J Korean Hip Soc.
2010 Dec;22(4):266-272. 10.5371/jkhs.2010.22.4.266.
The Efficacy of a Periarticular Soft Tissue Injection of Bupivacaine and Morphine in Total Hip Arthroplasty: a Prospective Study
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Hanyang University, Seoul, Korea. kimyh1@hanyang.ac.kr
- 2Department of Anesthesiology & Pain Medicine, Guri Hospital, College of Medicine, Hanyang University, Guri, Korea.
- KMID: 1461181
- DOI: http://doi.org/10.5371/jkhs.2010.22.4.266
Abstract
- PURPOSE
We wanted to assess the benefits and safety of periarticular soft tissue injection of bupivacaine and morphine in total hip arthroplasty by conducting a prospective randomized trial.
MATERIALS AND METHODS
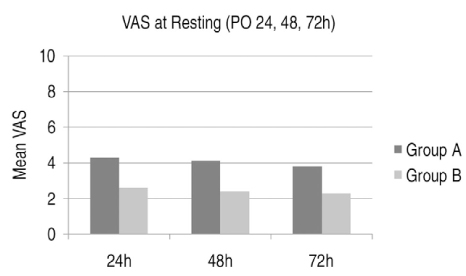
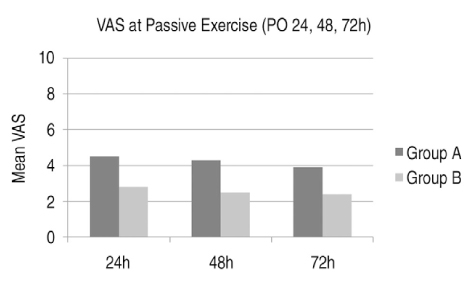
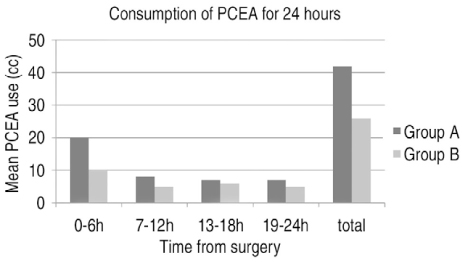
Between February 2008 and January 2010, a prospective, randomized study was performed on fifty patients with an American Society of Anesthesiology stage of I or II. All the patients were administered COX-2 inhibitor and we used PCEA (Patient Controlled Epidural Analgesia) for 24 hours postoperatively. All the patients underwent their operation under general anesthesia. Fifty randomly selected patients were divided into two groups. After reduction of the hip joint, 50 ml of normal saline was intraoperatively injected into 25 patients (Group A) and 50 ml of locally injected analgesia that included 0.5 ml 5 mg of morphine HCL, 40 ml of 0.5% 50 mg chirocaine (Levo-bupivacaine) and 9.5 ml of normal saline was injected into the capsule and the soft tissue and muscle around the hip joint in 25 patients (Group B). The analgesic efficacy was evaluated by the visual analogue scale (VAS) at 6 and 12 hours postoperatively with the patients in a resting state and at 24, 48 and 72 hours postoperatively with the patients in a resting state and during a passive exercise (30degrees) state. The consumption of PCEA and additional analgesic drugs was also evaluated postoperatively.
RESULTS
Significant differences were found between the 2 groups (P<0.05) with regard to the VAS at 6 and 12 hours postoperatively with the patients in a resting state and at 24, 48 and 72 hours postoperatively with the patients in a resting state and a passive exercise state. During 24 hours postoperatively, in the mixed analgesia injected group, the consumption of PCEA was significantly lower than that in the normal saline injected group (P<0.05). No significant differences were found for the consumption of additional analgesic drugs between the 2 groups (P>0.05).
CONCLUSION
Intraoperative periarticular soft tissue injection of bupivacaine and morphine can significantly reduce pain and it can reduce the requirement for patient-controlled analgesia, with no apparent risks, following total hip arthroplasty.
MeSH Terms
Figure
Reference
-
1. Söderman P, Malchau H, Herberts P. Outcome after total hip arthroplasty: Part I. General health evaluation in relation to definition of failure in the Swedish National Total Hip Arthoplasty register. Acta Orthop Scand. 2000. 71:354–359.
Article2. Söderman P, Malchau H, Herberts P, Zügner R, Regnér H, Garellick G. Outcome after total hip arthroplasty: Part II. Disease-specific follow-up and the Swedish National Total Hip Arthroplasty Register. Acta Orthop Scand. 2001. 72:113–119.
Article3. Filos KS, Lehmann KA. Current concepts and practice in postoperative pain management: need for a change? Eur Surg Res. 1999. 31:97–107.
Article4. Lee KJ, Min BW, Bae KC, Cho CH, Kwon DH. Efficacy of multimodal pain control protocol in the setting of total hip arthroplasty. Clin Orthop Surg. 2009. 1:155–160.
Article5. Singelyn FJ, Deyaert M, Joris D, Pendeville E, Gouverneur JM. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg. 1998. 87:88–92.
Article6. Horlocker TT, Hebl JR, Kinney MA, Cabanela ME. Opioid-free analgesia following total knee arthroplasty--a multimodal approach using continuous lumbar plexus (psoas compartment) block, acetaminophen, and ketorolac. Reg Anesth Pain Med. 2002. 27:105–108.
Article7. Pettine KA, Wedel DJ, Cabanela ME, Weeks JL. The use of epidural bupivacaine following total knee arthroplasty. Orthop Rev. 1989. 18:894–901.8. Mahoney OM, Noble PC, Davidson J, Tullos HS. The effect of continuous epidural analgesia on postoperative pain, rehabilitation, and duration of hospitalization in total knee arthroplasty. Clin Orthop Relat Res. 1990. 260:30–37.
