J Surg Ultrasound.
2021 Nov;8(2):25-31. 10.46268/jsu.2021.8.2.25.
Evaluation Methods for Foot Perfusion in Critical Limb Ischemia
- Affiliations
-
- 1Division of Vascular Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2525877
- DOI: http://doi.org/10.46268/jsu.2021.8.2.25
Abstract
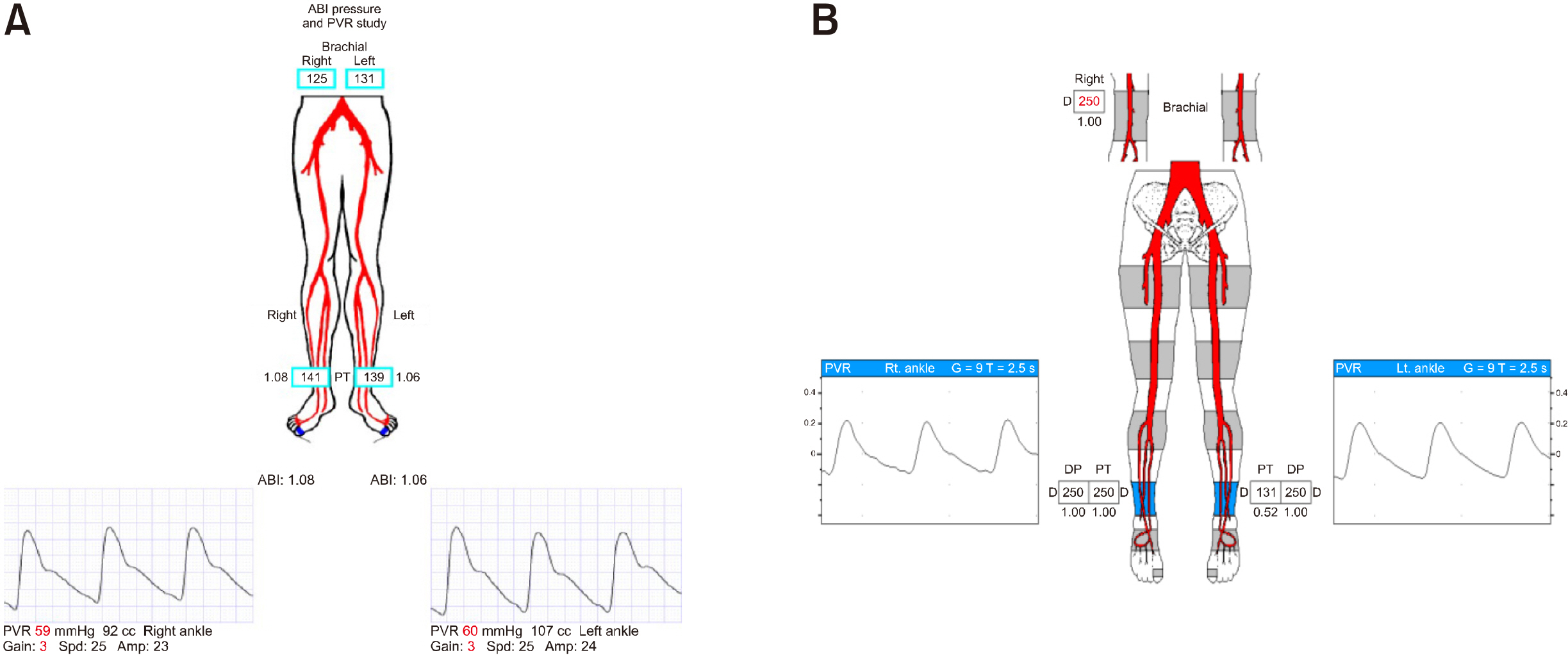
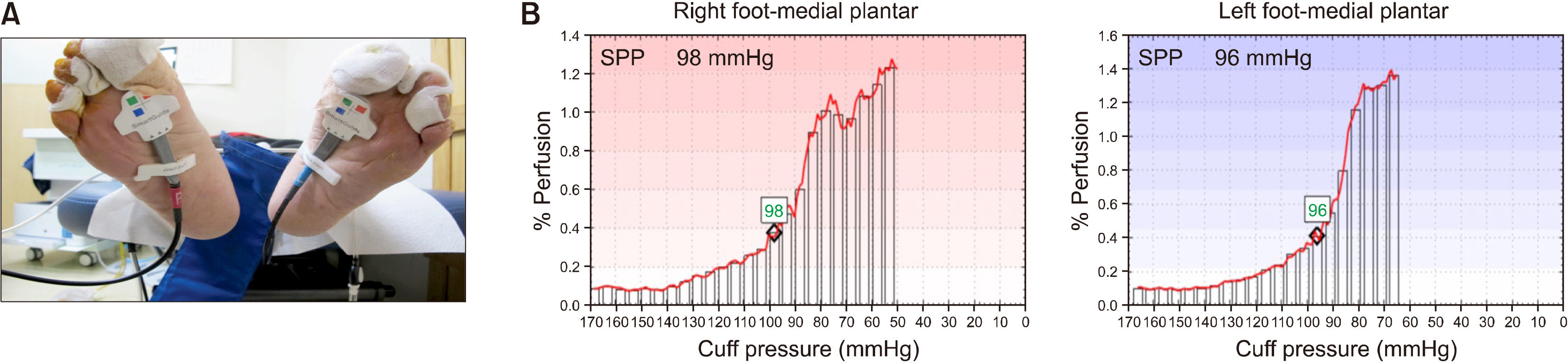
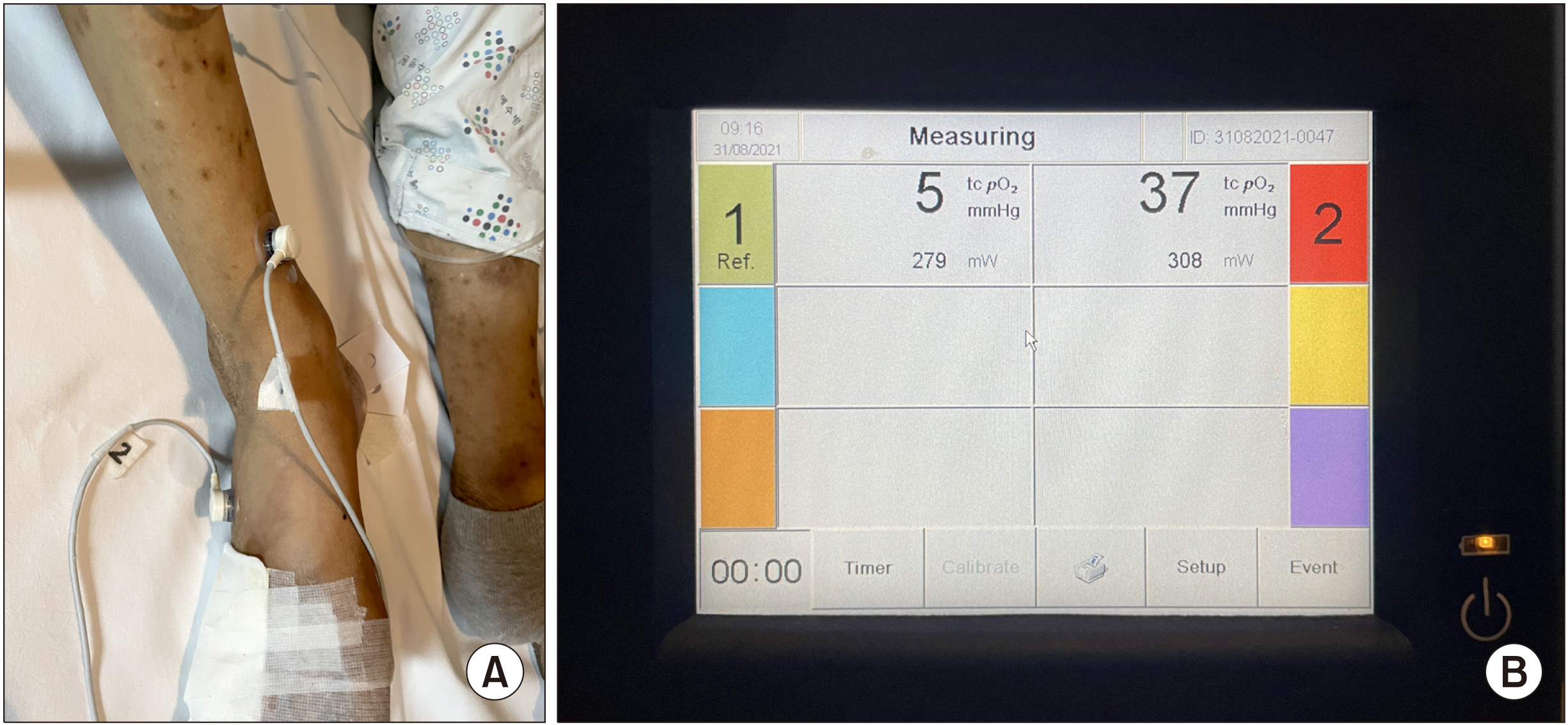
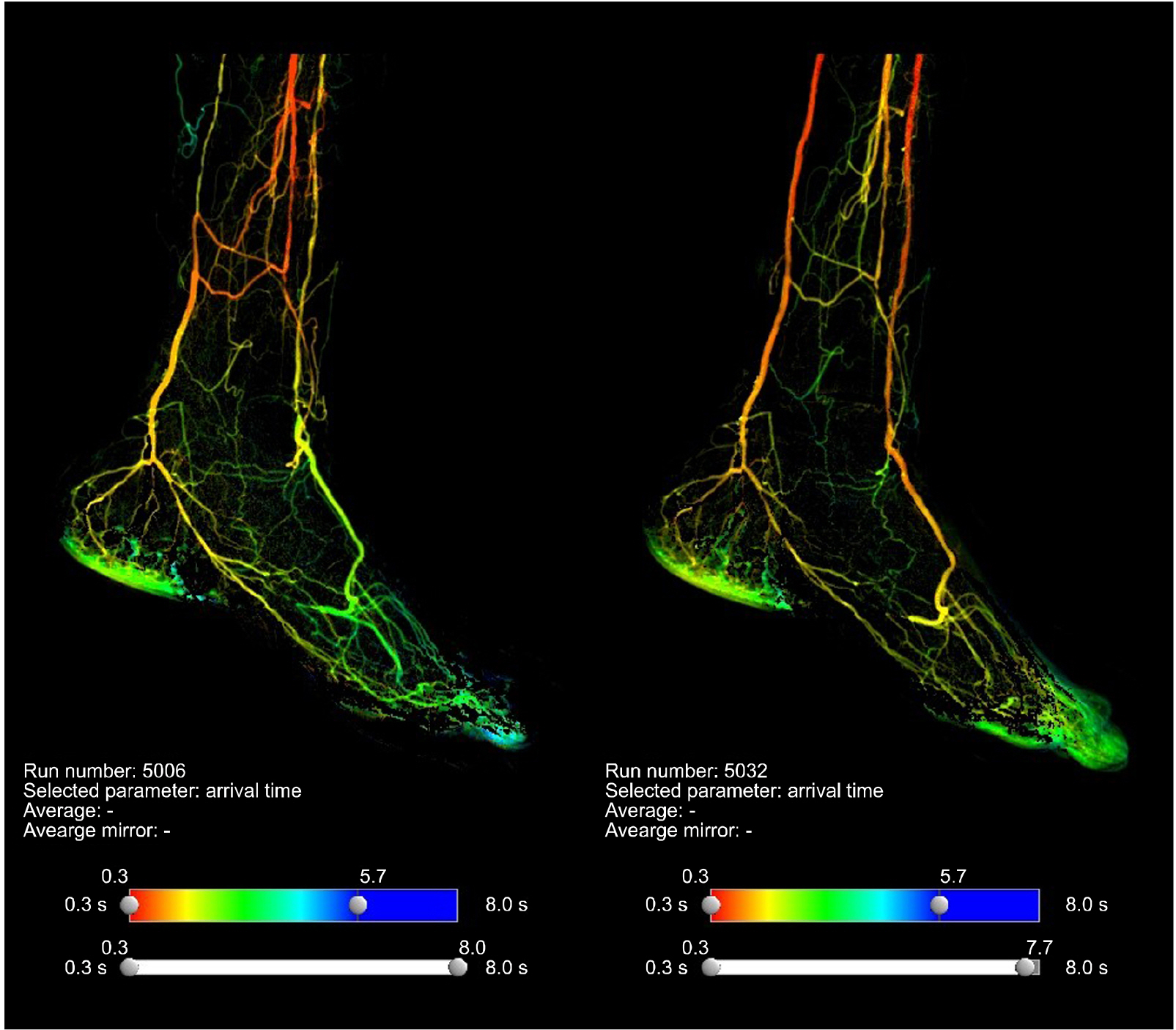
- Critical limb ischemia is a clinical syndrome of ischemic pain at rest or tissue loss resulting from non-healing ulcers or gangrene related to peripheral artery disease. The