J Korean Hip Soc.
2010 Dec;22(4):273-282. 10.5371/jkhs.2010.22.4.273.
Pain Control after Total Hip Replacement Arthroplasty Using Periarticular Multimodal Drug Injection
- Affiliations
-
- 1Department of Orthopedic Surgery, Busan Paik Hospital, College of Medicine, Inje University, Busan, Korea. kimjh8142@hanmail.net
- 2Department of Orthopedic Surgery, Busan Seail Hospital, Busan, Korea.
- KMID: 1461182
- DOI: http://doi.org/10.5371/jkhs.2010.22.4.273
Abstract
- PURPOSE
This study attempted to evaluate the pattern of change of the pain after total hip arthroplasty (THA) and to confirm the effect of periarticular multimodal drug injection (PMDI) on controlling the early postoperative pain.
MATERIALS AND METHODS
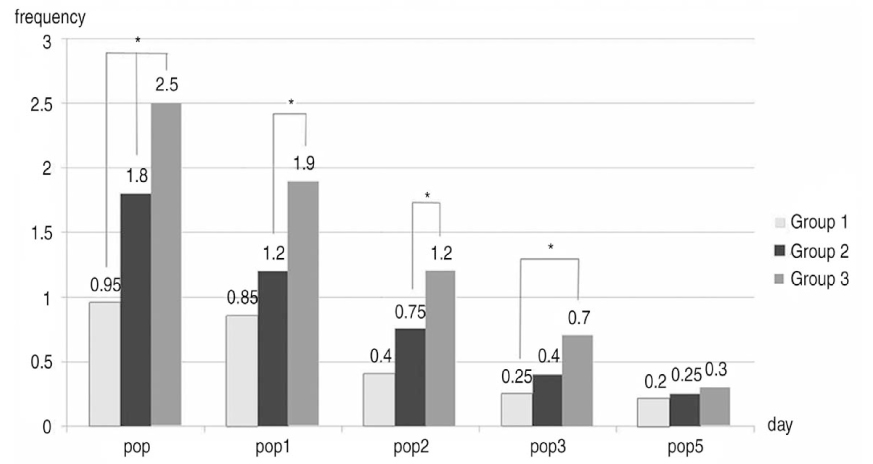
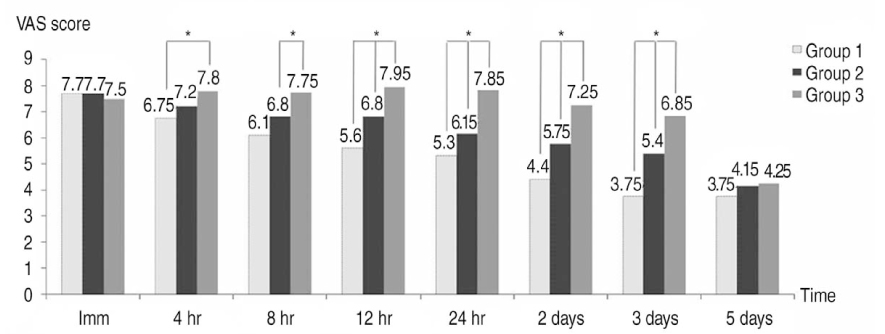
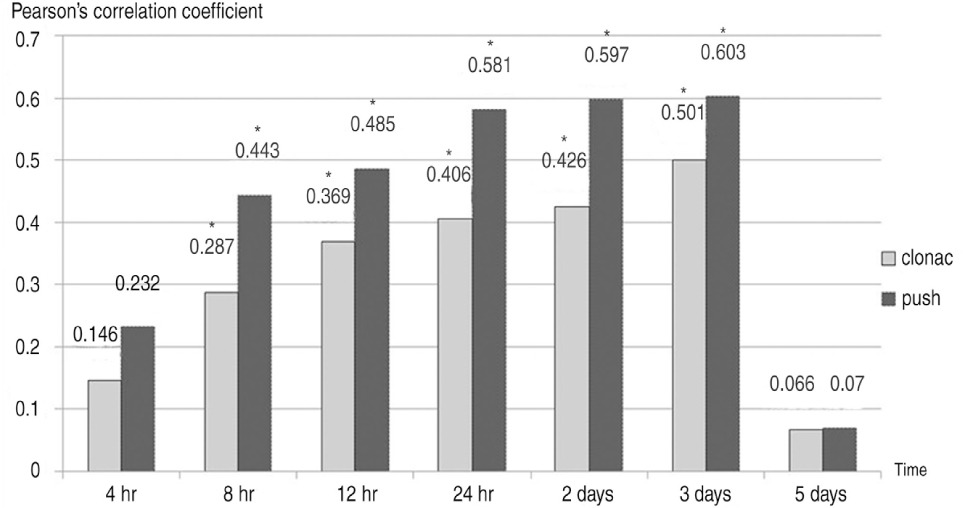
Of the total patients who underwent primary THA at our hospital because of osteonecrosis of the femoral head from March to October 2008, 60 patients were enrolled in this study. The subjects were divided into three groups. Groups 1 & 2 received periarticular injection. Group 1 included the patients who were injected with a combination of opioid, long-acting local anesthetics, a non-steroidal anti-inflammatory drug and epinephrine. Group 2 received a combination of morphine and ropivacaine and group 3 was not injected with any analgesics. The visual analogue scale (VAS) at 4 hours, 8 hours, 12 hours, 24 hours, 2 days, 3 days, 5 days, 14 days and 1 month after surgery, the frequency that patients pushed the self-controlled pain medication machine for 2 days after surgery and the amount of clonac that was injected according to the needs of the patients were used as objective measures.
