J Cardiovasc Ultrasound.
2013 Sep;21(3):123-129. 10.4250/jcu.2013.21.3.123.
Prediction of Hemorrhagic Transformation Following Embolic Stroke in Patients with Prosthetic Valve Endocarditis
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Yonsei University Health System, Seoul, Korea. hjchang@yuhs.ac
- 2Division of Cardiology, Bundang CHA Medical Center, CHA University, Seongnam, Korea.
- 3Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea.
- 4Division of Cardiology, Seoul National University College of Medicine, Seoul, Korea.
- 5Division of Cardiology, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Division of Cardiology, Pusan National University Hospital, Busan, Korea.
- KMID: 1500191
- DOI: http://doi.org/10.4250/jcu.2013.21.3.123
Abstract
- BACKGROUND
Hemorrhagic transformation (HT) of stroke is a disastrous complication in patients with infective endocarditis (IE). In patients with mechanical heart valves complicated by IE, physicians struggle with the appropriateness of anticoagulation administration given the risk of thromboembolism and HT of stroke. In this study, we aimed to define predictive parameters of HT of stroke in patients with prosthetic valve endocarditis (PVE).
METHODS
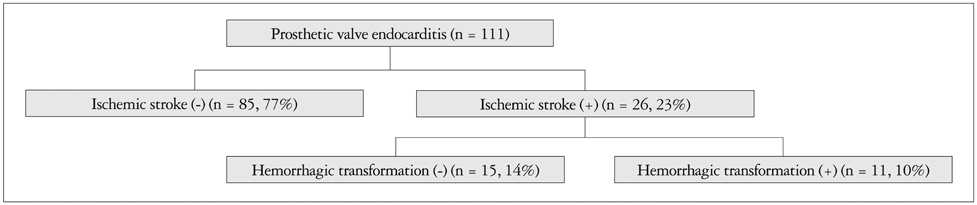
This study was a multicenter, retrospective design. We recruited from 7 institutions a total of 111 patients diagnosed with PVE during May, 2011 to April, 2012.
RESULTS
Complication of stroke was seen in 26/111 patients (23%), and HT of stroke was seen in 11/111 patients (10%). Most patients with HT (9/11, 82%) had supratherapeutic prothrombin times. However, there were no significant differences in clinical and laboratory values between PVE patients without stroke and those patients who had a stroke and with or without concurrent HT. Furthermore, echocardiographic parameters also did not show significant between-group differences.
CONCLUSION
Even though this was a multicenter study, a limited number of patients was identified and may explain the negative results seen here. However, a large number of PVE patients with stroke also developed HT. Therefore, further studies to define predictive parameters of HT should be implemented in a larger population.
MeSH Terms
Figure
Reference
-
1. Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr, Bolger AF, Levison ME, Ferrieri P, Gerber MA, Tani LY, Gewitz MH, Tong DC, Steckelberg JM, Baltimore RS, Shulman ST, Burns JC, Falace DA, Newburger JW, Pallasch TJ, Takahashi M, Taubert KA. Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease. Council on Cardiovascular Disease in the Young. Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia. American Heart Association. Infectious Diseases Society of America. Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association Association: endorsed by the Infectious Diseases Society of America. Circulation. 2005; 111:e394–e434.2. Okada Y, Yamaguchi T, Minematsu K, Miyashita T, Sawada T, Sadoshima S, Fujishima M, Omae T. Hemorrhagic transformation in cerebral embolism. Stroke. 1989; 20:598–603.
Article3. Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, Grubb RL, Higashida RT, Jauch EC, Kidwell C, Lyden PD, Morgenstern LB, Qureshi AI, Rosenwasser RH, Scott PA, Wijdicks EF. American Heart Association. American Stroke Association Stroke Council. Clinical Cardiology Council. Cardiovascular Radiology and Intervention Council. Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007; 38:1655–1711.
Article4. Lodder J, Krijne-Kubat B, Broekman J. Cerebral hemorrhagic infarction at autopsy: cardiac embolic cause and the relationship to the cause of death. Stroke. 1986; 17:626–629.
Article5. Hallevi H, Albright KC, Martin-Schild S, Barreto AD, Savitz SI, Escobar MA, Gonzales NR, Noser EA, Illoh K, Grotta JC. Anticoagulation after cardioembolic stroke: to bridge or not to bridge? Arch Neurol. 2008; 65:1169–1173.6. Aviv RI, d'Esterre CD, Murphy BD, Hopyan JJ, Buck B, Mallia G, Li V, Zhang L, Symons SP, Lee TY. Hemorrhagic transformation of ischemic stroke: prediction with CT perfusion. Radiology. 2009; 250:867–877.
