Therapeutic Efficacy and Safety of Percutaneous Ethanol Injection with or without Combined Radiofrequency Ablation for Hepatocellular Carcinomas in High Risk Locations
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea. leeminwoo0@gmail.com
- KMID: 1482783
- DOI: http://doi.org/10.3348/kjr.2013.14.2.240
Abstract
OBJECTIVE
To evaluate the therapeutic efficacy and safety of percutaneous ethanol injection (PEI) alone and combined with radiofrequency ablation (RFA) for hepatocellular carcinomas (HCCs) in high risk locations.
MATERIALS AND METHODS
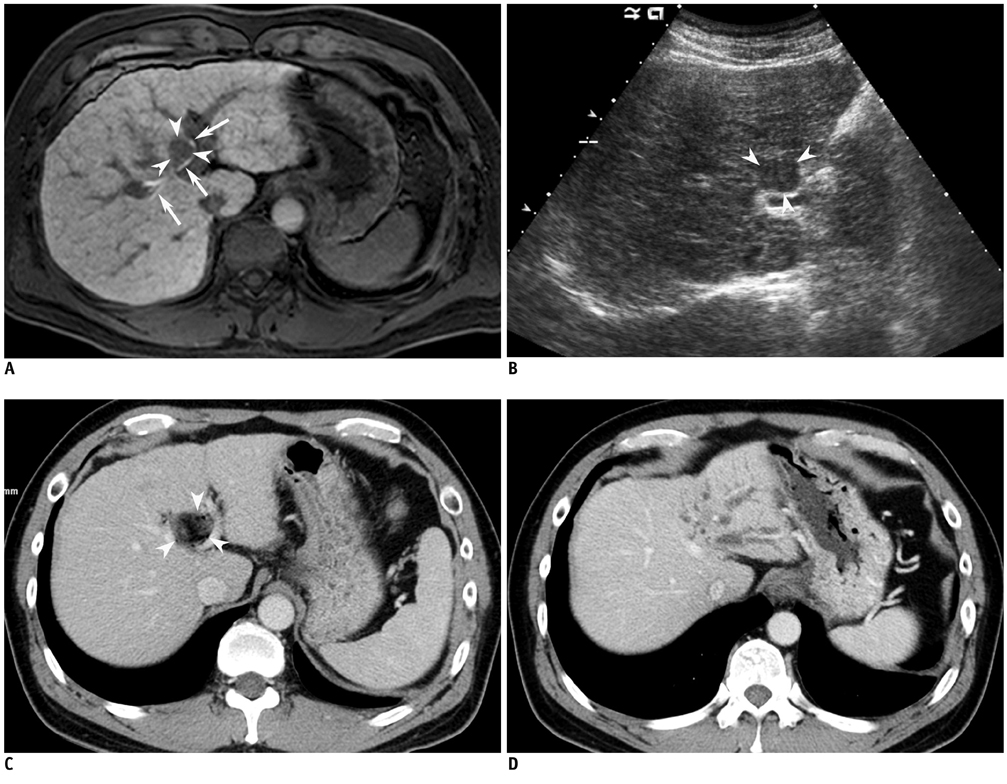
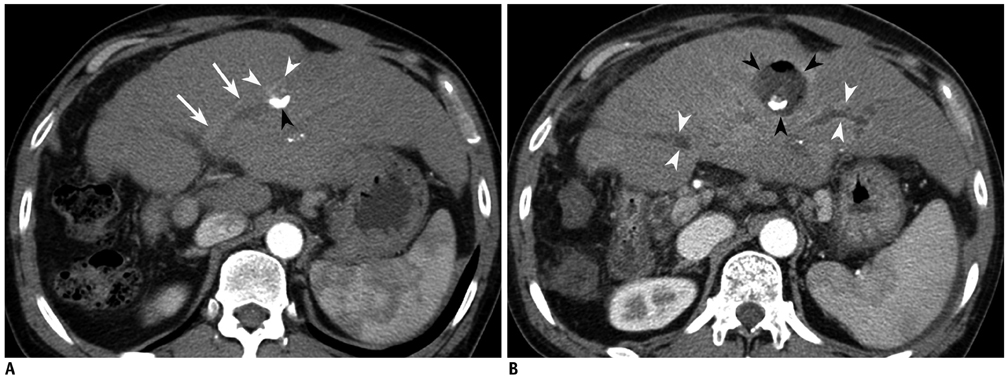
We performed PEI for HCCs in RFA-high risk locations, either alone or in combination with RFA. There were 20 HCCs (1.7 +/- 0.9 cm) in 20 patients (PEI group: n = 12; PEI + RFA group: n = 8). We evaluated technical success, local tumor progression and complications in both groups.