RESULTS
The VAS score at postoperative 4 hours to 3 days among the groups showed a significant difference (P<0.05), but the VAS scores at postoperative 5 days to 1 month among the groups showed no significant difference (P>0.05). The frequency of pushing the self-controlled pain medication machine among the groups and the amount of clonac according to the needs of the patients among the groups showed that there were significant decreases at the operation day, the postoperative 1, 2 day and the 3 days (P<0.05).
CONCLUSION
PMDI has a significant effect on controlling the early postoperative pain after THA.
MeSH Terms
Figure
Reference
-
1. Donald SM. Sir John Charnley (1911-1982): inspiration to future generations of orthopaedic surgeons. Scott Med J. 2007. 52:43–46.
Article2. Berry DJ. Long-term follow-up studies of total hip arthroplasty. Orthopedics. 2005. 28:8 Suppl. s879–s880.
Article3. Eswaramoorthy V, Moonot P, Kalairajah Y, Biant LC, Field RE. The Metasul metal-on-metal articulation in primary total hip replacement: clinical and radiological results at ten years. J Bone Joint Surg Br. 2008. 90:1278–1283.4. Mullins MM, Norbury W, Dowell JK, Heywood-Waddington M. Thirty-year results of a prospective study of Charnley total hip arthroplasty by the posterior approach. J Arthroplasty. 2007. 22:833–839.
Article5. Yoon TR, Rowe SM, Kim MS, Cho SG, Seon JK. Fifteen- to 20-year results of uncemented tapered fully porous-coated cobalt-chrome stems. Int Orthop. 2008. 32:317–323.
Article6. Illgen RL, Pellino TA, Gordon DB, Butts S, Heiner JP. Prospective analysis of a novel long-acting oral opioid analgesic regimen for pain control after total hip and knee arthroplasty. J Arthroplasty. 2006. 21:814–820.
Article7. Maheshwari AV, Blum YC, Shekhar L, Ranawat AS, Ranawat CS. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res. 2009. 467:1418–1423.
Article8. Ranawat AS, Ranawat CS. Pain management and accelerated rehabilitation for total hip and total knee arthroplasty. J Arthroplasty. 2007. 22:7 Suppl 3. 12–15.
Article9. Parvataneni HK, Ranawat AS, Ranawat CS. The use of local periarticular injections in the management of postoperative pain after total hip and knee replacement: a multimodal approach. Instr Course Lect. 2007. 56:125–131.10. Parvataneni HK, Shah VP, Howard H, Cole N, Ranawat AS, Ranawat CS. Controlling pain after total hip and knee arthroplasty using a multimodal protocol with local periarticular injections: a prospective randomized study. J Arthroplasty. 2007. 22:6 Suppl 2. 33–38.
Article11. Andersen LJ, Poulsen T, Krogh B, Nielsen T. Postoperative analgesia in total hip arthroplasty: a randomized double-blinded, placebo-controlled study on peroperative and postoperative ropivacaine, ketorolac, and adrenaline wound infiltration. Acta Orthop. 2007. 78:187–192.
Article12. Ritter MA, Koehler M, Keating EM, Faris PM, Meding JB. Intra-articular morphine and/or bupivacaine after total knee replacement. J Bone Joint Surg Br. 1999. 81:301–303.
