J Korean Assoc Oral Maxillofac Surg.
2010 Aug;36(4):291-302. 10.5125/jkaoms.2010.36.4.291.
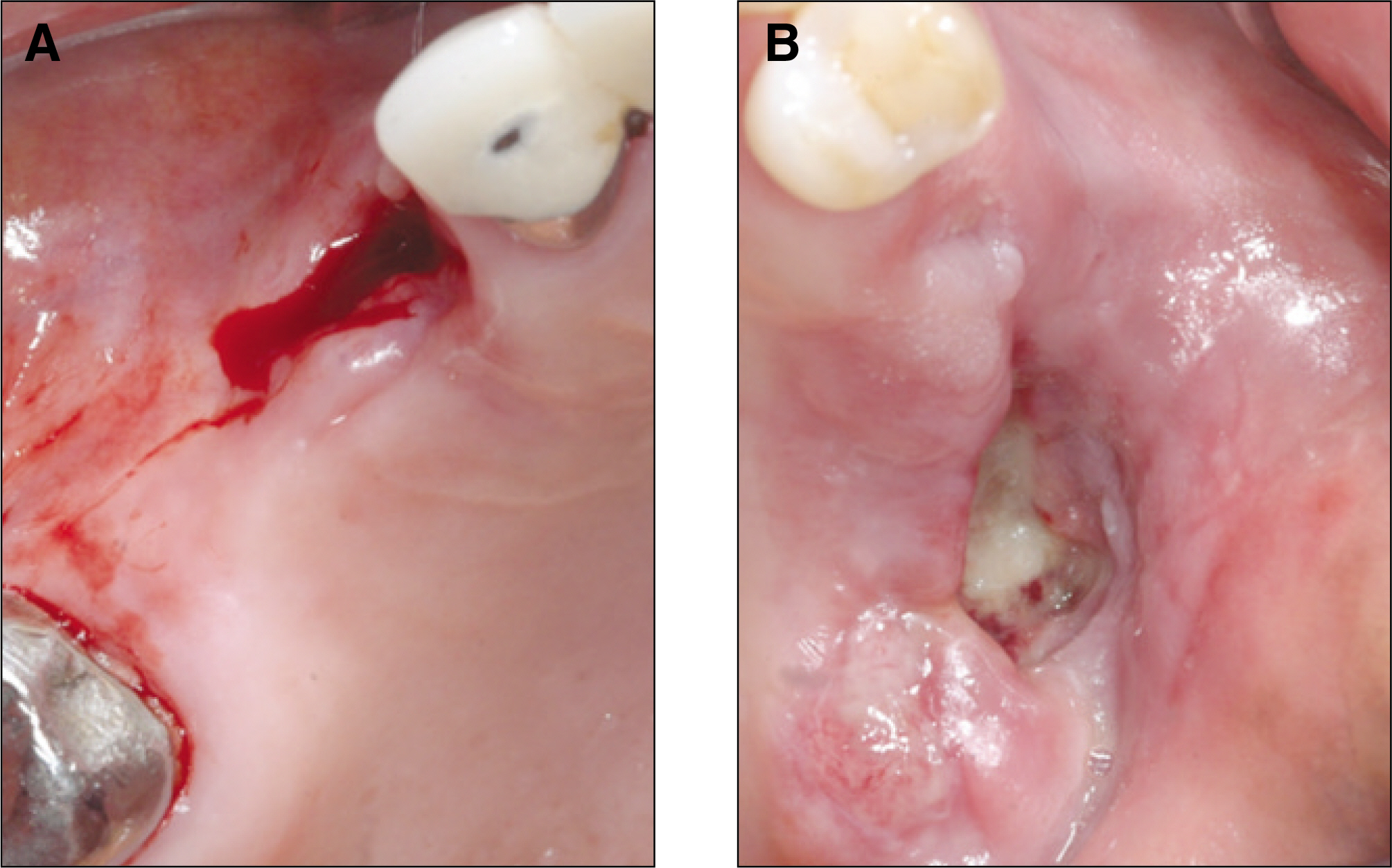