RESULTS
Technical success was achieved in all HCCs in both groups. During follow-up, local tumor progression was found in 41.7% (5/12) in the PEI group, whereas 12.5% (1/8) for the PEI + RFA group (p = 0.32). Bile duct dilatation was the most common complication, especially when the tumors were in periportal locations; 55% (5/9) in the PEI group and 50% (2/4) in the PEI + RFA group (p = 1.00). One patient in the PEI group developed severe biliary stricture and upstream dilatation that resulted in atrophy of the left hepatic lobe. One patient treated with PEI + RFA developed cholangitis and an abscess.
CONCLUSION
Combined PEI and RFA treatment has a tendency to be more effective than PEI alone for managing HCCs in high risk locations, although the difference is not statistically significant. Even though PEI is generally accepted as a safe procedure, it may cause major biliary complications for managing HCCs adjacent to the portal vein.
Keyword
MeSH Terms
-
Aged
Aged, 80 and over
Carcinoma, Hepatocellular/*drug therapy/*surgery
Catheter Ablation/*methods
Chemoembolization, Therapeutic/*methods
Disease Progression
Ethanol/administration & dosage
Female
Humans
Liver Neoplasms/*drug therapy/*surgery
Magnetic Resonance Imaging
Male
Middle Aged
Postoperative Complications
Retrospective Studies
Statistics, Nonparametric
Tomography, X-Ray Computed
Ethanol
Figure
Cited by 4 articles
-
Recent advance of local ablation for hepatocellular carcinoma
Hyunchul Rhim
J Korean Med Assoc. 2013;56(11):964-971. doi: 10.5124/jkma.2013.56.11.964.Innovative Techniques for Image-Guided Ablation of Benign Thyroid Nodules: Combined Ethanol and Radiofrequency Ablation
Hye Sun Park, Jung Hwan Baek, Young Jun Choi, Jeong Hyun Lee
Korean J Radiol. 2017;18(3):461-469. doi: 10.3348/kjr.2017.18.3.461.2018 Korean Liver Cancer Association–National Cancer Center Korea Practice Guidelines for the Management of Hepatocellular Carcinoma
,
Korean J Radiol. 2019;20(7):1042-1113. doi: 10.3348/kjr.2019.0140.2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma
J Liver Cancer. 2023;23(1):1-120. doi: 10.17998/jlc.2022.11.07.
Reference
-
1. Deuffic S, Poynard T, Buffat L, Valleron AJ. Trends in primary liver cancer. Lancet. 1998. 351:214–215.2. El-Serag HB, Mason AC. Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med. 1999. 340:745–750.3. Taylor-Robinson SD, Foster GR, Arora S, Hargreaves S, Thomas HC. Increase in primary liver cancer in the UK, 1979-94. Lancet. 1997. 350:1142–1143.4. Teratani T, Yoshida H, Shiina S, Obi S, Sato S, Tateishi R, et al. Radiofrequency ablation for hepatocellular carcinoma in so-called high-risk locations. Hepatology. 2006. 43:1101–1108.5. Shiina S, Teratani T, Obi S, Sato S, Tateishi R, Fujishima T, et al. A randomized controlled trial of radiofrequency ablation with ethanol injection for small hepatocellular carcinoma. Gastroenterology. 2005. 129:122–130.6. Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC. Radiofrequency ablation improves prognosis compared with ethanol injection for hepatocellular carcinoma < or =4 cm. Gastroenterology. 2004. 127:1714–1723.7. Shiina S, Tagawa K, Unuma T, Takanashi R, Yoshiura K, Komatsu Y, et al. Percutaneous ethanol injection therapy for hepatocellular carcinoma. A histopathologic study. Cancer. 1991. 68:1524–1530.8. Galandi D, Antes G. Radiofrequency thermal ablation versus other interventions for hepatocellular carcinoma. Cochrane Database Syst Rev. 2002. CD003046.9. Lu DS, Yu NC, Raman SS, Limanond P, Lassman C, Murray K, et al. Radiofrequency ablation of hepatocellular carcinoma: treatment success as defined by histologic examination of the explanted liver. Radiology. 2005. 234:954–960.10. Livraghi T. Radiofrequency ablation, PEIT, and TACE for hepatocellular carcinoma. J Hepatobiliary Pancreat Surg. 2003. 10:67–76.11. Wong SN, Lin CJ, Lin CC, Chen WT, Cua IH, Lin SM. Combined percutaneous radiofrequency ablation and ethanol injection for hepatocellular carcinoma in high-risk locations. AJR Am J Roentgenol. 2008. 190:W187–W195.12. Kurokohchi K, Watanabe S, Masaki T, Hosomi N, Funaki T, Arima K, et al. Combination therapy of percutaneous ethanol injection and radiofrequency ablation against hepatocellular carcinomas difficult to treat. Int J Oncol. 2002. 