J Korean Orthop Assoc.
2012 Feb;47(1):15-20. 10.4055/jkoa.2012.47.1.15.
The Relationship between Soft Tissue Damages and Neurologic Deficits in Distractive Extension Injury of the Lower Cervical Spine
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Research Institute of Clinical Medicine, Chonbuk National University, Jeonju, Korea.
- 2Department of Orthopedic Surgery, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. alla1013@naver.com
- KMID: 1439987
- DOI: http://doi.org/10.4055/jkoa.2012.47.1.15
Abstract
- PURPOSE
To evaluate the relationship between the damage to anterior soft tissues and neurological deficit in distractive extension injury of the lower cervical spine.
MATERIALS AND METHODS
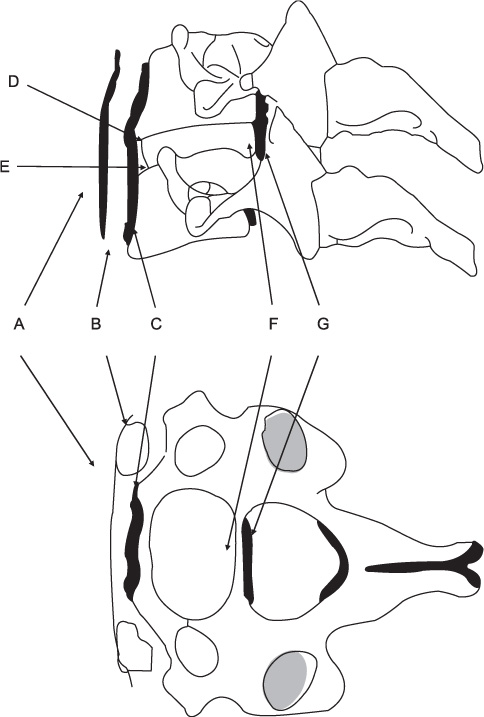
Ninety-two patients who were treated surgically for distractive extension injury of the lower cervical spine were included in this study. Soft tissue swelling was evaluated on plain radiographs. Damage to the longus colli muscle, anterior longitudinal ligament, superior end plate, inferior end plate, annulus fibrosus, and posterior longitudinal ligament were intraoperatively checked and the relationship between these findings and clinical neurologic deficits was analyzed.
RESULTS
Soft tissue swelling was increased to 92% in the retropharyngeal space and to 89% in the retrotracheal space but there was no significant difference. No relationship was found between the damage to the prevertebral fascia, longus colli muscle and neurological deficit. Injuries to the inferior end plate and annulus fibrosus showed a directly propotional relation with neurological deficit, but it was not significant. Injuries to the anterior longitudinal ligament (p<0.01), superior end plate (p=0.02), posterior longitudinal ligament (p=0.04) showed significant relations with neurological deficit.
CONCLUSION
The distractive extension injury combined with the damage to the anterior longitudinal ligament, superior end plate or posterior longitudinal ligament showed high frequency of neurological deficit. Hence, these are regarded as the important structures for maintaining the stability of the lower cervical spine.
Figure
Reference
-
1. Allen BL Jr, Ferguson RL, Lehmann TR, O'Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976). 1982. 7:1–27.
Article2. Harris JH, Yeakley JW. Hyperextension-dislocation of the cervical spine. Ligament injuries demonstrated by magnetic resonance imaging. J Bone Joint Surg Br. 1992. 74:567–570.
Article3. Harris WH, Hamblen DL, Ojemann RG. Traumatic disruption of cervical intervertebral disk from hyperextension injury. Clin Orthop Relat Res. 1968. 60:163–167.
Article4. Song KJ, Bae HK, Koh DH. Diagnosis in extension injuries of the lower cervical spine. J Korean Orthop Assoc. 2003. 38:172–178.
Article5. Marar BC. Hyperextension injuries of the cervical spine. The pathogenesis of damage to the spinal cord. J Bone Joint Surg Am. 1974. 56:1655–1662.6. Schaefer DM, Flanders A, Northrup BE, Doan HT, Osterholm JL. Magnetic resonance imaging of acute cervical spine trauma. Correlation with severity of neurologic injury. Spine (Phila Pa 1976). 1989. 14:1090–1095.7. Song KJ, Kim GH, Lee KB. The efficacy of the modified classification system of soft tissue injury in extension injury of the lower cervical spine. Spine (Phila Pa 1976). 2008. 33:E488–E493.
Article8. Marino RJ, Barros T, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2003. 26:Suppl 1. S50–S56.
Article9. Taylor AR, Blackwood W. Paraplegia in hyperextension cervical injuries with normal radiographic appearances. J Bone Joint Surg Br. 1948. 30B:245–248.
Article10. Penning L. Some aspects of plain radiography of the cervical spine in chronic myelopathy. Neurology. 1962. 12:513–519.
Article11. Stauffer ES, MacMillan M. Rockwood CA, Green DP, Bucholz RW, Heckman JD, editors. Fractures and dislocations of the cervical spine. Rockwood and Green's fractures in adults. 1996. 4th ed. Philadelphia: Lippincott-Raven Publishers.12. Dunn EJ, Blazar S. Soft-tissue injuries of the lower cervical spine. Instr Course Lect. 1987. 36:499–512.13. Akaishi F. Biomechanical properties of the anterior and posterior longitudinal ligament in the cervical spine. Nihon Ika Daigaku Zasshi. 1995. 62:360–368.
Article14. Myklebust JB, Pintar F, Yoganandan N, et al. Tensile strength of spinal ligaments. Spine (Phila Pa 1976). 1988. 13:526–531.
Article15. Yoganandan N, Stemper BD, Pintar FA, Baisden JL, Shender BS, Paskoff G. Normative segment-specific axial and coronal angulation corridors of subaxial cervical column in axial rotation. Spine (Phila Pa 1976). 2008. 33:490–496.
Article16. Rizzolo SJ, Piazza MR, Cotler JM, Balderston RA, Schaefer D, Flanders A. Intervertebral disc injury complicating cervical spine trauma. Spine (Phila Pa 1976). 1991. 16:6 Suppl. S187–S189.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Soft Tissue Damage in Cervical Spine Extension Injury
- Relationship between Soft Tissue Damages and Spinal Cord Injury in Lower Cervical Spine Trauma
- Clinical Analysis of Lower Cervical Spine Injury according to Injury Mechanism: Data of 277 Surgical Patients
- Airway Compression as a Result of Extensive Prevertebral Hematoma Following Extension Injury of Lower Cervical Spine without Fracture/Dislocation
- Diagnosis in Extension Injuries of the Lower Cervical Spine