Article9. Kalso E, Tramér MR, Carroll D, McQuay HJ, Moore RA. Pain relief from intra-articular morphine after knee surgery: a qualitative systematic review. Pain. 1997. 71:127–134.
Article10. DeWeese FT, Akbari Z, Carline E. Pain control after knee arthroplasty: intraarticular versus epidural anesthesia. Clin Orthop Relat Res. 2001. 392:226–231.11. Mauerhan DR, Campbell M, Miller JS, Mokris JG, Gregory A, Kiebzak GM. Intra-articular morphine and/or bupivacaine in the management of pain after total knee arthroplasty. J arthroplasty. 1997. 12:546–552.
Article12. Vendittoli PA, Makinen P, Drolet P, et al. A multimodal analgesia protocol for total knee arthroplasty. A randomized, controlled study. J Bone Joint Surg Am. 2006. 88:282–289.13. Busch CA, Shore BJ, Bhandari R, et al. Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am. 2006. 88:959–963.
Article14. Follin SL, Charland SL. Acute pain management: operative or medical procedures and trauma. Ann Pharmacother. 1997. 31:1068–1076.
Article15. Kroll MA, Otis JC, Sculco TP, et al. The relationship of stride characteristics to pain before and after total knee arthroplasty. Clin Orthop Relat Res. 1989. 239:191–195.
Article16. Strassels SA, Chen C, Carr DB. Postoperative analgesia: economics, resource use, and patient satisfaction in an urban teaching hospital. Anesth Analg. 2002. 94:130–137.
Article17. Bianconi M, Ferraro L, Traina GC, et al. Pharmacokinetics and efficacy of ropivacaine continuous wound instillation after joint replacement surgery. Br J Anaesth. 2003. 91:830–835.
Article18. Forst J, Wolff S, Thamm P, Forst R. Pain therapy following joint replacement.A randomized study of patient-controlled analgesia versus conventional pain therapy. Arch Orthop Trauma Surg. 1999. 119:267–270.19. Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA Jr, Wu CL. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA. 2003. 290:2455–2463.20. Perl ER. Cutaneous polymodal receptors: characteristics and plasticity. Prog Brain Res. 1996. 113:21–37.21. Woolf CJ. Evidence for a central component of post-injury pain hypersensitivity. Nature. 1983. 306:686–688.
Article22. Stein C. The control of pain in peripheral tissue by opioids. N Engl J Med. 1995. 332:1685–1690.
Article23. Parvataneni HK, Shah VP, Howard H, Cole N, Ranawat AS, Ranawat CS. Controlling pain after total hip and knee arthroplasty using a multimodal protocol with local periarticular injections: a prospective randomized study. J Arthroplasty. 2007. 22:6 Suppl 2. 33–38.
Article24. Badner NH, Bourne RB, Rorabeck CH, MacDonald SJ, Doyle JA. Intra-articular injection of bupivacaine in knee-replacement operations. Results of use for analgesia and for preemptive blockade. J Bone Joint Surg Am. 1996. 78:734–738.25. Dalsgaard J, Felsby S, Juelsgaard P, Froekjaer J. Low-dose intra-articular morphine analgesia in day case knee arthroscopy: a randomized double-blinded prospective study. Pain. 1994. 56:151–154.
Article26. Martinsson T, Haegerstrand A, Dalsgaard CJ. Effects of ropivacaine on eicosanoid release from human granulocytes and endothelial cells in vitro. Inflamm Res. 1997. 46:398–403.
Article27. Lombardi AV Jr, Berend KR, Mallory TH, Dodds KL, Adams JB. Soft tissue and intra-articular injection of bupivacaine, epinephrine, and morphine has a beneficial effect after total knee arthroplasty. Clin Orthop Relat Res. 2004. 428:125–130.
Article28. Ritter MA, Koehler M, Keating EM, Faris PM, Meding JB. Intra-articular morphine and/or bupivacaine after total knee replacement. J Bone Joint Surg Br. 1999. 81:301–303.
Article29. Andersen LJ, Poulsen T, Krogh B, Nielsen T. Postoperative analgesia in total hip arthroplasty: a randomized double-blinded, placebo-controlled study on peroperative and postoperative ropivacaine, ketorolac, and adrenaline wound infiltration. Acta Orthop. 2007. 78:187–192.
Article30. Andersen KV, Pfeiffer-Jensen M, Haraldsted V, Søballe K. Reduced hospital stay and narcotic consumption, and improved mobilization with local and intraarticular infiltration after hip arthroplasty: a randomized clinical trial of an intraarticular technique versus epidural infusion in 80 patients. Acta Orthop. 2007. 78:180–186.
Article31. Heard SO, Edwards WT, Ferrari D, et al. Analgesic effect of intraarticular bupivacaine or morphine after arthroscopic knee surgery: a randomized, prospective, double-blind study. Anesth Analg. 1992. 74:822–826.32. Woolf CJ, Chong MS. Preemptive analgesia--treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg. 1993. 77:362–379.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Intraoperative Periarticular Local Injection in Total Knee Arthroplasty
- The Analgesic Effect of Postoperative Combined Epidural, Soft Tissue, and Intra-articular Injection of Morphine and Bupivacaine in Patients undergoing Total Knee Arthroplasty
- Pain Control after Total Hip Replacement Arthroplasty Using Periarticular Multimodal Drug Injection
- Minimally Invasive Total Hip Arthroplasty
- The Analgesic Effect of Intraarticular Bupivacaine and Morphine after Arthroscopic Knee Surgery