21:611–615.13. Bruix J, Sherman M. American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011. 53:1020–1022.14. Kuang M, Lu MD, Xie XY, Xu HX, Xu ZF, Liu GJ, et al. Ethanol ablation of hepatocellular carcinoma Up to 5.0 cm by using a multipronged injection needle with high-dose strategy. Radiology. 2009. 253:552–561.15. Rhim H, Lim HK. Radiofrequency ablation for hepatocellular carcinoma abutting the diaphragm: the value of artificial ascites. Abdom Imaging. 2009. 34:371–380.16. Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD 3rd, Dupuy DE, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol. 2009. 20:7 Suppl. S377–S390.17. Kondo Y, Shiina S, Tateishi R, Arano T, Uchino K, Enooku K, et al. Intrahepatic bile duct dilatation after percutaneous radiofrequency ablation for hepatocellular carcinoma: impact on patient's prognosis. Liver Int. 2011. 31:197–205.18. Orlando A, Leandro G, Olivo M, Andriulli A, Cottone M. Radiofrequency thermal ablation vs. percutaneous ethanol injection for small hepatocellular carcinoma in cirrhosis: meta-analysis of randomized controlled trials. Am J Gastroenterol. 2009. 104:514–524.19. Bouza C, López-Cuadrado T, Alcázar R, Saz-Parkinson Z, Amate JM. Meta-analysis of percutaneous radiofrequency ablation versus ethanol injection in hepatocellular carcinoma. BMC Gastroenterol. 2009. 9:31.20. Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC. Randomised controlled trial comparing percutaneous radiofrequency thermal ablation, percutaneous ethanol injection, and percutaneous acetic acid injection to treat hepatocellular carcinoma of 3 cm or less. Gut. 2005. 54:1151–1156.21. Livraghi T, Meloni F, Di Stasi M, Rolle E, Solbiati L, Tinelli C, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: Is resection still the treatment of choice? Hepatology. 2008. 47:82–89.22. Minami Y, Kudo M. Radiofrequency ablation of hepatocellular carcinoma: Current status. World J Radiol. 2010. 2:417–424.23. Livraghi T, Meloni F, Morabito A, Vettori C. Multimodal image-guided tailored therapy of early and intermediate hepatocellular carcinoma: long-term survival in the experience of a single radiologic referral center. Liver Transpl. 2004. 10:2 Suppl 1. S98–S106.24. Livraghi T, Solbiati L, Meloni MF, Gazelle GS, Halpern EF, Goldberg SN. Treatment of focal liver tumors with percutaneous radio-frequency ablation: complications encountered in a multicenter study. Radiology. 2003. 226:441–451.25. Kwon JH. Is percutaneous ethanol injection therapy still effective for hepatocellular carcinoma in the era of radiofrequency ablation? Gut Liver. 2010. 4:Suppl 1. S105–S112.26. Sung YM, Choi D, Lim HK, Lee WJ, Kim SH, Kim MJ, et al. Long-term results of percutaneous ethanol injection for the treatment of hepatocellular carcinoma in Korea. Korean J Radiol. 2006. 7:187–192.27. Kim SH, Lim HK, Choi D, Lee WJ, Kim SH, Kim MJ, et al. Changes in bile ducts after radiofrequency ablation of hepatocellular carcinoma: frequency and clinical significance. AJR Am J Roentgenol. 2004. 183:1611–1617.28. Koda M, Okamoto K, Miyoshi Y, Kawasaki H. Hepatic vascular and bile duct injury after ethanol injection therapy for hepatocellular carcinoma. Gastrointest Radiol. 1992. 17:167–169.29. Ogawa T, Kawamoto H, Kobayashi Y, Nakamura S, Miyatake H, Harada R, et al. Prevention of biliary complication in radiofrequency ablation for hepatocellular carcinoma-Cooling effect by endoscopic nasobiliary drainage tube. Eur J Radiol. 2010. 73:385–390.30. Lam VW, Ng KK, Chok KS, Cheung TT, Wat J, Fan ST, et al. Safety and efficacy of radiofrequency ablation for periductal hepatocellular carcinoma with intraductal cooling of the central bile duct. J Am Coll Surg. 2008. 207:e1–e5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is Percutaneous Ethanol Injection Therapy Still Effective for Hepatocellular Carcinoma in the Era of Radiofrequency Ablation?
- Needle Tract Implantation after Percutaneous Interventional Procedures in Hepatocellular Carcinomas: Lessons Learned from a 10-year Experience
- Non-surgical, Image-guided Management of Benign Thyroid Nodules
- Therapy of Pancreatic Neuroendocrine Tumors: Fine Needle Intervention including Ethanol and Radiofrequency Ablation
- Percutaneous cryoablation for hepatocellular carcinoma