J Korean Soc Radiol.
2012 Jun;66(6):507-517. 10.3348/jksr.2012.66.6.507.
Ultrasonographic Findings of Foreign-Body Granulomas after Endoscopic Thyroidectomy via an Axillo-Breast Approach
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University College of Medicine, Bucheon Hospital, Bucheon, Korea. hshong@schmc.ac.kr
- 2Department of Nuclear Medicine, Soonchunhyang University College of Medicine, Bucheon Hospital, Bucheon, Korea.
- 3Department of Pathology, Soonchunhyang University College of Medicine, Bucheon Hospital, Bucheon, Korea.
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Soonchunhyang University College of Medicine, Bucheon Hospital, Bucheon, Korea.
- KMID: 1439467
- DOI: http://doi.org/10.3348/jksr.2012.66.6.507
Abstract
- PURPOSE
To assess the ultrasonographic (US) findings of foreign body granulomas detected by endoscopic thyroidectomy.
MATERIALS AND METHODS
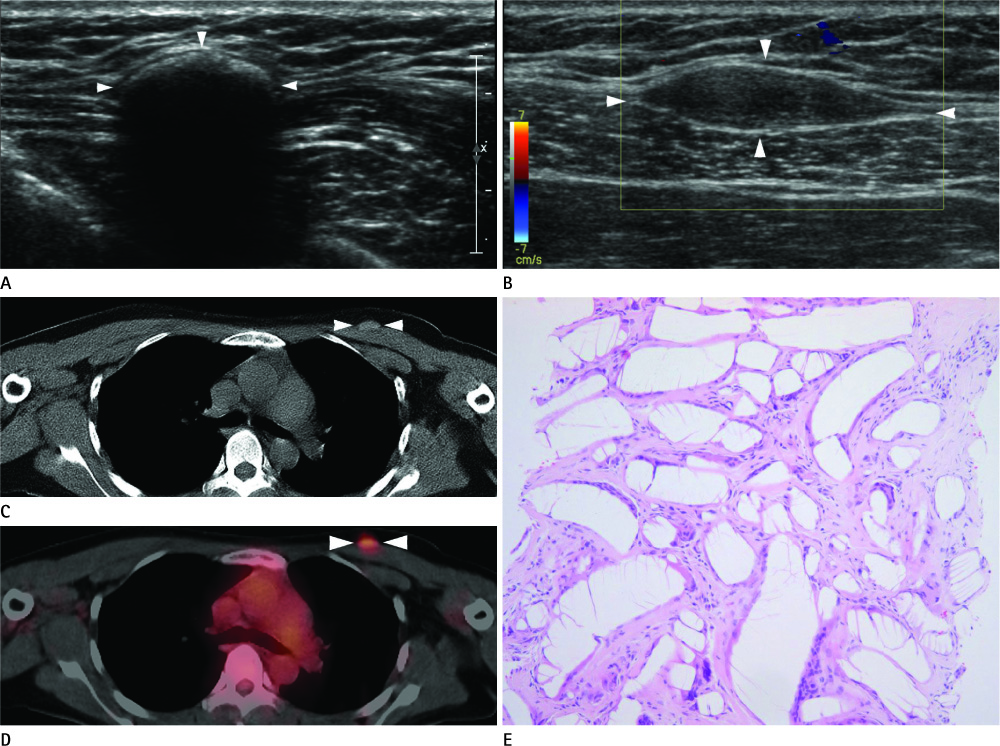
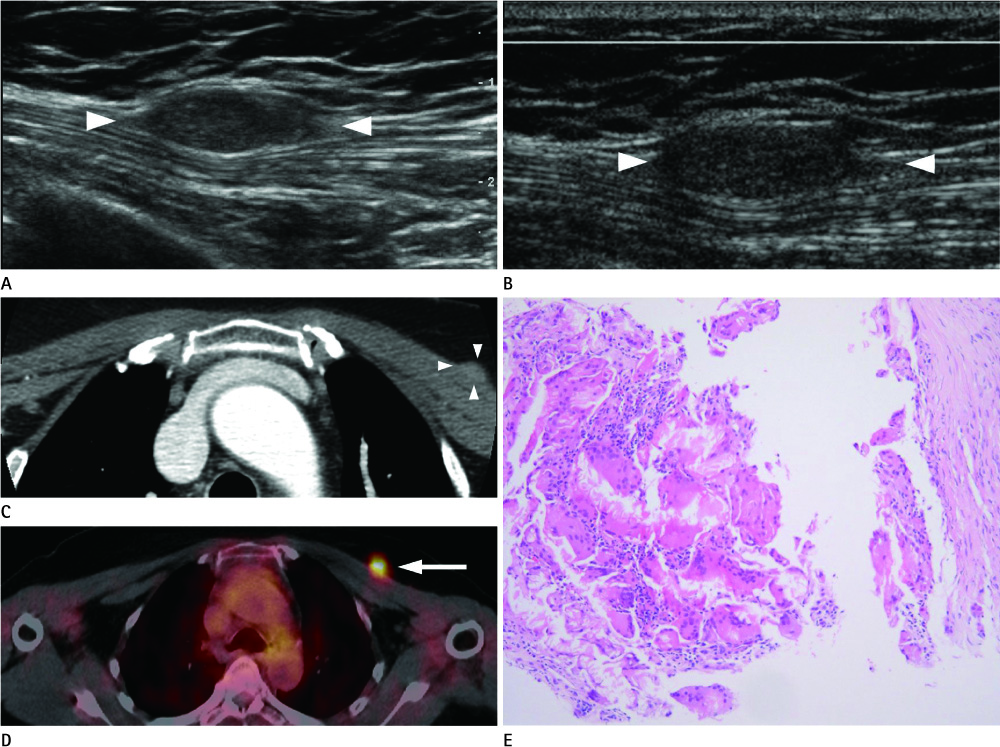
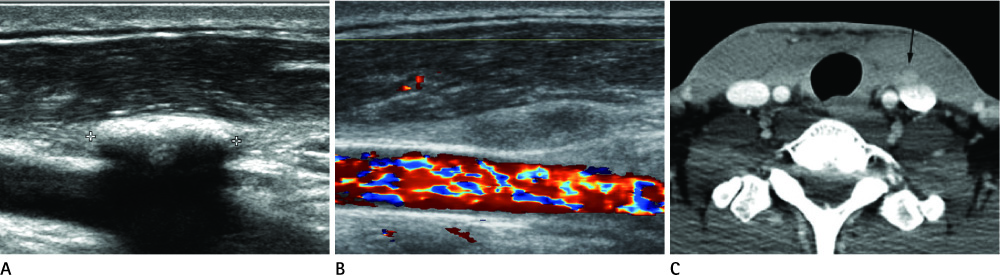
On positron emission tomography-computed tomography of patients who had undergone endoscopic thyroidectomy, we encountered three fluorodeoxyglucose uptaken lesions in the surgical bed and those were pathologically confirmed to be foreign body granulomas. Additionally, 10 lesions demonstrating the same US findings were clinically diagnosed as foreign body granulomas. Echogenicity, shape, size, location, and vascularity were evaluated on US. Eleven lesions were subjected to follow-up US.
RESULTS
On US, seven lesions were found to be hyperechoic linear lesions with posterior acoustic shadowing while six other lesions were oval, iso- to slightly hypoechoic lesions. No vascularity was observed on color Doppler US. The size of the lesions was inversely correlated with the time to lesion detection (Spearman's correlation r = -0.6528; p = 0.02). Oval iso- to slightly hypoechoic lesions (mean, 672 days) had statistically longer times from the time of thyroidectomy to lesion detection on US than hyperechoic linear lesions (mean, 318 days; Mann-Whitney test, p = 0.02). On follow-up US, the lesions had decreased in size and hyperechoic linear lesions became oval iso- to slightly hypoechoic lesions.
CONCLUSION
In patients who underwent endoscopic thyroidectomy, characteristic US findings and evolutional changes are helpful for the diagnosis of foreign body granulomas and to distinguish from recurrent thyroid cancer, thus avoiding invasive procedures.
