J Korean Soc Radiol.
2011 Jan;64(1):25-32. 10.3348/jksr.2011.64.1.25.
Cervical Transforaminal Epidural Steroid Injection (TFESI): Role of MR Imaging and Epidurography
- Affiliations
-
- 1Department of Radiology, GangNeung Asan Hospital, University of Ulsan College of Medicine, Korea. sjchoi@gnah.co.kr
- 2Department of Orthopedic Surgery, GangNeung Asan Hospital, University of Ulsan College of Medicine, Korea.
- 3Department of Preventive Medicine, University of Kwandong College of Medicine, Korea.
- KMID: 1443578
- DOI: http://doi.org/10.3348/jksr.2011.64.1.25
Abstract
- PURPOSE
To evaluate the relationship between MR/epidurographic findings and the clinical outcome after a fluoroscopy-guided transforaminal epidural steroid injection (TFESI) in patients with cervical radicular pain.
MATERIALS AND METHODS
Forty-five patients who had taken a cervical TFESI in our department were included in this study. We retrospectively reviewed MR and epidurographic findings to see if there was a relationship between these methods and the amount of pain relief, by way of a multiple regression analysis.
RESULTS
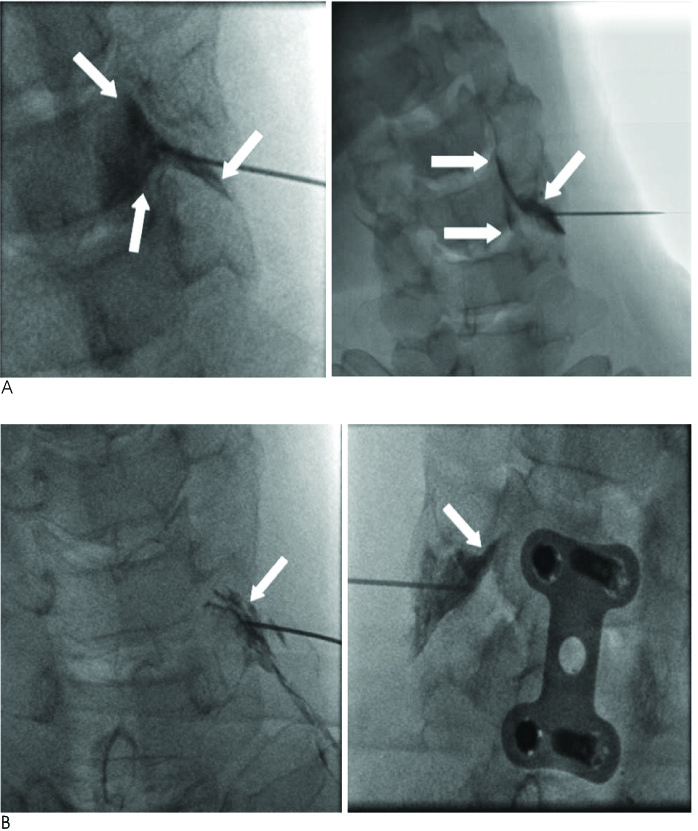