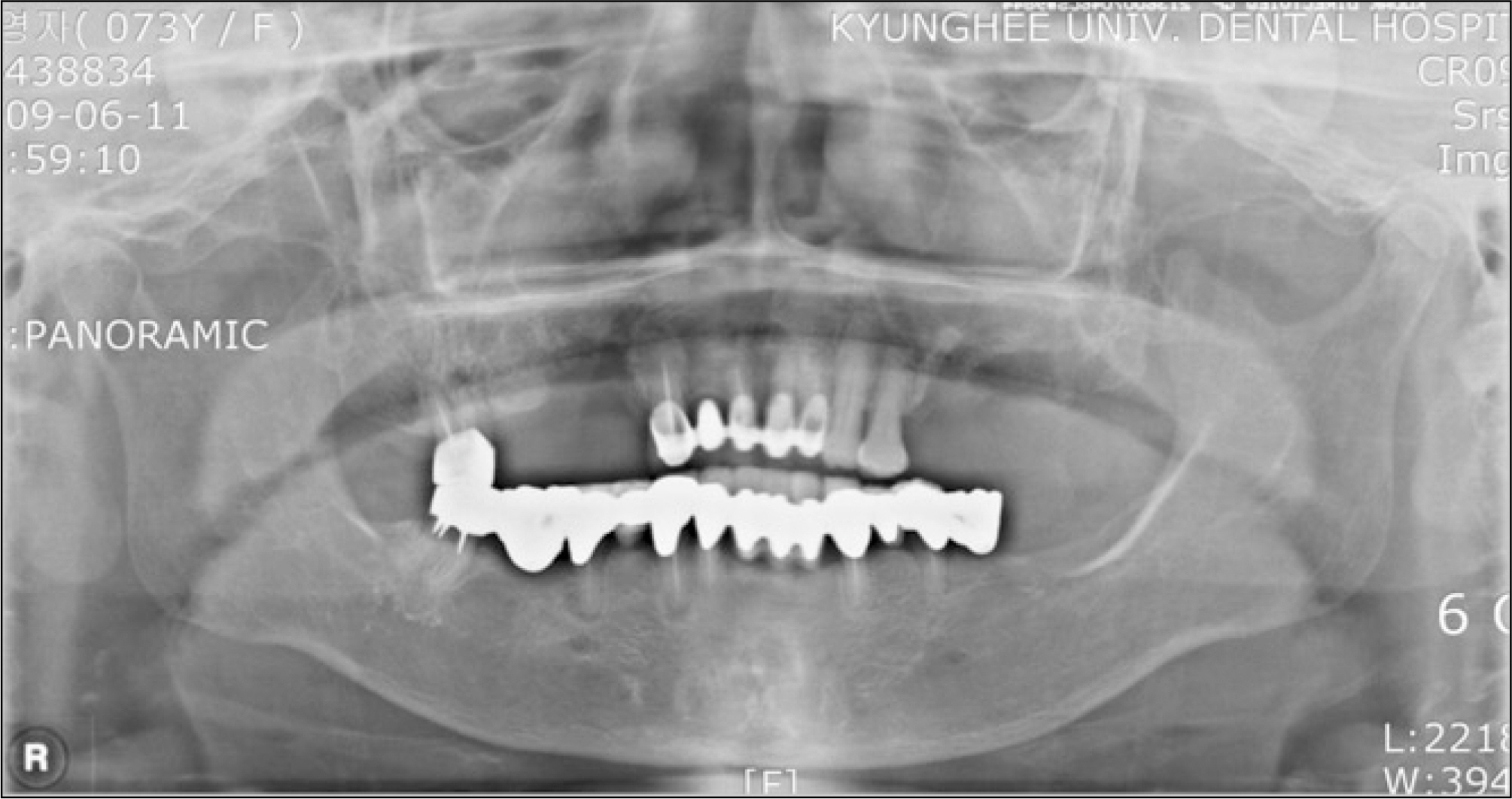
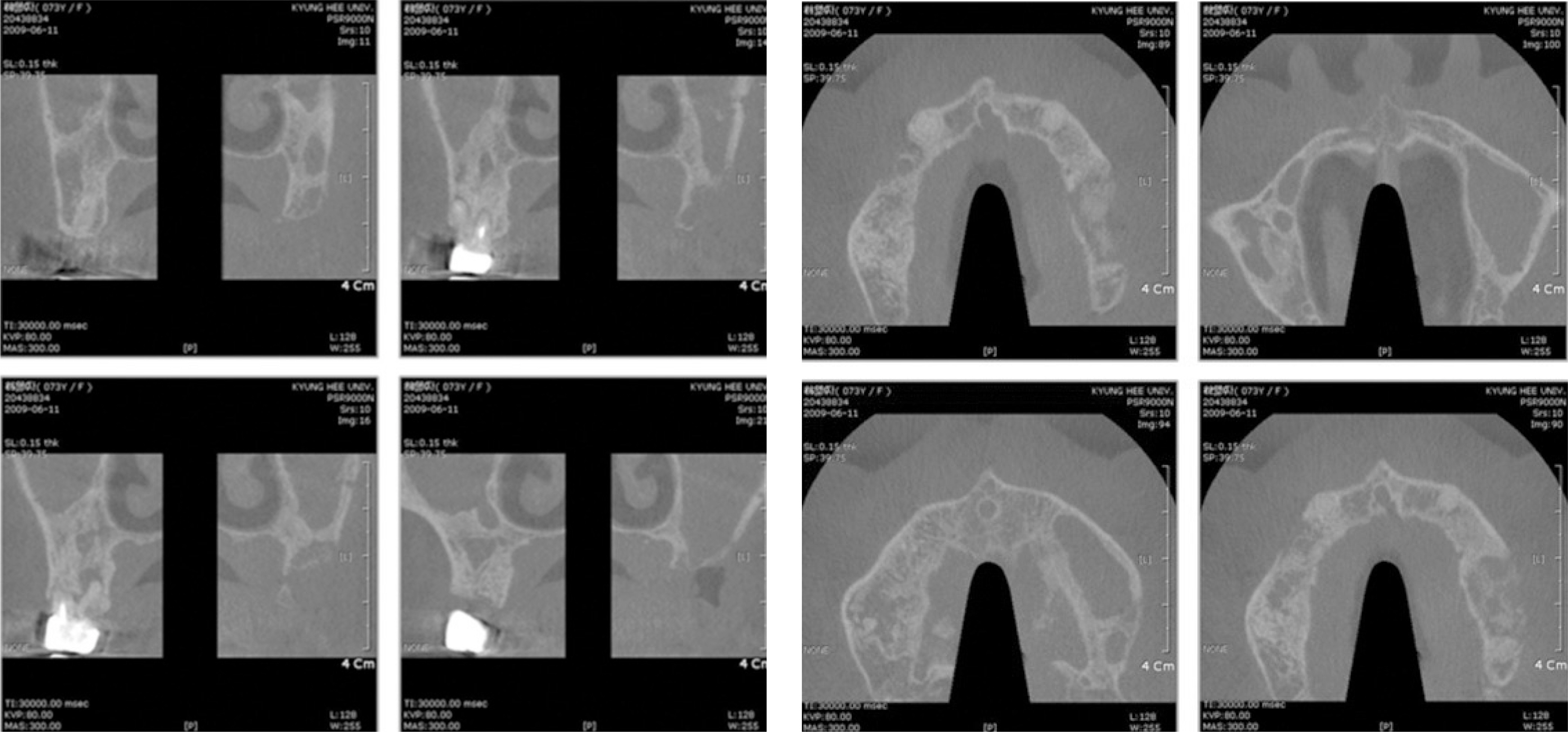
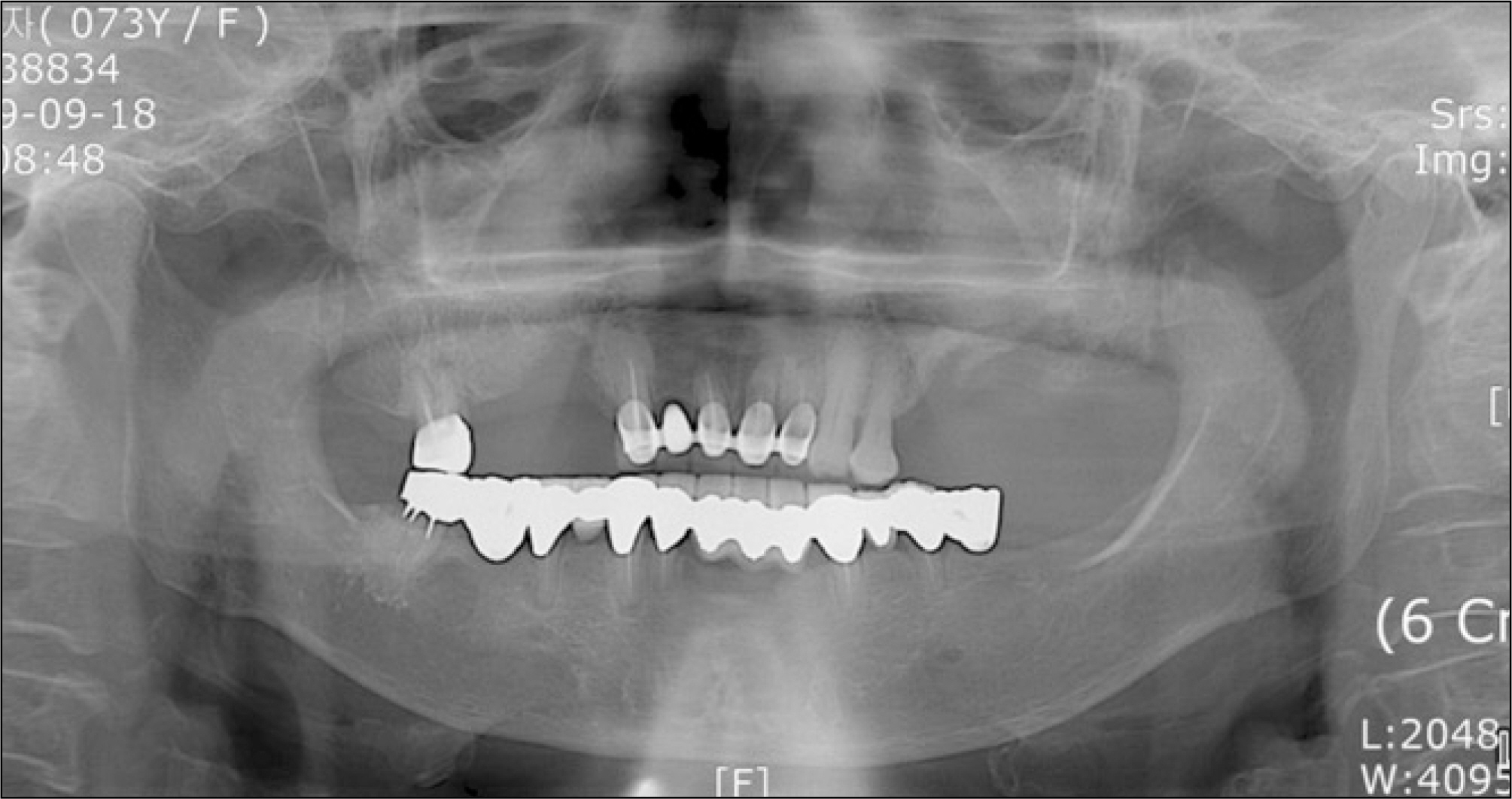
