Anesth Pain Med.
2021 Jan;16(1):96-102. 10.17085/apm.20068.
Paraplegia after transforaminal epidural steroid injection in a patient with severe lumbar disc herniation - A case report -
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul Sungsim General Hospital, Seoul, Korea
- KMID: 2512287
- DOI: http://doi.org/10.17085/apm.20068
Abstract
- Background
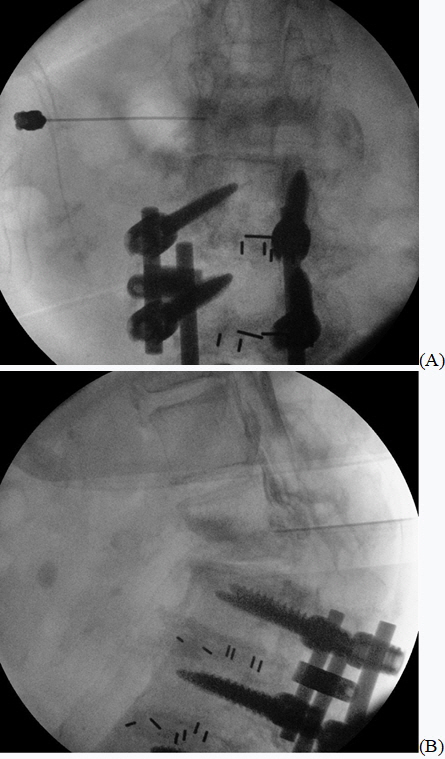
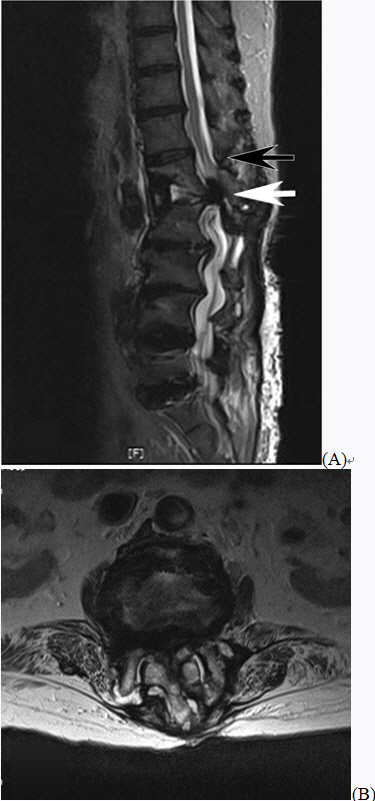
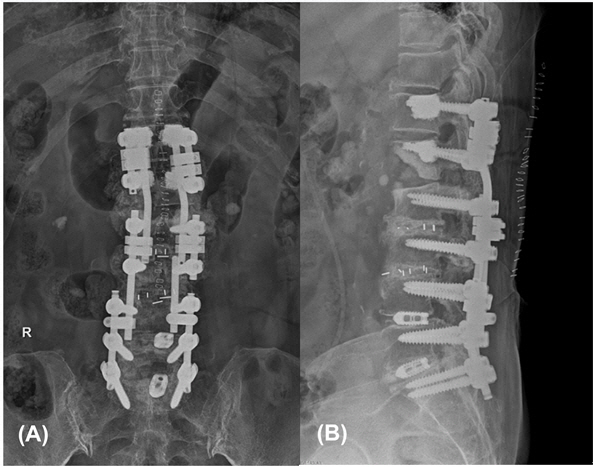
Transforaminal epidural steroid injection (TFESI) is a conservative treatment for patients with lumbar disc herniation (LDH). However, there are reports of various complications that can occur after TFESI; among these, paraplegia is a serious complication. Case: A 70-year-old woman who was unable to lie supine due to low back pain exacerbation during back extension underwent TFESI. After injection, there was pain relief and the patient was able to lie supine; however, paraplegia developed immediately. Magnetic resonance imaging confirmed cauda equina syndrome (CES) due to nerve compression from L1–2 LDH. We determined that the patient's LDH was already severe enough to be considered CES and that the TFESI procedure performed without an accurate understanding of the patient's condition aggravated the disease.