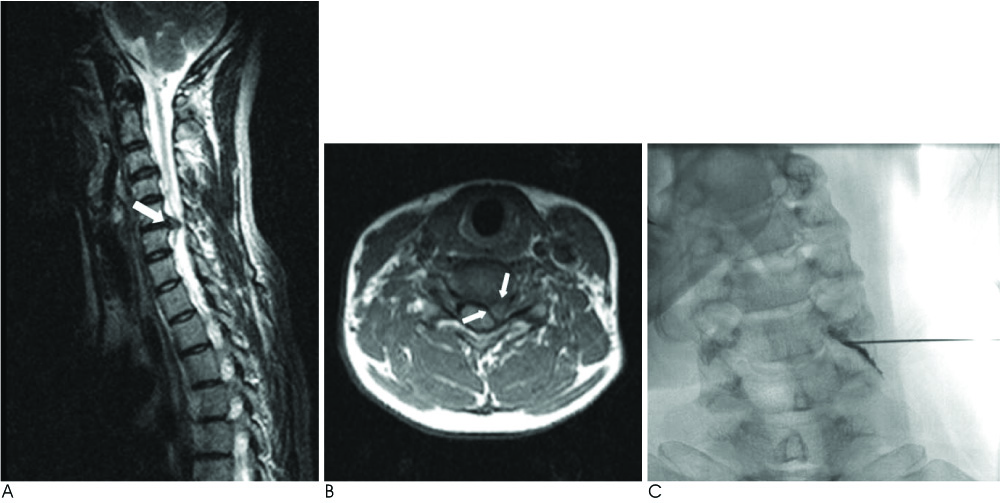
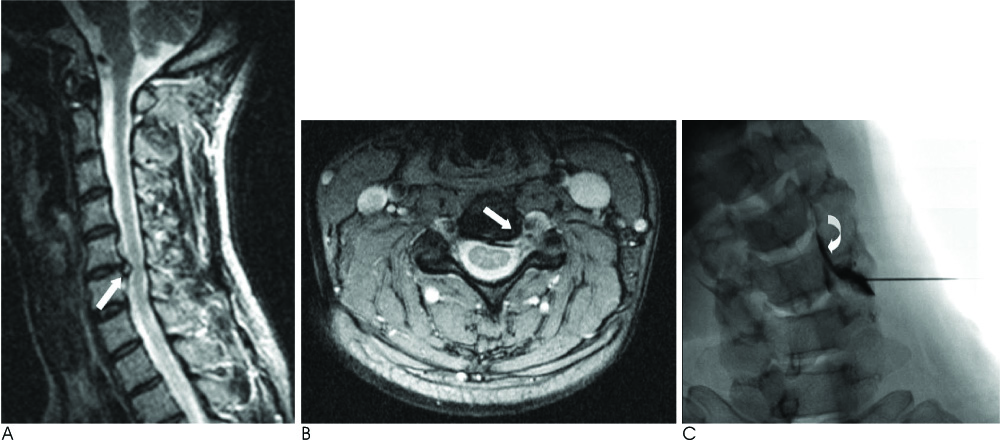
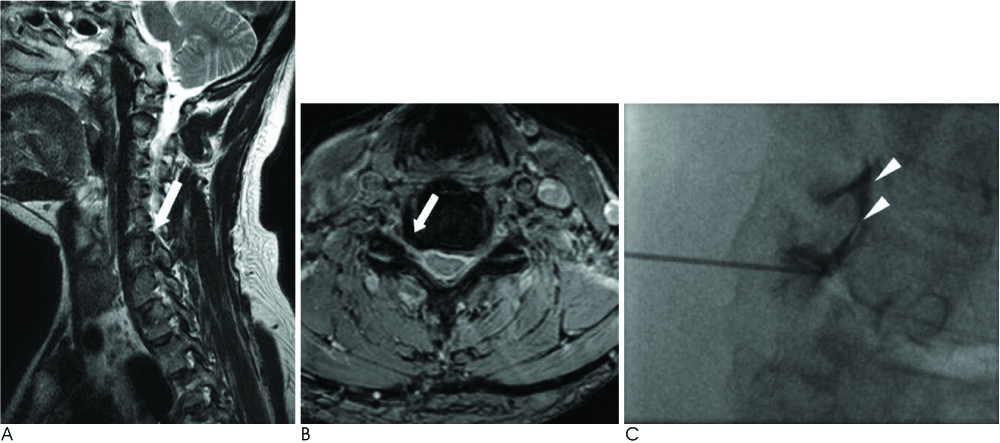
On MR imaging, there was significant relationship between the amount of pain relief and location of herniated intervertebral disc (HIVD, central: 54.4%, lateral recess: 69.4%, foraminal: 59%; p = 0.048). There was no significant difference regarding the other MR findings. On epidurographic findings, there was significant difference in the amount of pain relief with the extent of the contrast (epidural and epineural space, 65.3%; epineural space only, 64.2%; p = 0.03) and location of the needle tip (in the foramen, 59.4%; outside the foramen, 68.4%; p = 0.002).
CONCLUSION
The results indicate that TFESI could be more useful in patients with cervical HIVD in lateral recess rather than another location. Contrast spread into epidural reflux appears to be a favorable injection pattern. Needle tip location is recommended outside the foramen rather than in the foramen.
MeSH Terms
Figure
Cited by 1 articles
-
Musculoskeletal intervention
Jong Won Kwon
J Korean Med Assoc. 2015;58(6):502-515. doi: 10.5124/jkma.2015.58.6.502.
