Yonsei Med J.
2013 Mar;54(2):381-388. 10.3349/ymj.2013.54.2.381.
The Role of One-Year Endoscopic Follow-Up for the Esophageal Remnant and Gastric Conduit after Esophagectomy with Gastric Reconstruction for Esophageal Squamous Cell Carcinoma
- Affiliations
-
- 1Center for Lung Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea. thoracic@ncc.re.kr
- 2Cancer Biostatistics Branch, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
- 3Department of Thoracic and Cardiovascular Surgery, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Systems Biology, The University of Texas MD Anderson Cancer Center, TX, USA.
- 5Department of Thoracic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1503900
- DOI: http://doi.org/10.3349/ymj.2013.54.2.381
Abstract
- PURPOSE
After esophagectomy and gastric reconstruction for esophageal cancer, patients suffer from various symptoms that can detract from quality of life. Endoscopy is a useful diagnostic tool for evaluating patients after esophagectomy. This observational study was performed to investigate the correlation between symptoms and endoscopic findings one year after esophageal surgery and to assess the clinical usefulness of one-year endoscopic follow-up.
MATERIALS AND METHODS
From 2001 to 2008, 162 patients who underwent esophagectomy with gastric reconstruction were endoscopically examined one year after operation.
RESULTS
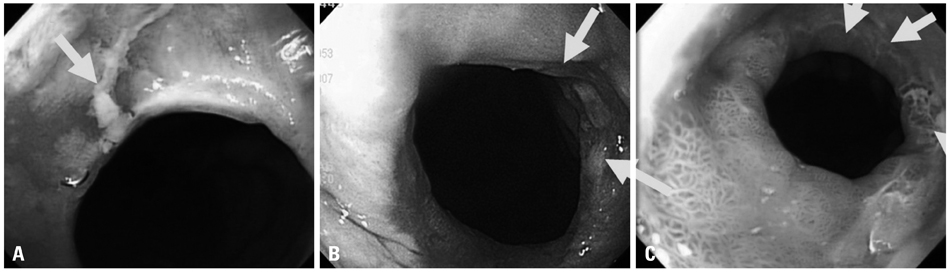
Patients suffered from the following symptoms: nocturnal cough (n=10), regurgitation (n=7), cervical heartburn (n=3), lump sensation (n=2), dysphagia (n=20) and odynophagia (n=22). Eighty-five (52.5%) patients had abnormal findings on endoscopic examination. Twelve (7.4%) patients had reflux esophagitis, and 37 (22.8%) patients had an anastomotic stricture. Only stricture-related symptoms were correlated with the finding of anastomotic strictures (p<0.001). Two patients had recurrences at the anastomotic sites, and four patients had regional lymph node recurrences with gastric conduit invasion visualized by endoscopy. Newly-developed malignancies in the esophageal remnant or hypopharynx that were not detected by clinical symptoms and imaging studies were reported in two patients.
CONCLUSION
One year after esophagectomy, endoscopic findings were not correlated with clinical symptoms, except those related to stricture. Routine endoscopic follow-up is a useful tool for identifying latent functional and oncological lesions.
MeSH Terms
-
Anastomosis, Surgical
Carcinoma, Squamous Cell/pathology/*surgery
Esophageal Neoplasms/pathology/*surgery
Esophagectomy/*adverse effects
Follow-Up Studies
Humans
Neoplasm Recurrence, Local/diagnosis/epidemiology
Postoperative Complications/*diagnosis/epidemiology
Reconstructive Surgical Procedures
Retrospective Studies
Figure
Cited by 1 articles
-
Optimal Adjuvant Treatment for Curatively Resected Thoracic Esophageal Squamous Cell Carcinoma: A Radiotherapy Perspective
Kyung Hwan Kim, Jee Suk Chang, Ji Hye Cha, Ik Jae Lee, Dae Joon Kim, Byoung Chul Cho, Kyung Ran Park, Chang Geol Lee
Cancer Res Treat. 2017;49(1):168-177. doi: 10.4143/crt.2016.142.
Reference
-
1. McLarty AJ, Deschamps C, Trastek VF, Allen MS, Pairolero PC, Harmsen WS. Esophageal resection for cancer of the esophagus: long-term function and quality of life. Ann Thorac Surg. 1997. 63:1568–1572.
