J Korean Orthop Assoc.
2012 Aug;47(4):264-270. 10.4055/jkoa.2012.47.4.264.
Clinical Analysis of Lower Cervical Spine Injury according to Injury Mechanism: Data of 277 Surgical Patients
- Affiliations
-
- 1Department of Orthopedic Surgery, Chonbuk National University Hospital, Chonbuk National University Medical School, Research Institute of Clinical Medicine, Biomedical Science Institute, Jeonju, Korea. osdr2815@naver.com
- KMID: 2185373
- DOI: http://doi.org/10.4055/jkoa.2012.47.4.264
Abstract
- PURPOSE
To analyze the incidence and treatment outcomes of lower cervical spine injury since there is no long term, large Korean data available.
MATERIALS AND METHODS
We analyzed 277 patients with lower cervical spine injury who underwent surgical treatments between May 1994 and October 2008. The injury types are based on Allen's classification, and neurologic injury was classified as complete, incomplete cord injury, root injury and no neurologic status. We analyzed postoperative complications, neurologic recovery and the relief of pain.
RESULTS
Distractive-extension injury occurred most commonly in 140 patients (50.5%). Neurologic injury was detected in 232 cases (83.8%); 46 (16.6%) complete cord injury; 154 (55.6%) incomplete cord injury; and 32 (11.6%) root injury. Incomplete cord injury of distractive extension injury was poorly recovered. Clinical outcomes demonstrated improvement compared with the preoperative values in mean visual analogue scale. Complications were respiratory failure, neurogenic bladder, urinary tract infection and gastritis.
CONCLUSION
This study showed the highest incidence of distractive extension injury and neurologic injury contrary to previous studies. This result was caused by the use of plain radiograph to establish Allen's classification in the past. Therefore, we suggest the use of magnetic resonance imaging for evaluating soft tissue injury with Allen's classification to achieve accurate assessment.
MeSH Terms
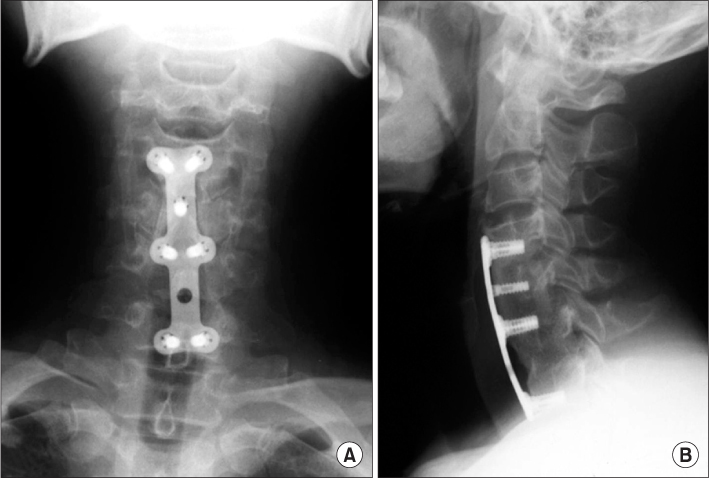
Figure
Reference
-
1. Cho DY, Seo JG, Baek SN, Kim KY, Kim YT. Surgical treatment of the unstable lower cervical spine injuries. J Korean Orthop Assoc. 1990. 25:151–160.
Article2. Durbin FC. Fracture-dislocations of the cervical spine. J Bone Joint Surg Br. 1957. 39:23–38.
Article3. Penning L. Normal movements of the cervical spine. AJR Am J Roentgenol. 1978. 130:317–326.
Article4. Allen BL Jr, Ferguson RL, Lehmann TR, O'Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976). 1982. 7:1–27.
Article5. Denis F. Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin Orthop Relat Res. 1984. 189:65–76.
Article6. Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970. 52:1534–1551.
Article7. Kahn EA, Schneider RC. Chronic neurological sequelae of acute trauma to the spine and spinal cord. I. The significance of the acute-flexion or tear-drop fracture-dislocation of the cervical spine. J Bone Joint Surg Am. 1956. 38:985–997.8. Taylor AR, Blackwood W. Paraplegia in hyperextension cervical injuries with normal radiographic appearances. J Bone Joint Surg Br. 1948. 30B:245–248.
Article9. Vaccaro AR, Madigan L, Schweitzer ME, Flanders AE, Hilibrand AS, Albert TJ. Magnetic resonance imaging analysis of soft tissue disruption after flexion-distraction injuries of the subaxial cervical spine. Spine (Phila Pa 1976). 2001. 26:1866–1872.
Article10. Barnes R. Paraplegia in cervical spine injuries. J Bone Joint Surg Br. 1948. 30B:234–244.
Article11. Castellano V, Bocconi FL. Injuries of the cervical spine with spinal cord involvement (myelic fractures): statistical considerations. Bull Hosp Joint Dis. 1970. 31:188–194.12. Bedbrook GM. Pathological principles in the management of spinal cord trauma. Paraplegia. 1966. 4:43–56.
Article13. Song KJ, Shin PS. Surgical treatment of lower cervical spine injury. J Korean Orthop Assoc. 1999. 34:117–126.
Article14. Guttmann L, Frankel H. The value of intermittent catheterisation in the early management of traumatic paraplegia and tetraplegia. Paraplegia. 1966. 4:63–84.
Article15. Song KJ, Lee KB. The prognosis of the acute cervical spinal cord injury. J Korean Orthop Assoc. 1998. 33:794–801.
Article16. Song KJ, Lee KR. The significance of space available for the spinal cord at the injured level in the lower cervical spine fractures and dislocations. J Korean Orthop Assoc. 1997. 32:1070–1077.
Article17. Ikata T, Iwasa K, Morimoto K, Tonai T, Taoka Y. Clinical considerations and biochemical basis of prognosis of cervical spinal cord injury. Spine (Phila Pa 1976). 1989. 14:1096–1101.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vertebral Artery Injury during Anterior Cervical Spine Surgery: Report of Two Cases
- An Analysis of Operative Treatment of Lower Cervical Spine Injury
- Epidemiology and Management of Iatrogenic Vertebral Artery Injury Associated With Cervical Spine Surgery
- Missed Traumatic Cervical Spine Injury
- Pattern of Cervical Spine Injury in Patients with a Facial Fracture