MeSH Terms
Figure
Reference
-
1. Hong HJ, Kim WS, Koh YW, Lee SY, Shin YS, Koo YC, et al. Endoscopic thyroidectomy via an axillo-breast approach without gas insufflation for benign thyroid nodules and micropapillary carcinomas: preliminary results. Yonsei Med J. 2011; 52:643–654.2. Colonna M, Guizard AV, Schvartz C, Velten M, Raverdy N, Molinie F, et al. A time trend analysis of papillary and follicular cancers as a function of tumour size: a study of data from six cancer registries in France (1983-2000). Eur J Cancer. 2007; 43:891–900.3. Ohgami M, Ishii S, Arisawa Y, Ohmori T, Noga K, Furukawa T, et al. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech. 2000; 10:1–4.4. Shimizu K, Tanaka S. Asian perspective on endoscopic thyroidectomy -- a review of 193 cases. Asian J Surg. 2003; 26:92–100.5. Yoon JH, Park CH, Chung WY. Gasless endoscopic thyroidectomy via an axillary approach: experience of 30 cases. Surg Laparosc Endosc Percutan Tech. 2006; 16:226–231.6. Choe JH, Kim SW, Chung KW, Park KS, Han W, Noh DY, et al. Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg. 2007; 31:601–606.7. Koh YW, Park JH, Kim JW, Lee SW, Choi EC. Endoscopic hemithyroidectomy with prophylactic ipsilateral central neck dissection via an unilateral axillo-breast approach without gas insufflation for unilateral micropapillary thyroid carcinoma: preliminary report. Surg Endosc. 2010; 24:188–197.8. Shimazu K, Shiba E, Tamaki Y, Takiguchi S, Taniguchi E, Ohashi S, et al. Endoscopic thyroid surgery through the axillo-bilateral-breast approach. Surg Laparosc Endosc Percutan Tech. 2003; 13:196–201.9. Antonelli A, Miccoli P, Ferdeghini M, Di Coscio G, Alberti B, Iacconi P, et al. Role of neck ultrasonography in the follow-up of patients operated on for thyroid cancer. Thyroid. 1995; 5:25–28.10. Frasoldati A, Pesenti M, Gallo M, Caroggio A, Salvo D, Valcavi R. Diagnosis of neck recurrences in patients with differentiated thyroid carcinoma. Cancer. 2003; 97:90–96.11. Sutton RT, Reading CC, Charboneau JW, James EM, Grant CS, Hay ID. US-guided biopsy of neck masses in postoperative management of patients with thyroid cancer. Radiology. 1988; 168:769–772.12. Frasoldati A, Toschi E, Zini M, Flora M, Caroggio A, Dotti C, et al. Role of thyroglobulin measurement in fine-needle aspiration biopsies of cervical lymph nodes in patients with differentiated thyroid cancer. Thyroid. 1999; 9:105–111.13. Lee MJ, Ross DS, Mueller PR, Daniels GH, Dawson SL, Simeone JF. Fine-needle biopsy of cervical lymph nodes in patients with thyroid cancer: a prospective comparison of cytopathologic and tissue marker analysis. Radiology. 1993; 187:851–854.14. Pacini F, Fugazzola L, Lippi F, Ceccarelli C, Centoni R, Miccoli P, et al. Detection of thyroglobulin in fine needle aspirates of nonthyroidal neck masses: a clue to the diagnosis of metastatic differentiated thyroid cancer. J Clin Endocrinol Metab. 1992; 74:1401–1404.15. Simeone JF, Daniels GH, Hall DA, McCarthy K, Kopans DB, Butch RJ, et al. Sonography in the follow-up of 100 patients with thyroid carcinoma. AJR Am J Roentgenol. 1987; 148:45–49.16. Grant CS, Hay ID, Gough IR, Bergstralh EJ, Goellner JR, McConahey WM. Local recurrence in papillary thyroid carcinoma: is extent of surgical resection important? Surgery. 