Korean J Radiol.
2013 Jun;14(3):430-438. 10.3348/kjr.2013.14.3.430.
Endovascular Revascularization for Patients with Critical Limb Ischemia: Impact on Wound Healing and Long Term Clinical Results in 189 Limbs
- Affiliations
-
- 1Department of Radiology, Ajou University School of Medicine, Suwon 443-721, Korea. wonkwak@ajou.ac.kr
- 2Department of Orthopedic Surgery, Ajou University School of Medicine, Suwon 443-721, Korea.
- 3Department of Cardiovascular Surgery, Ajou University School of Medicine, Suwon 443-721, Korea.
- 4DNF Hospital, Seoul 131-875, Korea.
- 5Department of Family Medicine, Busan Paik Hospital, Inje University College of Medicine, Busan 614-735, Korea.
- KMID: 1705455
- DOI: http://doi.org/10.3348/kjr.2013.14.3.430
Abstract
OBJECTIVE
To evaluate the impact on wound healing and long-term clinical outcomes of endovascular revascularization in patients with critical limb ischemia (CLI).
MATERIALS AND METHODS
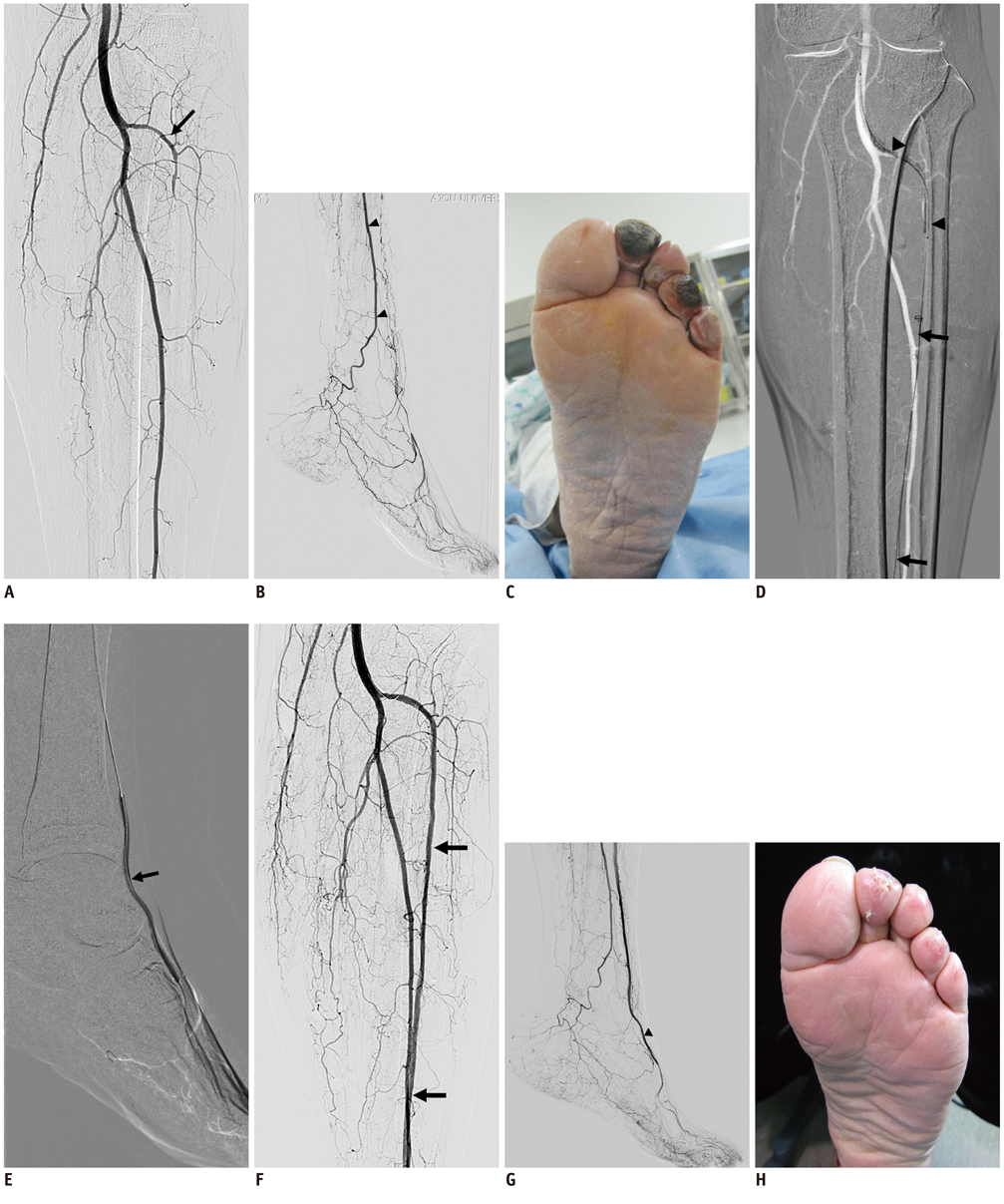
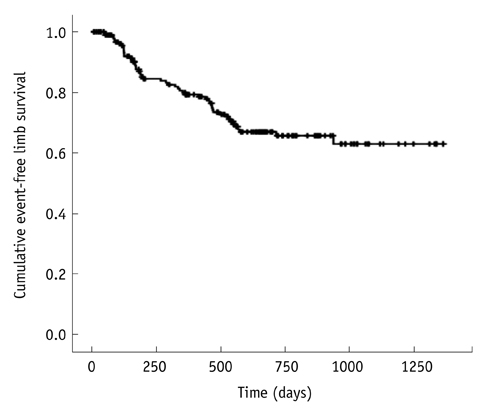
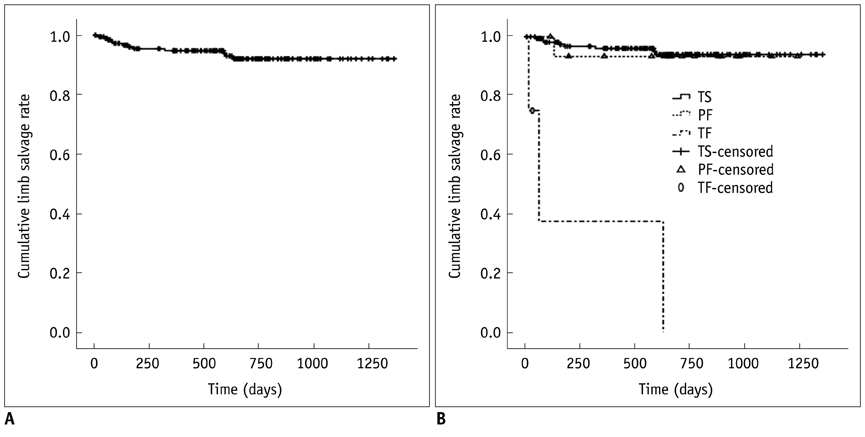
This is a retrospective study on 189 limbs with CLI treated with endovascular revascularization between 2008 and 2010 and followed for a mean 21 months. Angiographic outcome was graded to technical success (TS), partial failure (PF) and complete technical failure. The impact on wound healing of revascularization was assessed with univariate analysis and multivariate logistic regression models. Analysis of long-term event-free limb survival, and limb salvage rate (LSR) was performed by Kaplan-Meier method.
RESULTS
TS was achieved in 89% of treated limbs, whereas PF and CF were achieved in 9% and 2% of the limbs, respectively. Major complications occurred in 6% of treated limbs. The 30-day mortality was 2%. Wound healing was successful in 85% and failed in 15%. Impact of angiographic outcome on wound healing was statistically significant. The event-free limb survival was 79.3% and 69.5% at 1- and 3-years, respectively. The LSR was 94.8% and 92.0% at 1- and 3-years, respectively.
CONCLUSION
Endovascular revascularization improve wound healing rate and provide good long-term LSRs in CLI.
MeSH Terms
Figure
Cited by 2 articles
-
Amputation in Diabetic Foot Ulcer and Infection
Seung Hwan Han, Young Chang Park
J Korean Foot Ankle Soc. 2014;18(1):8-13. doi: 10.14193/jkfas.2014.18.1.8.Statistical Analysis of the Risk Factors for Single Toe Amputation Patients in Wound Healing
Hyung-Jin Chung, Su-Young Bae, Woo-Jin Shin, Jun-Ho Lee
J Korean Foot Ankle Soc. 2019;23(1):18-23. doi: 10.14193/jkfas.2019.23.1.18.
Reference
-
1. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg. 2007. 33:Suppl 1. S1–S75.2. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004. 27:1047–1053.3. Boulton AJ. The diabetic foot: a global view. Diabetes Metab Res Rev. 2000. 16:Suppl 1. S2–S5.4. Faglia E, Dalla Paola L, Clerici G, Clerissi J, Graziani L, Fusaro M, et al. Peripheral angioplasty as the first-choice revascularization procedure in diabetic patients with critical limb ischemia: prospective study of 993 consecutive patients hospitalized and followed between 1999 and 2003. Eur J Vasc Endovasc Surg. 2005. 29:620–627.5. Faglia E, Clerici G, Clerissi J, Mantero M, Caminiti M, Quarantiello A, et al. When is a technically successful peripheral angioplasty effective in preventing above-the-ankle amputation in diabetic patients with critical limb ischaemia? Diabet Med. 2007. 24:823–829.6. Conrad MF, Crawford RS, Hackney LA, Paruchuri V, Abularrage CJ, Patel VI, et al. Endovascular management of patients with critical limb ischemia. J Vasc Surg. 2011. 53:1020–1025.7. Peregrin JH, Koznar B, Kovác J, Lastovicková J, Novotný J, Vedlich D, et al. PTA of infrapopliteal arteries: long-term clinical follow-up and analysis of factors influencing clinical outcome. Cardiovasc Intervent Radiol. 2010. 33:720–725.8. Odink H, van den Berg A, Winkens B. Technical and clinical long-term results of infrapopliteal percutaneous transluminal angioplasty for critical limb ischemia. J Vasc Interv Radiol. 2012. 23:461–467. 467.e19. Giles KA, Pomposelli FB, Spence TL, Hamdan AD, Blattman SB, Panossian H, et al. Infrapopliteal angioplasty for critical limb ischemia: relation of TransAtlantic InterSociety Consensus class to outcome in 176 limbs. J Vasc Surg. 2008. 48:128–136.10. Rutherford RB, Baker JD, Ernst C, Johnston KW, Porter JM, Ahn S, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997. 26:517–538.11. Sacks D, Marinelli DL, Martin LG, Spies JB. Society of Interventional Radiology Technology Assessment Committee. Reporting standards for clinical evaluation of new peripheral arterial revascularization devices. J Vasc Interv Radiol. 2003. 14(9 Pt 2):S395–S404.12. Garbalosa JC, Cavanagh PR, Wu G, Ulbrecht JS, Becker MB, Alexander IJ, et al. Foot function in diabetic patients after partial amputation. Foot Ankle Int. 1996. 17:43–48.13. Jeffcoate WJ, Harding KG. Diabetic foot ulcers. Lancet. 2003. 361:1545–1551.14. Morbach S, Furchert H, Gröblinghoff U, Hoffmeier H, Kersten K, Klauke GT, et al. Long-term prognosis of diabetic foot patients and their limbs: amputation and death over the course of a decade. Diabetes Care. 2012. 35:2021–2027.15. Campbell WB, Ponette D, Sugiono M. Long-term results following operation for diabetic foot problems: arterial disease confers a poor prognosis. Eur J Vasc Endovasc Surg. 2000. 19:174–177.16. Adam DJ, Beard JD, Cleveland T, Bell J, Bradbury AW, Forbes JF, et al. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005. 