Reference
-
1. Slipman CW, Lipetz JS, Jackson HB, Rogers DP, Vresilovic EJ. Therapeutic selective nerve root block in the nonsurgical treatment of atraumatic cervical spondylotic radicular pain: a retrospective analysis with independent clinical review. Arch Phys Med Rehabil. 2000; 81:741–746.2. Bush K, Hiller S. Outcome of cervical radiculopathy treated with periradicular/epidural corticosteroid injections: a prospective study with independent clinical review. Eur Spine J. 1996; 5:319–325.3. Rathmell JP, Aprill C, Bogduk N. Cervical transforaminal injection of steroids. Anesthesiology. 2004; 100:1595–1600.4. Furman MB, Giovanniello MT, O'Brien EM. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Spine. 2003; 28:21–25.5. Brouwers PJ, Kottnik EJ, Simon MA, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001; 91:397–399.6. Baker R, Dreyfuss P, MercerS , Bogduk N. Cervical transforaminal injection of corticosteoids into a radicular artery: a possible mechanism for spinal cord injury. Pain. 2003; 103:211–215.7. Scanlon GC, Moeller-Bertram T, Romanowsky SM, Wallace MS. Cervical transforaminal epidural steroid injections: more dangerous than we think? Spine. 2007; 32:1249–1256.8. Boutin RD, Steinbach LS, Finnesey K. MR imaging of degenerative diseases in the cervical spine. . 2000; 8:471–490.9. Brown MN, Schwartz RH, Frank E, Blank NK. Preoperative evaluation of cervical radiculopathy and myelopathy by surface-coil MR imaging. AJR Am J Roentgenol. 1988; 151:1205–1212.10. Strobel K, Pfirrmann CW, Schmid M, Hoder J, Boos N, Zanetti M. Cervical nerve root blocks: indications and role of MR imaging. Radiology. 2004; 233:87–92.11. Choi SJ, Song JS, Kim C, Ryu DS, Ahn JH, Jung SM, et al. The use of magnetic resonance imaging to predict the clinical outcome of non-surgical treatment for lumbar intervertebral disc herniation. Korean J Radiol. 2007; 8:156–163.12. Jeong HS, Lee JW, Kim SH, Myung JS, Kim JH, Kim JH, et al. Effectiveness of transforaminal epidural steroid injection by using a preganglionic approach: a prospective randomized controlled study. Radiology. 2007; 245:584–590.13. Johnson BA, Schellhas KP, Pollei SR. Epidurography and therapeutic epidural injections: technical considerations and experience with 5334 cases. AJNR Am J Neuroradiol. 1999; 20:697–705.14. Manchikanti L, Cash KA, Pampati V, McManus CD, Damron KS. Evaluation of fluoroscopically guided caudal epidural injections. Pain Physician. 2004; 7:81–92.15. Botwin KP, Natalicchio J, Hanna A. Fluoroscopic guided lumbar interlaminar epidural injections: a prospective evaluation of epidurography contrast patterns and anatomincal review of the epidural space. Pain Physician. 2004; 7:77–80.16. Boswell MV, Shah RV, Everett CR, Sehgal N, McKenzie Brown AM, Abdi S, et al. Interventional techniques in the management of chronic spinal pain: evidence-based practice guidelines. Pain Physician. 2005; 8:1–47.17. Kubo Y, Waga S, Kojima T, Matsubara T, Kuga Y, Nakagawa Y. Microsurgical anatomy of the lower cervical spine and cord. Neurosurgery. 1994; 34:895–902.18. Ma DJ, Gilula LA, Riew KD. Complications of fluoroscopically guided extraforaminal cervical nerve blocks. An analysis of 1036 injections. J Bone Joint Surg Am. 2005; 87:1025–1030.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of L4-5 Transforaminal Epidural Steroid Injection in L5 Radiculopathy
- Comparison of incidence of intravascular injections during transforaminal epidural steroid injection using different needle types
- Spinal Cord Infarction after C7 Transforaminal Epidural Steroid Injection Using Dexamethasone
- Paraplegia after transforaminal epidural steroid injection in a patient with severe lumbar disc herniation - A case report -
- An Analysis of Pattern of Transforaminal Epidurography