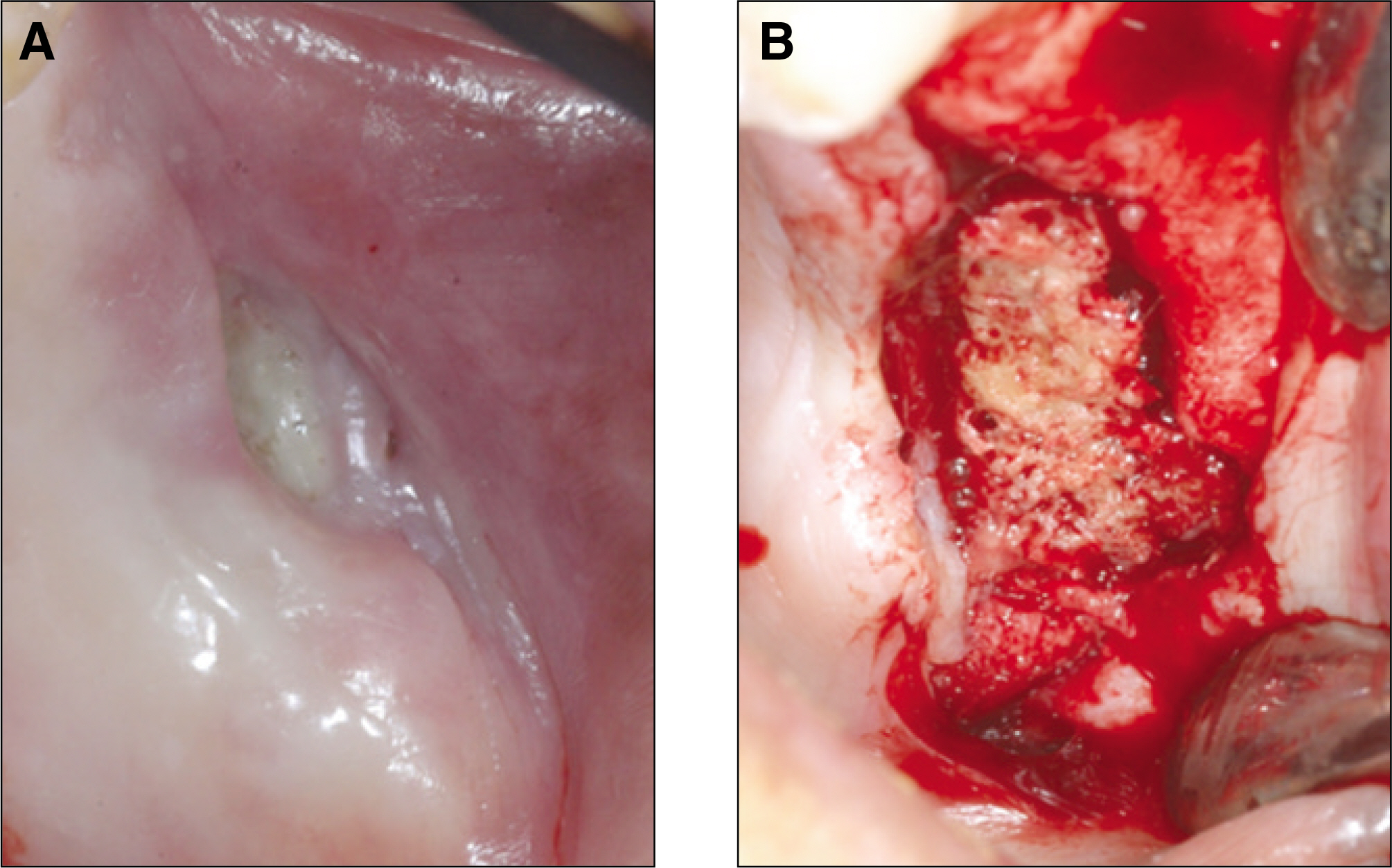
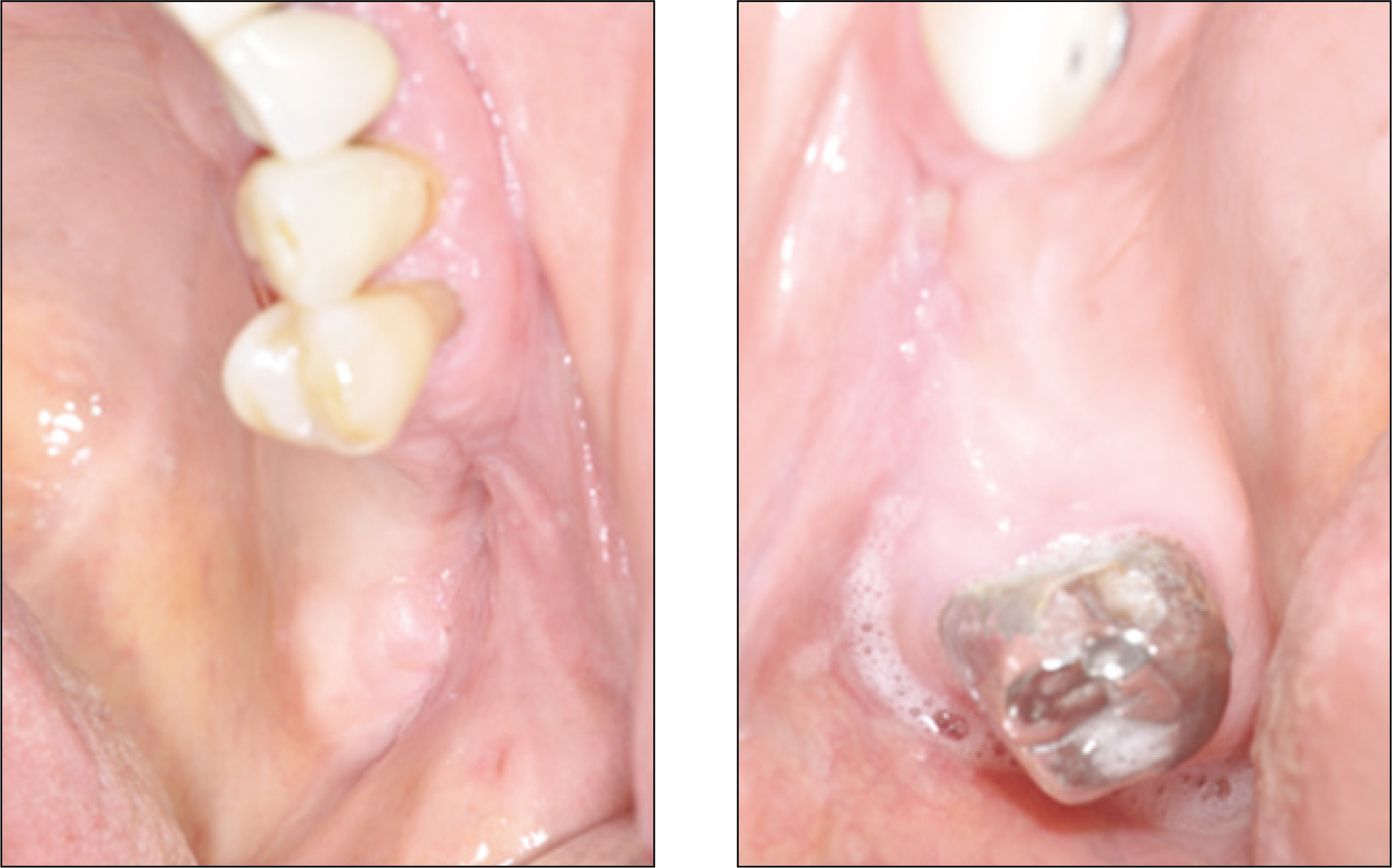
Study on bisphosphonate-related osteonecrosis of the jaw (BRONJ): case report and literature review
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Dentistry, Kyung Hee University, Seoul, Korea. kyukab@khu.ac.kr
- 2School of Dentistry, Kyung Hee University, Seoul, Korea.