Article7. Salem DN, Daudelin HD, Levine HJ, Pauker SG, Eckman MH, Riff J. Antithrombotic therapy in valvular heart disease. Chest. 2001; 119:1 Suppl. 207S–219S.
Article8. Davenport J, Hart RG. Prosthetic valve endocarditis 1976-1987. Antibiotics, anticoagulation, and stroke. Stroke. 1990; 21:993–999.
Article9. Piechowski-Jóźwiak B, Bogousslavsky J. Infectious endocarditis and stroke: any lessons learned since William Osler's Gulstonian lectures? Neurology. 2003; 61:1324–1325.10. Ulrich JN, Hesse B, Schuele S, Vlassak I, Sila CA, Jaber WA. Single-vessel versus multivessel territory acute ischemic stroke: value of transesophageal echocardiography in the differentiation of embolic stroke. J Am Soc Echocardiogr. 2006; 19:1165–1169.
Article11. Fiorelli M, Bastianello S, von Kummer R, del Zoppo GJ, Larrue V, Lesaffre E, Ringleb AP, Lorenzano S, Manelfe C, Bozzao L. Hemorrhagic transformation within 36 hours of a cerebral infarct: relationships with early clinical deterioration and 3-month outcome in the European Cooperative Acute Stroke Study I (ECASS I) cohort. Stroke. 1999; 30:2280–2284.
Article12. Ruttmann E, Willeit J, Ulmer H, Chevtchik O, Höfer D, Poewe W, Laufer G, Müller LC. Neurological outcome of septic cardioembolic stroke after infective endocarditis. Stroke. 2006; 37:2094–2099.
Article13. Paciaroni M, Agnelli G, Micheli S, Caso V. Efficacy and safety of anticoagulant treatment in acute cardioembolic stroke: a meta-analysis of randomized controlled trials. Stroke. 2007; 38:423–430.
Article14. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994; 96:200–209.
Article15. Anguera I, Miro JM, Vilacosta I, Almirante B, Anguita M, Muñoz P, Roman JA, de Alarcon A, Ripoll T, Navas E, Gonzalez-Juanatey C, Cabell CH, Sarria C, Garcia-Bolao I, Fariñas MC, Leta R, Rufi G, Miralles F, Pare C, Evangelista A, Fowler VG Jr, Mestres CA, de Lazzari E, Guma JR. Aorto-cavitary Fistula in Endocarditis Working Group. Aorto-cavitary fistulous tract formation in infective endocarditis: clinical and echocardiographic features of 76 cases and risk factors for mortality. Eur Heart J. 2005; 26:288–297.
Article16. Sanfilippo AJ, Picard MH, Newell JB, Rosas E, Davidoff R, Thomas JD, Weyman AE. Echocardiographic assessment of patients with infectious endocarditis: prediction of risk for complications. J Am Coll Cardiol. 1991; 18:1191–1199.
Article17. Derex L, Bonnefoy E, Delahaye F. Impact of stroke on therapeutic decision making in infective endocarditis. J Neurol. 2010; 257:315–321.
Article18. Røder BL, Wandall DA, Espersen F, Frimodt-Møller N, Skinhøj P, Rosdahl VT. Neurologic manifestations in Staphylococcus aureus endocarditis: a review of 260 bacteremic cases in nondrug addicts. Am J Med. 1997; 102:379–386.
Article19. Tornos P, Almirante B, Mirabet S, Permanyer G, Pahissa A, Soler-Soler J. Infective endocarditis due to Staphylococcus aureus: deleterious effect of anticoagulant therapy. Arch Intern Med. 1999; 159:473–475.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hemorrhagic Transformation of Ischemic Stroke: Severe Complications of Prosthetic Valve Endocarditis
- Use of a Valved-Conduit for Exclusion of the Infected Portion in the Prosthetic Pulmonary Valve Endocarditis
- Successful Medical Treatment of Prosthetic Mitral Valve Endocarditis Caused by Brucella abortus
- A Case Report of Surgical Management of Tricuswpid Valve Endocarditis
- Infective Endocarditis due to Streptococcus Agalactiae in Young and Immunocompetent Woman: A Case of Structurally Normal Valve Endocarditis Presented with Major Stroke