primary therapeutic goal is to preserve limb function. The most important factor for determining the healing potential of a wound is the degree of perfusion to the affected segment. Several tests objectively measure the degree of tissue perfusion: for example, ankle-brachial index, toe pressure, ultrasound, transcutaneous oxygen pressure, two-dimensional perfusion angiography, indocyanine green angiography, diagnostic nuclear medicine imaging, and laser doppler skin perfusion pressure. In this study, we investigated tests that can measure tissue perfusion and discussed the advantages and limitations of each test.
Figure
Reference
-
1. Kinlay S. 2016; Management of critical limb ischemia. Circ Cardiovasc Interv. 9:e001946. DOI: 10.1161/CIRCINTERVENTIONS.115.001946. PMID: 26858079. PMCID: PMC4827334.
Article2. Misra S, Shishehbor MH, Takahashi EA, Aronow HD, Brewster LP, Bunte MC, et al. 2019; Perfusion assessment in critical limb ischemia: principles for understanding and the development of evidence and evaluation of devices: a scientific statement from the American Heart Association. Circulation. 140:e657–72. DOI: 10.1161/CIR.0000000000000708. PMID: 31401843. PMCID: PMC7372288.
Article3. Shishehbor MH, Bunte MC. 2017; Time to redefine critical limb ischemia. JACC Cardiovasc Interv. 10:2317–9. DOI: 10.1016/j.jcin.2017.09.012. PMID: 29169499.
Article4. Mills JL Sr, Conte MS, Armstrong DG, Pomposelli FB, Schanzer A, Sidawy AN, et al. 2014; The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System: risk stratification based on wound, ischemia, and foot infection (WIfI). J Vasc Surg. 59:220–34.e1. DOI: 10.1016/j.jvs.2013.08.003. PMID: 24126108.
Article5. Taylor GI, Pan WR. 1998; Angiosomes of the leg: anatomic study and clinical implications. Plast Reconstr Surg. 102:599–616. discussion 617–8. DOI: 10.1097/00006534-199809010-00001. PMID: 9727424.