- KMID: 1457782
- DOI: http://doi.org/10.5125/jkaoms.2010.36.4.291
Abstract
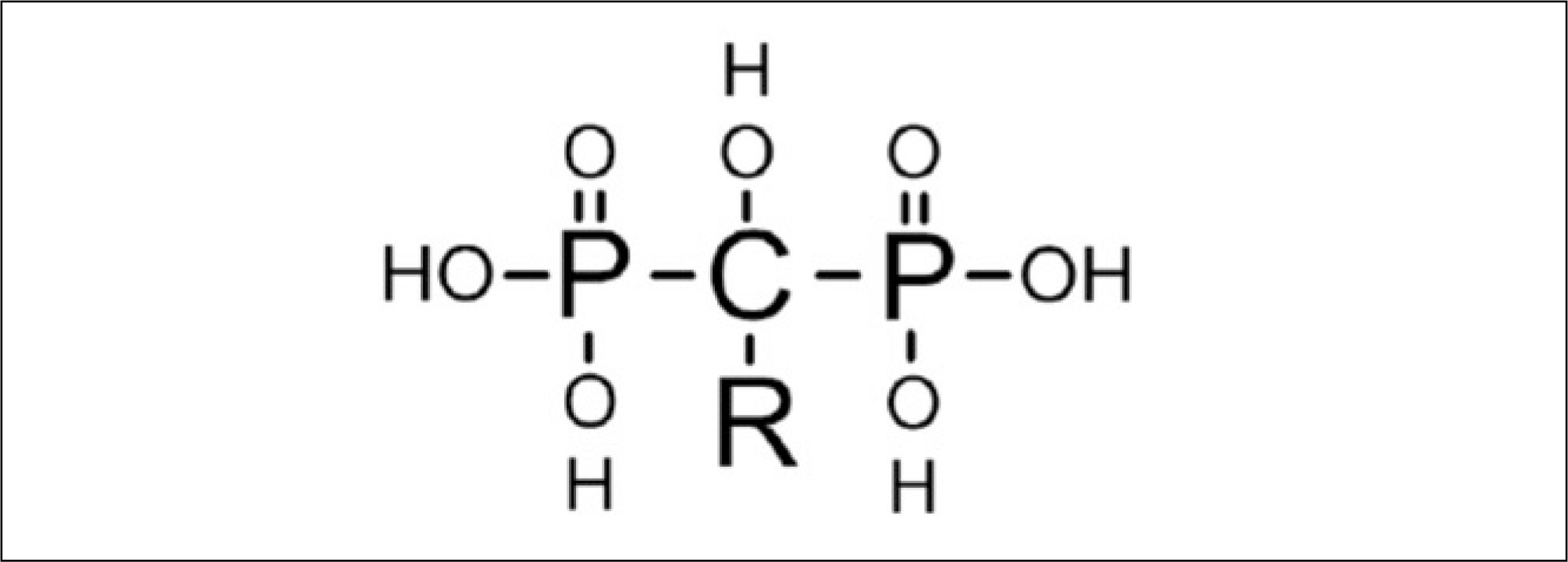
- Bisphosphonate-related osteonecrosis of the jaw (BRONJ) is a side effect of Bisphosphonates (BPs) use. These days, oral bisphosphonates are normally prescribed to treat osteoporosis. Intravenous BPs are used extensively to treat osteolytic bone lesions related to multiplemyeloma and bone metastasis of solid cancers, breast cancer or prostate cancer. As the prescription of BPs is universalized and the number of people treated with BPs is increasing, an accurate understanding and proper management of BRONJ are required. The aim of this study was to improve the clinicians'understanding of BRONJ by reviewing the literature. To achieve this, this paper introduces case reports as well as the current concept of BRONJ based on the 2009 updates by American Association of Oral and Maxillofacial (AAOMS) including the definition, epidemiology, etiology, diagnosis, treatment and prevention of BRONJ.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003; 61:1115–7.
