Article13. Ansari Moein CM, Verhofstad MH, Bleys RL, van der Werken C. Soft tissue injury related to choice of entry point in antegrade femoral nailing: piriform fossa or greater trochanter tip. Injury. 2005; 36:1337–1342.
Article14. Khan FA, Ikram MA, Badr AA, al-Khawashki H. Femoral neck fracture: a complication of femoral nailing. Injury. 1995; 26:319–321.
Article15. Dora C1, Leunig M, Beck M, Rothenfluh D, Ganz R. Entry point soft tissue damage in antegrade femoral nailing: a cadaver study. J Orthop Trauma. 2001; 15:488–493.
Article16. Stannard JP, Bankston L, Futch LA, McGwin G, Volgas DA. Functional outcome following intramedullary nailing of the femur: a prospective randomized comparison of piriformis fossa and greater trochanteric entry portals. J Bone Joint Surg Am. 2011; 93:1385–1391.17. Ha SH, Kim WH, Lee GC. Results of intramedullary nailing of femoral shaft fracture: trochanteric entry portal (Sirus nail) versus piriformis entry portal (M/DN nail). J Korean Fract Soc. 2014; 27:50–57.
Article18. Ricci WM, Schwappach J, Tucker M, et al. Trochanteric versus piriformis entry portal for the treatment of femoral shaft fractures. J Orthop Trauma. 2006; 20:663–667.
Article19. Taitsman LA, Lynch JR, Agel J, Barei DP, Nork SE. Risk factors for femoral nonunion after femoral shaft fracture. J Trauma. 2009; 67:1389–1392.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Results of Intramedullary Nailing of Femoral Shaft Fracture: Trochanteric Entry Portal (Sirus Nail) versus Piriformis Entry Portal (M/DN Nail)
- The Treatment of IM Nailing of Femoral Shaft Fracture: Piriformis Fossa versus Trochanteric Entry Portal
- Treatment of the Femoral Fracture Using Sirus(R) Nail: A Comparison of Complication according to the Entry Potal
- Percutaneous Interlocking Intramedullary Nailing of Femoral Shaft Fracture with Retrograde Guide Wire Insertion Technique
- Bursting Fracture of the Proximal Femur during Insertion of Unreamed Femoral Nail for Femur Shaft Fracture: A Case Report