J Korean Soc Transplant.
2012 Mar;26(1):1-5. 10.4285/jkstn.2012.26.1.1.
Liver Transplantation for the Curative Treatment of Hilar Cholangiocarcinoma: Model of the Mayo Clinic
- Affiliations
-
- 1Division of Hepato-Biliary-Pancreatic Surgery, Department of Surgery, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea. kjkang@dsmc.or.kr
- KMID: 1435075
- DOI: http://doi.org/10.4285/jkstn.2012.26.1.1
Abstract
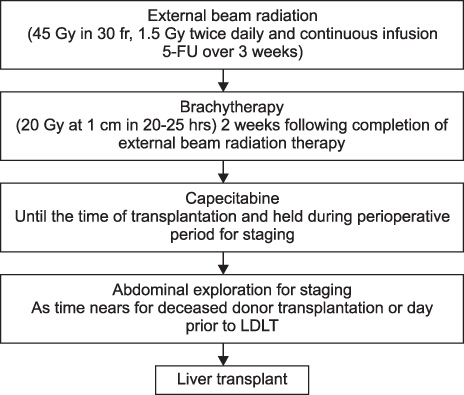
- Liver transplantation for treating cholangiocarcinoma (CCA) has potential benefits in terms of accomplishing radical resection even in patients with unresectable tumor and treating underlying disease such as primary sclerosing cholangitis (PSC). Despite this ideal rationale, the initial results of liver transplantation alone for CCA have been uniformly poor. Because of a high recurrence rate and a poor survival rate, CCA has been viewed as an absolute contraindication for transplantation. However, from the 1990s, liver transplantation following high dose neoadjuvant radiotherapy with chemotherapy has achieved excellent results, in a few medical centers, for selected patients with unresectable hilar CCA arising in the setting of PSC. Especially, the Mayo Clinic reported a 5-year survival rate of 73% for 120 patients in 2010 by performing neoadjuvant therapy and liver transplantation. We reviewed the results of liver transplantation in patients with hilar CCA and the protocol of the Mayo Clinic to consider the feasibility of liver transplantation for Korean patients with hilar CCA. Although liver transplantation with neoadjuvant therapy cannot be applied to most Korean patients due to the different disease entities and the good results with performing radical surgical resection, it can be considered as an alternative curative treatment option for selected patients with anatomically unresectable hilar CCA or CCA arising in the setting of PSC.
MeSH Terms
Figure
Reference
-
1. Burak K, Angulo P, Pasha TM, Egan K, Petz J, Lindor KD. Incidence and risk factors for cholangiocarcinoma in primary sclerosing cholangitis. Am J Gastroenterol. 2004. 99:523–526.
Article2. Shin HR, Oh JK, Lim MK, Shin A, Kong HJ, Jung KW, et al. Descriptive epidemiology of cholangiocarcinoma and clonorchiasis in Korea. J Korean Med Sci. 2010. 25:1011–1016.
Article3. Kondo S, Hirano S, Ambo Y, Tanaka E, Okushiba S, Morikawa T, et al. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Ann Surg. 2004. 240:95–101.
Article4. Hong JC, Jones CM, Duffy JP, Petrowsky H, Farmer DG, French S, et al. Comparative analysis of resection and liver transplantation for intrahepatic and hilar cholangiocarcinoma: a 24-year experience in a single center. Arch Surg. 2011. 146:683–689.
Article5. Meyer CG, Penn I, James L. Liver transplantation for cholangiocarcinoma: results in 207 patients. Transplantation. 2000. 69:1633–1637.6. Brandsaeter B, Isoniemi H, Broomé U, Olausson M, Bäckman L, Hansen B, et al. Liver transplantation for primary sclerosing cholangitis; predictors and consequences of hepatobiliary malignancy. J Hepatol. 2004. 40:815–822.
Article7. Robles R, Figueras J, Turrión VS, Margarit C, Moya A, Varo E, et al. Spanish experience in liver transplantation for hilar and peripheral cholangiocarcinoma. Ann Surg. 2004. 239:265–271.
Article8. Rosen CB, Heimbach JK, Gores GJ. Liver transplantation for cholangiocarcinoma. Transpl Int. 2010. 23:692–697.
Article9. Ghali P, Marotta PJ, Yoshida EM, Bain VG, Marleau D, Peltekian K, et al. Liver transplantation for incidental cholangiocarcinoma: analysis of the Canadian experience. Liver Transpl. 2005. 11:1412–1416.
Article10. Seehofer D, Thelen A, Neumann UP, Veltzke-Schlieker W, Denecke T, Kamphues C, et al. Extended bile duct resection and [corrected] liver and transplantation in patients with hilar cholangiocarcinoma: long-term results. Liver Transpl. 2009. 15:1499–1507.
Article11. Shimoda M, Farmer DG, Colquhoun SD, Rosove M, Ghobrial RM, Yersiz H, et al. Liver transplantation for cholangiocellular carcinoma: analysis of a single-center experience and review of the literature. Liver Transpl. 2001. 7:1023–1033.
Article12. Foo ML, Gunderson LL, Bender CE, Buskirk SJ. External radiation therapy and transcatheter iridium in the treatment of extrahepatic bile duct carcinoma. Int J Radiat Oncol Biol Phys. 1997. 39:929–935.
Article13. Sudan D, DeRoover A, Chinnakotla S, Fox I, Shaw B Jr, McCashland T, et al. Radiochemotherapy and transplantation allow long-term survival for nonresectable hilar cholangiocarcinoma. Am J Transplant. 2002. 2:774–779.
Article14. Heimbach JK, Gores GJ, Haddock MG, Alberts SR, Nyberg SL, Ishitani MB, et al. Liver transplantation for unresectable perihilar cholangiocarcinoma. Semin Liver Dis. 2004. 24:201–207.
Article15. Rea DJ, Rosen CB, Nagorney DM, Heimbach JK, Gores GJ. Transplantation for cholangiocarcinoma: when and for whom? Surg Oncol Clin N Am. 2009. 18:325–337.
Article16. Farley DR, Weaver AL, Nagorney DM. "Natural history" of unresected cholangiocarcinoma: patient outcome after noncurative intervention. Mayo Clin Proc. 1995. 70:425–429.
Article17. Tsao JI, Nimura Y, Kamiya J, Hayakawa N, Kondo S, Nagino M, et al. Management of hilar cholangiocarcinoma: comparison of an American and a Japanese experience. Ann Surg. 2000. 232:166–174.18. Igami T, Nishio H, Ebata T, Yokoyama Y, Sugawara G, Nimura Y, et al. Surgical treatment of hilar cholangiocarcinoma in the "new era": the Nagoya University experience. J Hepatobiliary Pancreat Sci. 2010. 17:449–454.
Article19. Lee SG, Song GW, Hwang S, Ha TY, Moon DB, Jung DH, et al. Surgical treatment of hilar cholangiocarcinoma in the new era: the Asan experience. J Hepatobiliary Pancreat Sci. 2010. 17:476–489.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical management of hilar cholangiocarcinoma: Controversies and recommendations
- Current treatment outcome of hilar cholangiocarcinoma
- Hilar Cholangiocarcinoma: Recent update of radiologic assessment
- Utility of Serum YKL-40 as a Tumor-Specific Marker of Hepatobiliary Malignancies
- Current Status and Recent Update of Imaging Evaluation for Peri-Hilar Cholangiocarcinoma