Article2. Marx RE, Sawatari Y, Fortin M, Broumand V. Biphosphonate-induced exposed bone (osteonecrosis/ostoepetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005; 63:1567–75.3. Advisory Task Force on Bisphosphonate-Related Ostenonecrosis of the Jaws, American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg. 2007; 65:369–76.4. Kwon YD, Yoon BW, Walter C. Bisphosphonate, is it an emerging risk factor in oral surgery? J Korean Assoc Maxillofac Plast Reconstr Surg. 2007; 29:456–62.5. Park YD, Kim YR, Kim DY, Chung YS, Lee JK, Kim YG, et al. Awareness of Korean dentists on bisphosphonate related osteonecrosis of the jaws: preliminary report. J Korean Assoc Oral Maxillofac Surg. 2009; 35:153–7.6. Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B. American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws-2009 update. J Oral Maxillofac Surg. 2009; 67(5 Suppl):2–12.
Article7. The Korean Endocrine Society, the Korean Society of Bone Metabolism, the Korean Society of Osteoporosis, the Korean Association of Oral and Maxillofacial Surgeons. Bisphosphonate related osteonecrosis of the jaw (BRONJ): position statement of Korea. J Korean Endocr Soc. 2009; 24:227–30.8. Francis MD, Russell RG, Fleisch H. Diphosphonate inhibit formation of calcium phosphate crystals in vitro and pathological calcifications in vivo. Science. 1969; 165:1264–6.9. van Beek E, Pieterman E, Cohen L, Lo ¨wik C, Papapoulos S. Farnesyl pyrophosphate synthase is the molecular target of nitrogen containing bisphosphonates. Biochem Biophys Res Commun. 1999; 264:108–11.10. Kimmel DB. Mechanism of action, pharmacokinetic and pharmacodynamic profile, and clinical applications of nitrogen-containing bisphosphonates. J Dent Res. 2007; 86:1022–33.
Article11. Va ¨a ¨na ¨nen HK, Zhao H, Mulari M, Halleen JM. The cell biology of osteoclast function. J Cell Sci. 2000; 113:377–81.12. Fantasia JE. Bisphosphonates-what the dentist needs to know: practical consideration. J Oral Maxillofac Surg. 2009; 67(5 Suppl):53–60.13. Hillner BE, Ingle JN, Berenson JR, Janjan NA, Albain KS, Lipton A, et al. American Society of Clinical Oncology guideline on the role of bisphosphonates in breast cancer. American Society of Clinical Oncology Bisphosphonates Expert Panel. J Clin Oncol. 2000; 18:1378–91.14. Mehrotra B. Bisphosphonates-role in cancer therapies. J Oral Maxillofac Surg. 2009; 67(5 Suppl):19–26.
Article15. Landesberg R, Eisig S, Fennoy I, Siris E. alternative indications for bisphosphonate therapy. J Oral Maxillofac Surg. 2009; 67(5 Suppl):27–34.
Article16. Allen MR, Burr DB. The pathogenesis of bisphosphonate-related osteonecrosis of the jaw: so many hypotheses, so few data. J Oral Maxillofac Surg. 2009; 67(5 Suppl):61–70.
Article17. Russell RG, Xia Z, Dunford JE, Oppermann U, Kwaasi A, Hulley PA, et al. Bisphosphonates: an update on mechanisms of action and how these relate to clinical efficacy. Ann N Y Acad Sci. 2007; 1117:209–57.
Article18. Garetto LP, Chen J, Parr JA, Roberts WE. Remodeling dynamics of bone supporting rigidly fixed titanium implants: a histomorphometric comparison in four species including humans. Implant Dent. 1995; 4:235–43.
Article19. Han ZH, Palnitkar S, Rao DS, Nelson D, Parfitt AM. Effects of ethnicity and age or menopause on the remodeling and turnover of iliac bone: implications for mechanism of bone loss. J Bone Miner Res. 1997; 12:498–508.20. Allen MR, Burr DB. Mandible matrix necrosis in beagle dogs after 3 years of daily oral bisphosphonate treatment. J Oral Maxillofac Surg. 2008; 66:987–94.
Article21. Lewiecki EM, Miller PD, McClung MR, Cohen SB, Bolognese MA, Liu Y, et al. Two-year treatment with denosumab (AMG 162) in a randomized phase 2 study of postmenopausal women with low BMD. J Bone Miner Res. 2007; 22:1832–41.
Article22. Harper RP, Fung E. Resolution of bisphosphonateassociated osteonecosis of the mandible: possible application for intermittent low-dose parathyroid hormone [rhPTH(1–34)]. J Oral Maxillofac Surg. 2007; 65:573–80.23. Lau AN, Ali SH, Adachi JD. Resolution of osteonecosis of the jaw after teriparatide [recombinant human PTH (1–34)] therapy. Osteoporos Int. 2008; 19(Suppl 1):S80.24. Wang HL, Weber D, McCauley LK. Effect of longterm oral bisphosphonates on implant wound healing: literature review and a case report. J Periodontol. 2007; 78:584–94.