Article6. Attinger CE, Evans KK, Bulan E, Blume P, Cooper P. 2006; Angiosomes of the foot and ankle and clinical implications for limb salvage: reconstruction, incisions, and revascularization. Plast Reconstr Surg. 117(7 Suppl):261S–93S. DOI: 10.1097/01.prs.0000222582.84385.54. PMID: 16799395.
Article7. Hardman RL, Jazaeri O, Yi J, Smith M, Gupta R. 2014; Overview of classification systems in peripheral artery disease. Semin Intervent Radiol. 31:378–88. DOI: 10.1055/s-0034-1393976. PMID: 25435665. PMCID: PMC4232437.
Article8. Benitez E, Sumpio BJ, Chin J, Sumpio BE. 2014; Contemporary assessment of foot perfusion in patients with critical limb ischemia. Semin Vasc Surg. 27:3–15. DOI: 10.1053/j.semvascsurg.2014.12.001. PMID: 25812754.
Article9. Aboyans V, Criqui MH, Abraham P, Allison MA, Creager MA, Diehm C, et al. 2012; Measurement and interpretation of the ankle-brachial index: a scientific statement from the American Heart Association. Circulation. 126:2890–909. DOI: 10.1161/CIR.0b013e318276fbcb. PMID: 23159553.
Article10. Tyrrell MR, Wolfe JH. 1993; Critical leg ischaemia: an appraisal of clinical definitions. Joint Vascular Research Group. Br J Surg. 80:177–80. DOI: 10.1002/bjs.1800800214. PMID: 8443643.11. Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, et al. 2019; Global vascular guidelines on the management of chronic limb-threatening ischemia. Eur J Vasc Endovasc Surg. 58(1S):S1–S109.e33. DOI: 10.1016/j.ejvs.2019.05.006. PMID: 31182334. PMCID: PMC8369495.12. Bunte MC, Shishehbor MH. 2013; Treatment of infrapopliteal critical limb ischemia in 2013: the wound perfusion approach. Curr Cardiol Rep. 15:363. DOI: 10.1007/s11886-013-0363-5. PMID: 23605465.
Article13. Kimura T, Watanabe Y, Tokuoka S, Nagashima F, Ebisudani S, Inagawa K. 2019; Utility of skin perfusion pressure values with the Society for Vascular Surgery Wound, Ischemia, and foot Infection classification system. J Vasc Surg. 70:1308–17. DOI: 10.1016/j.jvs.2019.01.045. PMID: 31113720.
Article14. Lo T, Sample R, Moore P, Gold P. 2009; Prediction of wound healing outcome using skin perfusion pressure and transcutaneous oximetry: a single-center experience in 100 patients. Wounds. 21:310–6. PMID: 25902775.15. Fife CE, Smart DR, Sheffield PJ, Hopf HW, Hawkins G, Clarke D. 2009; Transcutaneous oximetry in clinical practice: consensus statements from an expert panel based on evidence. Undersea Hyperb Med. 36:43–53. PMID: 19341127.16. Rogers RK, Montero-Baker M, Biswas M, Morrison J, Braun J. 2020; Assessment of foot perfusion: overview of modalities, review of evidence, and identification of evidence gaps. Vasc Med. 25:235–45. DOI: 10.1177/1358863X20909433. PMID: 32362209.
Article17. Kaur S, Pawar M, Banerjee N, Garg R. 2012; Evaluation of the efficacy of hyperbaric oxygen therapy in the management of chronic nonhealing ulcer and role of periwound transcutaneous oximetry as a predictor of wound healing response: a randomized prospective controlled trial. J Anaesthesiol Clin Pharmacol. 28:70–5. DOI: 10.4103/0970-9185.92444. PMID: 22345950. PMCID: PMC3275977.
Article18. Catella J, Long A, Mazzolai L. 2021; What is currently the role of TcPO2 in the choice of the amputation level of lower limbs? A comprehensive review. J Clin Med. 10:1413. DOI: 10.3390/jcm10071413. PMID: 33915838. PMCID: PMC8037184.