Article2. Yuasa N, Sasaki E, Ikeyama T, Miyake H, Nimura Y. Acid and duodenogastroesophageal reflux after esophagectomy with gastric tube reconstruction. Am J Gastroenterol. 2005. 100:1021–1027.
Article3. Johansson J, Oberg S, Wenner J, Zilling T, Johnsson F, von Holstein CS, et al. Impact of proton pump inhibitors on benign anastomotic stricture formations after esophagectomy and gastric tube reconstruction: results from a randomized clinical trial. Ann Surg. 2009. 250:667–673.
Article4. Motoyama S, Saito R, Kitamura M, Suzuki H, Nakamura M, Okuyama M, et al. Prospective endoscopic follow-up results of reconstructed gastric tube. Hepatogastroenterology. 2003. 50:666–669.5. Lee HS, Kim MS, Lee JM, Kim SK, Kang KW, Zo JI. Intrathoracic gastric emptying of solid food after esophagectomy for esophageal cancer. Ann Thorac Surg. 2005. 80:443–447.
Article6. Armstrong D. Endoscopic evaluation of gastro-esophageal reflux disease. Yale J Biol Med. 1999. 72:93–100.7. Gutschow C, Collard JM, Romagnoli R, Salizzoni M, Hölscher A. Denervated stomach as an esophageal substitute recovers intraluminal acidity with time. Ann Surg. 2001. 233:509–514.
Article8. Shibuya S, Fukudo S, Shineha R, Miyazaki S, Miyata G, Sugawara K, et al. High incidence of reflux esophagitis observed by routine endoscopic examination after gastric pull-up esophagectomy. World J Surg. 2003. 27:580–583.
Article9. Bemelman WA, Verburg J, Brummelkamp WH, Klopper PJ. A physical model of the intrathoracic stomach. Am J Physiol. 1988. 254(2 Pt 1):G168–G175.
Article10. Matsubara T, Ueda M, Kaisaki S, Kuroda J, Uchida C, Kokudo N, et al. Localization of initial lymph node metastasis from carcinoma of the thoracic esophagus. Cancer. 2000. 89:1869–1873.
Article11. D'Journo XB, Martin J, Rakovich G, Brigand C, Gaboury L, Ferraro P, et al. Mucosal damage in the esophageal remnant after esophagectomy and gastric transposition. Ann Surg. 2009. 249:262–268.12. Rice TW, Goldblum JR, Rybicki LA, Rajeswaran J, Murthy SC, Mason DP, et al. Fate of the esophagogastric anastomosis. J Thorac Cardiovasc Surg. 2011. 141:875–880.
Article13. Orringer MB, Marshall B, Iannettoni MD. Eliminating the cervical esophagogastric anastomotic leak with a side-to-side stapled anastomosis. J Thorac Cardiovasc Surg. 2000. 119:277–288.
Article14. Williams VA, Watson TJ, Zhovtis S, Gellersen O, Raymond D, Jones C, et al. Endoscopic and symptomatic assessment of anastomotic strictures following esophagectomy and cervical esophagogastrostomy. Surg Endosc. 2008. 22:1470–1476.
Article15. Kim HK, Choi YH, Shim JH, Cho YH, Baek MJ, Sohn YS, et al. Endoscopic evaluation of the quality of the anastomosis after esophagectomy with gastric tube reconstruction. World J Surg. 2008. 32:2010–2014.
Article16. Orringer MB, Marshall B, Iannettoni MD. Transhiatal esophagectomy: clinical experience and refinements. Ann Surg. 1999. 230:392–400.
Article17. Orringer MB, Lemmer JH. Early dilation in the treatment of esophageal disruption. Ann Thorac Surg. 1986. 42:536–539.
Article18. Ali T, Roberts DN, Tierney WM. Long-term safety concerns with proton pump inhibitors. Am J Med. 2009. 122:896–903.
Article19. Eom CS, Park SM, Myung SK, Yun JM, Ahn JS. Use of acid-suppressive drugs and risk of fracture: a meta-analysis of observational studies. Ann Fam Med. 2011. 9:257–267.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Total Gastrectomy in Gastric Conduit Cancer
- Endoscopic Treatment for Esophageal Cancer
- Perforation of a Gastric Tear during Esophageal Endoscopic Submucosal Dissection under General Anesthesia
- Reflux Following Esophagectomy for Esophageal Cancer
- Long-Term Outcomes of Colon Conduits in Surgery for Primary Esophageal Cancer: A Propensity Score-Matched Comparison to Gastric Conduits