Article25. Li C, Mori S, Li J, Kaji Y, Akiyama T, Kawanishi J, et al. Longterm effect of incadronate disodium (YM-175) on fracture healing of femoral shaft in growing rats. J Bone Miner Res. 2001; 16:429–36.
Article26. Peter CP, Cook WO, Nunamaker DM, Provost MT, Seedor JG, Rodan GA. Effect of alendronate on fracture healing and bone remodeling in dogs. J Orthop Res. 1996; 14:74–9.
Article27. Frost HM. In vivo osteocyte death. J Bone Joint Surg Am. 1960; 42A:138–43.
Article28. Roelofs AJ, Coxon FP, Ebetino FH, Bala JF, Kashemirov BA, McKenna CE, et al. Use of a fluorescent analogue of risedronate to study localisation and cellular uptake of bisphosphonates in vivo. Bone. 2008; 42(Suppl 1):S85.
Article29. Guise TA. Antitumor effects of bisphosphonates: promising preclinical evidence. Cancer Treat Rev. 2008; 34(Suppl 1):S19–24.
Article30. Lipton A. Emerging role of bisphosphonates in the clinic-antitumor activity and prevention of metastasis to bone. Cancer Treat Rev. 2008; 34(Suppl 1):S25–30.
Article31. Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004; 62:527–34.
Article32. Wood J, Bonjean K, Ruetz S, Bellahce ` ne A, Devy L, Foidart JM, et al. Novel antiangiogenic effects of the bisphosphonate compound zoledronic acid. J Pharmacol Exp Ther. 2002; 302:1055–61.
Article33. Estilo CL, Fornier M, Farooki A, Carlson D, Bohle G 3rd, Huryn JM. Osteonecrosis of the jaw related to bevacizumab. J Clin Oncol. 2008; 26:4037–8.
Article34. Somerman MJ, McCauley LK. Bisphosphonates: sacrificing the jaw to save the skeleton? Bonekey Osteovision. 2006; 3:12–8.
Article35. Lurie AG, Matteson SR. 99 M/Tc-diphosphonate bone imaging and uptake in healing rat extraction sockets. J Nucl Med. 1976; 17:688–92.36. McDougall IR. Skeletal scintigraphy. West J Med. 1979; 130:503–14.37. Hellstein JW, Marek CL. Bisphosphonate osteochemonecrosis (bis-phossy jaw): is this phossy jaw of the 21st century? J Oral Maxillofac Surg. 2005; 63:682–9.
Article38. Hansen T, Kunkel M, Springer E, Walter C, Weber A, Siegel E, et al. Actinomycosis of the jaws-histopathological study of 45 patients shows significant involvement in bisphosphonateassociated osteonecrosis and infected osteoradionecrosis. Virchows Arch. 2007; 451:1009–17.
Article39. Khamaisi M, Regev E, Yarom N, Avni B, Leitersdorf E, Raz I, et al. Possible association between diabetes and bisphosphonate-related jaw osteonecrosis. J Clin Endocrinol Metab. 2007; 92:1172–5.
Article40. Wessel JH, Dodson TB, Zavras AI. Zoledronate, smoking and obesity are strong risk factors for osteonecrosis of the jaw: a case-control study. J Oral Maxillofac Surg. 2008; 66:625–31.
Article41. Bamias A, Kastritis E, Bamia C, Moulopoulos LA, Melakopoulos I, Bozas G, et al. Osteonecrosis of the jaw in cancer after treatment with bisphosphonates: incidence and risk factors. J Clin Oncol. 2005; 23:8580–7.
Article42. Hoff AO, Toth BB, Altundag K, Guarneri V, Adamus A, Nooka AK, et al. Osteonecrosis of the jaw in patients receiving intravenous bisphosphonate therapy. ASCO Annual Meeting Proceedings (postmeeting edition). J Clin Oncol. 2006; 24(18 Suppl):8528.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Sinusitis due to Bisphosphonate Related Osteonecrosis of Jaw
- Dental implant treatment after healing of bisphosphonate-related osteonecrosis of the jaw (BRONJ) in the same region: a case report
- A Case of Intractable Bisphosphonate-Related Osteonecrosis of the Jaw Treated with Teriparatide
- Bisphosphonate Related Osteonecrosis of the Jaw (BRONJ): Position Statement of Korea
- Features of Histopathologic and radiographic findings in bisphosphonate-related osteonecrosis of jaw-Clinical review