Article19. Wisniewski NA, Nichols SP, Gamsey SJ, Pullins S, Au-Yeung KY, Klitzman B, et al. 2017; Tissue-integrating oxygen sensors: continuous tracking of tissue hypoxia. Adv Exp Med Biol. 977:377–83. DOI: 10.1007/978-3-319-55231-6_49. PMID: 28685468. PMCID: PMC5657483.
Article20. Kanick SC, Schneider PA, Klitzman B, Wisniewski NA, Rebrin K. 2019; Continuous monitoring of interstitial tissue oxygen using subcutaneous oxygen microsensors: in vivo characterization in healthy volunteers. Microvasc Res. 124:6–18. DOI: 10.1016/j.mvr.2019.02.002. PMID: 30742844. PMCID: PMC6570499.
Article21. Rehman AU, Qureshi SA. 2021; A review of the medical hyperspectral imaging systems and unmixing algorithms' in biological tissues. Photodiagnosis Photodyn Ther. 33:102165. DOI: 10.1016/j.pdpdt.2020.102165. PMID: 33383204.
Article22. Sicher C, Rutkowski R, Lutze S, von Podewils S, Wild T, Kretching M, et al. 2018; Hyperspectral imaging as a possible tool for visualization of changes in hemoglobin oxygenation in patients with deficient hemodynamics - proof of concept. Biomed Tech (Berl). 63:609–16. DOI: 10.1515/bmt-2017-0084. PMID: 30210054.
Article23. Crawford JD, Robbins NG, Harry LA, Wilson DG, McLafferty RB, Mitchell EL, et al. 2016; Characterization of tibial velocities by duplex ultrasound in severe peripheral arterial disease and controls. J Vasc Surg. 63:646–51. DOI: 10.1016/j.jvs.2015.08.112. PMID: 26620716.
Article24. Wilson DG, Harris SK, Barton C, Crawford JD, Azarbal AF, Jung E, et al. 2018; Tibial artery duplex ultrasound-derived peak systolic velocities may be an objective performance measure after above-knee endovascular therapy for arterial stenosis. J Vasc Surg. 68:481–6. DOI: 10.1016/j.jvs.2017.11.092. PMID: 29523435.
Article25. Sommerset J, Karmy-Jones R, Dally M, Feliciano B, Vea Y, Teso D. 2019; Plantar acceleration time: a novel technique to evaluate arterial flow to the foot. Ann Vasc Surg. 60:308–14. DOI: 10.1016/j.avsg.2019.03.002. PMID: 31075481.
Article26. Yoneyama F, Osaka M, Sato F, Sakamoto H, Hiramatsu Y. 2018; Efficacy of two-dimensional perfusion angiography for evaluations after infrapopliteal bypass surgery for critical limb ischemia. Ann Vasc Dis. 11:248–51. DOI: 10.3400/avd.hdi.17-00137. PMID: 30116421. PMCID: PMC6094036.
Article27. Braun JD, Trinidad-Hernandez M, Perry D, Armstrong DG, Mills JL Sr. 2013; Early quantitative evaluation of indocyanine green angiography in patients with critical limb ischemia. J Vasc Surg. 57:1213–8. DOI: 10.1016/j.jvs.2012.10.113. PMID: 23352361.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- RE: Percutaneous Angioplasty in Diabetic Patients with Critical Limb Ischemia
- Clinical Comprehension and Application of Angiosome Concept in Critical Limb Ischemia
- Peripheral Transluminal Angioplasty for Limb Salvage in Critical Limb Ischemia in an Old Cerebral Infarction with Multiple Contractures
- Safety and Efficacy of Distal Perfusion Catheterization to Prevent Limb Ischemia after Common Femoral Artery Cannulation for Extracorporeal Membrane Oxygenation
- Endovascular Management for Infrapopliteal Stenocclusive Lesions Manifestating Critical Limb Ischemia