Article13. Ha YC, Jung WH, Kim JR, Seong NH, Kim SY, Koo KH. Prediction of collapse in femoral head osteonecrosis: a modified Kerboul method with use of magnetic resonance images. J Bone Joint Surg Am. 2006. 88:Suppl 3. 35–40.
Article14. Ybinger T, Kumpan W. Enhanced acetabular component positioning through computer-assisted navigation. Int Orthop. 2007. 31:Suppl 1. S35–S38.
Article15. Sculco TP, Jordan LC, Walter WL. Minimally invasive total hip arthroplasty: the Hospital for Special Surgery experience. Orthop Clin North Am. 2004. 35:137–142.
Article16. Willems MM, Kooloos J, Gibbons P, Minderhoud N, Weernink T, Verdonschot N. The stability of the femoral component of a minimal invasive total hip replacement system. Proc Inst Mech Eng H. 2006. 220:465–472.
Article17. Mont MA, Seyler TM. Advanced techniques for rehabilitation after total hip and knee arthroplasty. Clin Orthop Relat Res. 2009. 467:1395.
Article18. Rawal N, Hylander J, Nydahl PA, Olofsson I, Gupta A. Survey of postoperative analgesia following ambulatory surgery. Acta Anaesthesiol Scand. 1997. 41:1017–1022.
Article19. Filos KS, Lehmann KA. Current concepts and practice in postoperative pain management: need for a change? Eur Surg Res. 1999. 31:97–107.
Article20. Ryu J, Saito S, Yamamoto K, Sano S. Factors influencing the postoperative range of motion in total knee arthroplasty. Bull Hosp Jt Dis. 1993. 53:35–40.21. Mahoney OM, Noble PC, Davidson J, Tullos HS. The effect of continuous epidural analgesia on postoperative pain, rehabilitation, and duration of hospitalization in total knee arthroplasty. Clin Orthop Relat Res. 1990. 260:30–37.
Article22. DeWeese FT, Akbari Z, Carline E. Pain control after knee arthroplasty: intraarticular versus epidural anesthesia. Clin Orthop Relat Res. 2001. 392:226–231.23. Stein C. The control of pain in peripheral tissue by opioids. N Engl J Med. 1995. 332:1685–1690.
Article24. Allen HW, Liu SS, Ware PD, Nairn CS, Owens BD. Peripheral nerve blocks improve analgesia after total knee replacement surgery. Anesth Analg. 1998. 87:93–97.
Article25. Kligman M, Bruskin A, Sckliamser J, Vered R, Roffman M. Intra-synovial, compared to intra-articular morphine provides better pain relief following knee arthroscopy menisectomy. Can J Anaesth. 2002. 49:380–383.
Article26. Rasmussen ML, Mathiesen O, Dierking G, et al. Multimodal analgesia with gabapentin, ketamine and dexamethasone in combination with paracetamol and ketorolac after hip arthroplasty: a preliminary study. Eur J Anaesthesiol. 2010. 27:324–330.
Article27. Weng WJ, Wang F, Chen DY, Yuan T, Xu ZH, Jiang Q. Observation of the efficacy of local multimodal analgesic drugs injection in total hip arthroplasty. Zhongguo Gu Shang. 2008. 21:834–836.28. Karmakar MK, Ho AM, Law BK, Wong AS, Shafer SL, Gin T. Arterial and venous pharmacokinetics of ropivacaine with and without epinephrine after thoracic paravertebral block. Anesthesiology. 2005. 103:704–711.
Article29. McCormack K, Brune K. Dissociation between the antinociceptive and anti-inflammatory effects of the nonsteroidal anti-inflammatory drugs. A survey of their analgesic efficacy. Drugs. 1991. 41:533–547.
Article30. Lee KJ, Min BW, Bae KC, Cho CH, Kwon DH. Efficacy of multimodal pain control protocol in the setting of total hip arthroplasty. Clin Orthop Surg. 2009. 1:155–160.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Multimodal Pain Control Protocol in the Setting of Total Hip Arthroplasty
- Perioperative Pain Management in Total Hip Arthroplasty: Korean Hip Society Guidelines
- Usefulness of Morphine in the Periarticular Multimodal Drug Local Injection after Surgery for Hallux Valgus
- The Effect of Intraoperative Periarticular Local Injection in Total Knee Arthroplasty
- Posterior Approach to Total Hip Joint Replacement Arthroplasty