Yonsei Med J.
2009 Jun;50(3):437-440. 10.3349/ymj.2009.50.3.437.
Long-Surviving Patients with Recurrent GIST after Receiving Cytoreductive Surgery with Imatinib Therapy
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. choish@yuhs.ac
- 2Department of Radiology, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1758574
- DOI: http://doi.org/10.3349/ymj.2009.50.3.437
Abstract
- In the treatment of recurrent or metastatic gastrointestinal stromal tumors (GIST), good prognoses may not be expected by surgery alone. Recently, imatinib has been applied for the treatment of GISTs, resulting in improved patient survival. However, long-term success is limited due to the development of resistance. Herein, we report two cases of long-surviving patients with recurrent GIST after receiving cytoreductive surgery with imatinib therapy. A 49 year-old man was diagnosed to a duodenal GIST with single hepatic metastasis, and an antrectomy including the duodenal lesion with intraoperative radiofrequency ablation were performed in April, 2002. After four months, a new metastatic hepatic lesion was identified. Percutaneous radiofrequency ablation was done, and imatinib therapy was started. A 56 year-old man underwent laparoscopic segmental resection of the distal ileum and partial excision of parietal peritoneum in March, 2001 to treat a malignant GIST of the distal ileum that was attached to parietal peritoneum. After six months, recurrence of GIST with peritoneal seeding and hepatic metastasis was found, and he underwent cytoreductive surgery including right hemicolectomy and wedge resection of liver. After surgery, there was no residual tumor grossly and imatinib therapy was started. In both cases, they were doing well with no evidence of recurrence for 5 years with imatinib therapy. Therefore, in patients with a recurrent GIST, improved survival can be expected with imatinib therapy after cytoreductive surgery.
MeSH Terms
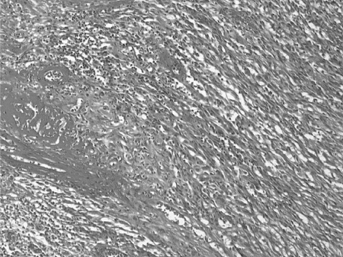
Figure
Cited by 1 articles
-
Successful Resection of Locally Advanced Gastrointestinal Stromal Tumor of the Ampulla of Vater after Treatment with Imatinib
Jeung Eun Park, Seok-Ho Dong, Kun Hyung Cho, Jae Young Jang, Hyo-Jong Kim, Byung-Ho Kim, Young Woon Chang, Rin Chang
Korean J Gastroenterol. 2010;56(1):39-44. doi: 10.4166/kjg.2010.56.1.39.
Reference
-
1. Gold JS, Dematteo RP. combined surgical and molecular therapy: the gastrointestinal stromal tumor model. Ann Surg. 2006. 244:176–184.2. Miettinen M, Lasota J. Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis. Arch Pathol Lab Med. 2006. 130:1466–1478.3. van Oosterom AT, Judson IR, Verweij J, Stroobants S, Dumez H, Donato di Paola E, et al. Update of phase I study of imatinib (STI571) in advanced soft tissue sarcomas and gastrointestinal stromal tumors: a report of the EORTC Soft Tissue and Bone Sarcoma Group. Eur J Cancer. 2002. 38:S83–S87.
Article4. Blanke CD, Rankin C, Demetri GD, Ryan CW, von Mehren M, Benjamin RS, et al. Phase III randomized, intergroup trial assessing imatinib mesylate at two dose levels in patients with unresectable or metastatic gastrointestinal stromal tumors expressing the kit receptor tyrosine kinase: S0033. J Clin Oncol. 2008. 26:626–632.
Article5. Verweij J, Casali PG, Zalcberg J, LeCesne A, Reichardt P, Blay JY, et al. Progression-free survival in gastrointestinal stromal tumours with high-dose imatinib: randomised trial. Lancet. 2004. 364:1127–1134.
Article6. Blanke CD, Demetri GD, von Mehren M, Heinrich MC, Eisenberg B, Fletcher JA, et al. Long-term results from a randomized phase II trial of standard- versus higher-dose imatinib mesylate for patients with unresectable or metastatic gastrointestinal stromal tumors expressing KIT. J Clin Oncol. 2008. 26:620–625.7. Ballarini C, Intra M, Ceretti AP, Prestipino F, Bianchi FM, Sparacio F, et al. Gastrointestinal stromal tumors: a "benign" tumor with hepatic metastasis after 11 years. Tumori. 1998. 84:78–81.
Article8. Miettinen M, El-Rifai W, H L Sobin L, Lasota J. Evaluation of malignancy and prognosis of gastrointestinal stromal tumors: a review. Hum Pathol. 2002. 33:478–483.9. Tamborini E, Bonadiman L, Greco A, Albertini V, Negri T, Gronchi A, et al. A new mutation in the KIT ATP pocket causes acquired resistance to imatinib in a gastrointestinal stromal tumor patient. Gastroenterology. 2004. 127:294–299.
Article10. Chen LL, Sabripour M, Andtbacka RH, Petel SR, Feig BW, Macapinlac HA, et al. Imatinib resistance in gastrointestinal stromal tumors. Curr Oncol Rep. 2005. 7:293–299.
Article11. Debiec-Rychter M, Cools J, Dumez H, Sciot R, Stul M, Mentens N, et al. Mechanisms of resistance to imatinib mesylate in gastrointestinal stromal tumors and activity of the PKC412 inhibitor against imatinib-resistant mutants. Gastroenterology. 2005. 128:270–279.
Article12. Nilsson B, Bümming P, Meis-Kindblom JM, Odén A, Dortok A, Gustavsson B, et al. Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era--a population-based study in western Sweden. Cancer. 2005. 103:821–829.
Article13. Tryggvason G, Gislason HG, Magnússon MK, Jónasson JG. Gastrointestinal stromal tumors in Iceland, 1990-2003: the icelandic GIST study, a population-based incidence and pathologic risk stratification study. Int J Cancer. 2005. 117:289–293.
Article14. Morabito A, De Maio E, Di Maio M, Normanno N, Perrone F. Tyrosine kinase inhibitors of vascular endothelial growth factor receptors in clinical trials: current status and future directions. Oncologist. 2006. 11:753–764.
Article15. Demetri GD, von Mehren M, Blanke CD, Van den Abbeele AD, Eisenberg B, Roberts PJ, et al. Efficacy and Safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002. 347:472–480.
Article16. Haller F, Detken S, Schulten HJ, Happel N, Gunawan B, Kuhlgatz J, et al. Surgical management after neoadjuvant imatinib therapy in gastrointestinal stromal tumours (GISTs) with respect to imatinib resistance caused by secondary KIT mutations. Ann Surg Oncol. 2007. 14:526–532.
Article17. DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000. 231:51–58.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Endoscopic Resection of a Rectal Gastrointestinal Stromal Tumor Larger Than 5 cm
- Adrenal Gland Metastasis of a Gastrointestinal Stromal Tumor
- Successful Resection of Locally Advanced Gastrointestinal Stromal Tumor of the Ampulla of Vater after Treatment with Imatinib
- Imatinib Plasma Monitoring-Guided Dose Modification for Managing Imatinib-Related Toxicities in Gastrointestinal Stromal Tumor Patients
- A Case of Disseminated Intra-abdominal Gastrointestinal Stromal Tumor Managed with Low Dose Imatinib