366:1925–1934.17. Romiti M, Albers M, Brochado-Neto FC, Durazzo AE, Pereira CA, De Luccia N. Meta-analysis of infrapopliteal angioplasty for chronic critical limb ischemia. J Vasc Surg. 2008. 47:975–981.18. Graziani L, Silvestro A, Bertone V, Manara E, Andreini R, Sigala A, et al. Vascular involvement in diabetic subjects with ischemic foot ulcer: a new morphologic categorization of disease severity. Eur J Vasc Endovasc Surg. 2007. 33:453–460.19. Alexandrescu V, Hubermont G, Philips Y, Guillaumie B, Ngongang Ch, Coessens V, et al. Combined primary subintimal and endoluminal angioplasty for ischaemic inferior-limb ulcers in diabetic patients: 5-year practice in a multidisciplinary 'diabetic-foot' service. Eur J Vasc Endovasc Surg. 2009. 37:448–456.20. Conrad MF, Kang J, Cambria RP, Brewster DC, Watkins MT, Kwolek CJ, et al. Infrapopliteal balloon angioplasty for the treatment of chronic occlusive disease. J Vasc Surg. 2009. 50:799–805.e4.21. Faglia E, Mantero M, Caminiti M, Caravaggi C, De Giglio R, Pritelli C, et al. Extensive use of peripheral angioplasty, particularly infrapopliteal, in the treatment of ischaemic diabetic foot ulcers: clinical results of a multicentric study of 221 consecutive diabetic subjects. J Intern Med. 2002. 252:225–232.22. Söder HK, Manninen HI, Jaakkola P, Matsi PJ, Räsänen HT, Kaukanen E, et al. Prospective trial of infrapopliteal artery balloon angioplasty for critical limb ischemia: angiographic and clinical results. J Vasc Interv Radiol. 2000. 11:1021–1031.23. Kudo T, Chandra FA, Ahn SS. The effectiveness of percutaneous transluminal angioplasty for the treatment of critical limb ischemia: a 10-year experience. J Vasc Surg. 2005. 41:423–435. discussion 435.24. Eun CS, Han DS, Park JY, Jeon YC, Hahm JS, Kim KS, et al. Changing pattern of antimicrobial resistance of Helicobacter pylori in Korean patients with peptic ulcer diseases. J Gastroenterol. 2003. 38:436–441.25. Utsunomiya M, Nakamura M, Nakanishi M, Takagi T, Hara H, Onishi K, et al. Impact of wound blush as an angiographic end point of endovascular therapy for patients with critical limb ischemia. J Vasc Surg. 2012. 55:113–121.26. Neville RF, Attinger CE, Bulan EJ, Ducic I, Thomassen M, Sidawy AN. Revascularization of a specific angiosome for limb salvage: does the target artery matter? Ann Vasc Surg. 2009. 23:367–373.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Comprehension and Application of Angiosome Concept in Critical Limb Ischemia
- Advancements in Endovascular Therapy for Chronic Limb-Threatening Ischemia: A Focus on Below-the-Ankle Interventions and Wound Healing Strategies
- RE: Percutaneous Angioplasty in Diabetic Patients with Critical Limb Ischemia
- Endovascular Management for Infrapopliteal Stenocclusive Lesions Manifestating Critical Limb Ischemia
- Evaluation Methods for Foot Perfusion in Critical Limb Ischemia