1988; 104:954–962.17. McConahey WM, Hay ID, Woolner LB, van Heerden JA, Taylor WF. Papillary thyroid cancer treated at the Mayo Clinic, 1946 through 1970: initial manifestations, pathologic findings, therapy, and outcome. Mayo Clin Proc. 1986; 61:978–996.18. Kim JH, Lee JH, Shong YK, Hong SJ, Ko MS, Lee DH, et al. Ultrasound features of suture granulomas in the thyroid bed after thyroidectomy for papillary thyroid carcinoma with an emphasis on their differentiation from locally recurrent thyroid carcinomas. Ultrasound Med Biol. 2009; 35:1452–1457.19. Ko MS, Lee JH, Shong YK, Gong GY, Baek JH. Normal and abnormal sonographic findings at the thyroidectomy sites in postoperative patients with thyroid malignancy. AJR Am J Roentgenol. 2010; 194:1596–1609.20. Langer JE, Luster E, Horii SC, Mandel SJ, Baloch ZW, Coleman BG. Chronic granulomatous lesions after thyroidectomy: imaging findings. AJR Am J Roentgenol. 2005; 185:1350–1354.21. Lee JH, Lee HK, Lee DH, Choi CG, Gong G, Shong YK, et al. Ultrasonographic findings of a newly detected nodule on the thyroid bed in postoperative patients for thyroid carcinoma: correlation with the results of ultrasonography-guided fine-needle aspiration biopsy. Clin Imaging. 2007; 31:109–113.22. Shin JH, Han BK, Ko EY, Kang SS. Sonographic findings in the surgical bed after thyroidectomy: comparison of recurrent tumors and nonrecurrent lesions. J Ultrasound Med. 2007; 26:1359–1366.23. Kim JH, Choi YJ, Kim JA, Gil WH, Nam SJ, Oh YL, et al. Thyroid cancer that developed around the operative bed and subcutaneous tunnel after endoscopic thyroidectomy via a breast approach. Surg Laparosc Endosc Percutan Tech. 2008; 18:197–201.24. Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K, et al. Needle tract implantation of papillary thyroid carcinoma after fine-needle aspiration biopsy. World J Surg. 2005; 29:1544–1549.25. Lee YS, Yun JS, Jeong JJ, Nam KH, Chung WY, Park CS. Soft tissue implantation of thyroid adenomatous hyperplasia after endoscopic thyroid surgery. Thyroid. 2008; 18:483–484.26. Schaeff B, Paolucci V, Thomopoulos J. Port site recurrences after laparoscopic surgery. A review. Dig Surg. 1998; 15:124–134.27. Kamaya A, Gross M, Akatsu H, Jeffrey RB. Recurrence in the thyroidectomy bed: sonographic findings. AJR Am J Roentgenol. 2011; 196:66–70.28. Ferrozzi F, Bova D, Gabrielli M. Foreign-body granuloma of the kidney: CT, MR and pathologic correlation. Eur Radiol. 1999; 9:1590–1592.29. Helms CA, Clark RE. Post-herniorrhaphy suture granuloma simulating a bladder neoplasm. Radiology. 1977; 124:56.30. Kim SW, Shin HC, Kim IY, Baek MJ, Cho HD. Foreign body granulomas simulating recurrent tumors in patients following colorectal surgery for carcinoma: a report of two cases. Korean J Radiol. 2009; 10:313–318.31. Pearl GS, Someren A. Suture granuloma simulating bladder neoplasm. Urology. 1980; 15:304–306.32. Yeretsian RA, Blodgett TM, Branstetter BF 4th, Roberts MM, Meltzer CC. Teflon-induced granuloma: a false-positive finding with PET resolved with combined PET and CT. AJNR Am J Neuroradiol. 2003; 24:1164–1166.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Thyroidectomy via an Axillo-bilateral Breast Approach: 5 Years of Experience
- Bilateral axillo-breast approach robotic total thyroidectomy without isthmectomy: a case report
- Endoscopic Removal of Parathyroid Tumors via an Unilateral Axillo-Breast Approach
- Evaluation of Surgical Completeness in Endoscopic Total Thyroidectomy with Central Neck Dissection via a Unilateral Axillo-Breast Approach Compared with Bilateral Axillo-Breast and Open Approach
- Endoscopic Thyroidectomy