Conclusions
It is important to accurately determine the cause of pain and disease state of a patient to establish a correct treatment plan before TFESI is performed.
Figure
Reference
-
1. Zhong M, Liu JT, Jiang H, Mo W, Yu PF, Li XC, et al. Incidence of spontaneous resorption of lumbar disc herniation: a meta-analysis. Pain Physician. 2017; 20:E45–52.2. Andersson GB, Brown MD, Dvorak J, Herzog RJ, Kambin P, Malter A, et al. Consensus summary of the diagnosis and treatment of lumbar disc herniation. Spine (Phila Pa 1976). 1996; 21(24 Suppl):75S–8S.3. Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine (Phila Pa 1976). 2002; 27:11–6.4. Boswell MV, Shah RV, Everett CR, Sehgal N, McKenzie Brown AM, Abdi S, et al. Interventional techniques in the management of chronic spinal pain: evidence-based practice guidelines. Pain Physician. 2005; 8:1–47.5. Kennedy DJ, Dreyfuss P, Aprill CN, Bogduk N. Paraplegia following image-guided transforaminal lumbar spine epidural steroid injection: two case reports. Pain Med. 2009; 10:1389–94.6. Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D; CARE Group. The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol. 2014; 67:46–51.7. Dai LY, Xu YK, Zhang WM, Zhou ZH. The effect of flexion-extension motion of the lumbar spine on the capacity of the spinal canal. An experimental study. Spine (Phila Pa 1976). 1989; 14:523–5.8. Usubiaga JE, Wikinski JA, Usubiaga LE. Epidural pressure and its relation to spread of anesthetic solutions in epidural space. Anesth Analg. 1967; 46:440–6.9. Melissano G, Chiesa R. Advances in imaging of the spinal cord vascular supply and its relationship with paraplegia after aortic interventions. A review. Eur J Vasc Endovasc Surg. 2009; 38:567–77.10. Desai MJ, Dua S. Perineural hematoma following lumbar transforaminal steroid injection causing acute-on-chronic lumbar radiculopathy: a case report. Pain Pract. 2014; 14:271–7.11. Kuramoto A, Chang L, Graham J, Holmes S. Lumbar spinal stenosis with exacerbation of back pain with extension: a potential contraindication for supine MRI with sedation. J Neuroimaging. 2011; 21:92–4.12. Jinkins JR, Dworkin JS, Damadian RV. Upright, weight-bearing, dynamic-kinetic MRI of the spine: initial results. Eur Radiol. 2005; 15:1815–25.13. Verhagen AP, Downie A, Popal N, Maher C, Koes BW. Red flags presented in current low back pain guidelines: a review. Eur Spine J. 2016; 25:2788–802.14. Saal JA. Natural history and nonoperative treatment of lumbar disc herniation. Spine (Phila Pa 1976). 1996; 21(24 Suppl):2S–9S.15. Brouwers E, van de Meent H, Curt A, Starremans B, Hosman A, Bartels R. Definitions of traumatic conus medullaris and cauda equina syndrome: a systematic literature review. Spinal Cord. 2017; 55:886–90.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Two Methods of Epidural Steroid Injection in the Treatment of Recurrent Lumbar Disc Herniation
- Lumbar Epidural Venography in the Diagnosis of Lumbar Disc Herniation
- Inadvertent discogram during transforaminal epidural injection in patients with lumbar disc herniation: A report of 2 cases
- Comparison of Transforaminal Epidural Steroid Injection and Lumbar/Caudal Epidural Steroid Injection for the Treatment of Lumbosacral Radiculopathy
- Lumbar Ventral Epidural Approach