Ann Hepatobiliary Pancreat Surg.
2023 Aug;27(3):227-240. 10.14701/ahbps.23-028.
Surgical management of hilar cholangiocarcinoma: Controversies and recommendations
- Affiliations
-
- 1Department of Surgical Gastroenterology and Liver Transplantation, Sir Ganga Ram Hospital, New Delhi, India
- KMID: 2545716
- DOI: http://doi.org/10.14701/ahbps.23-028
Abstract
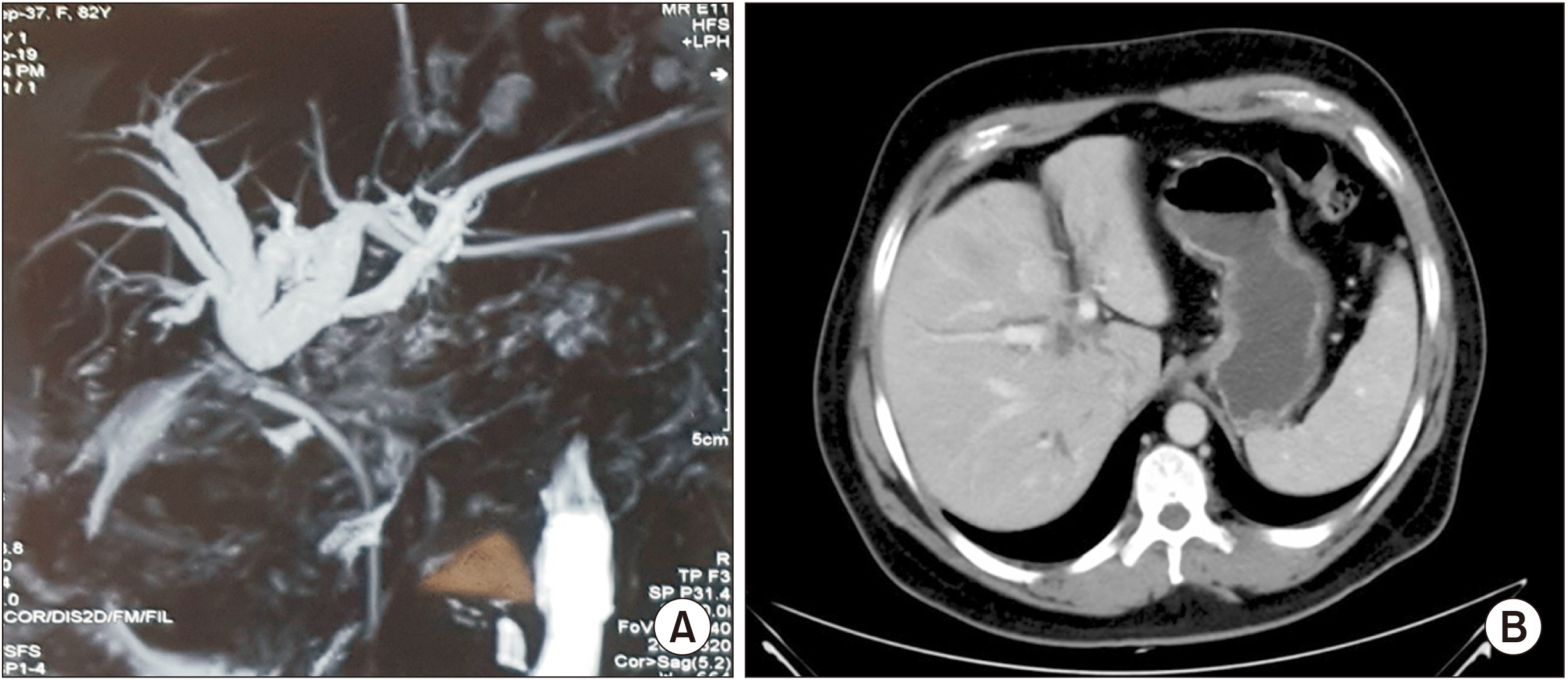
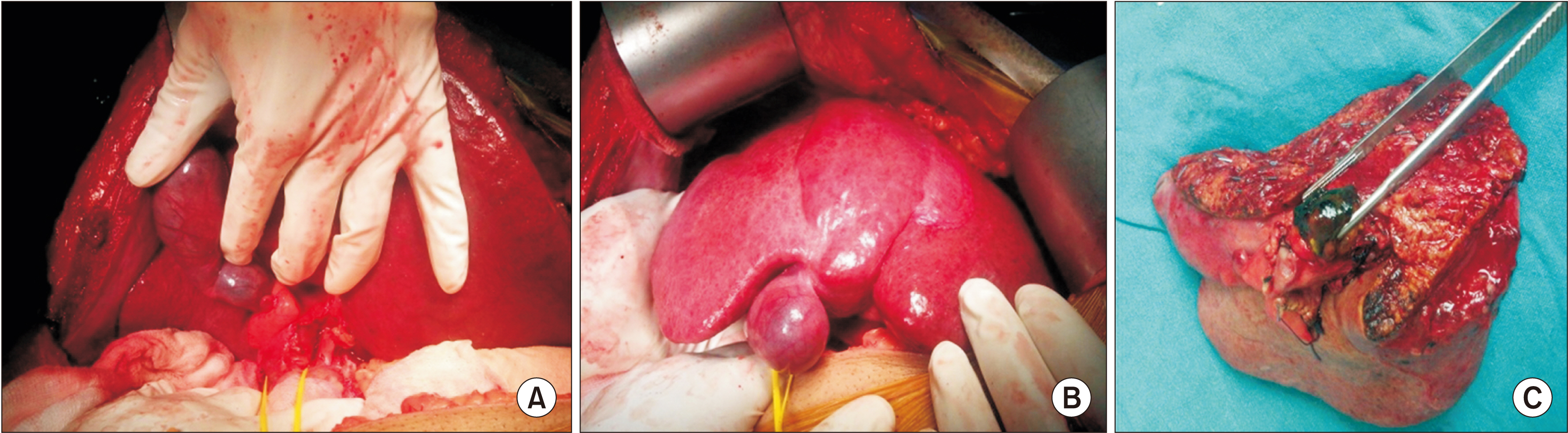
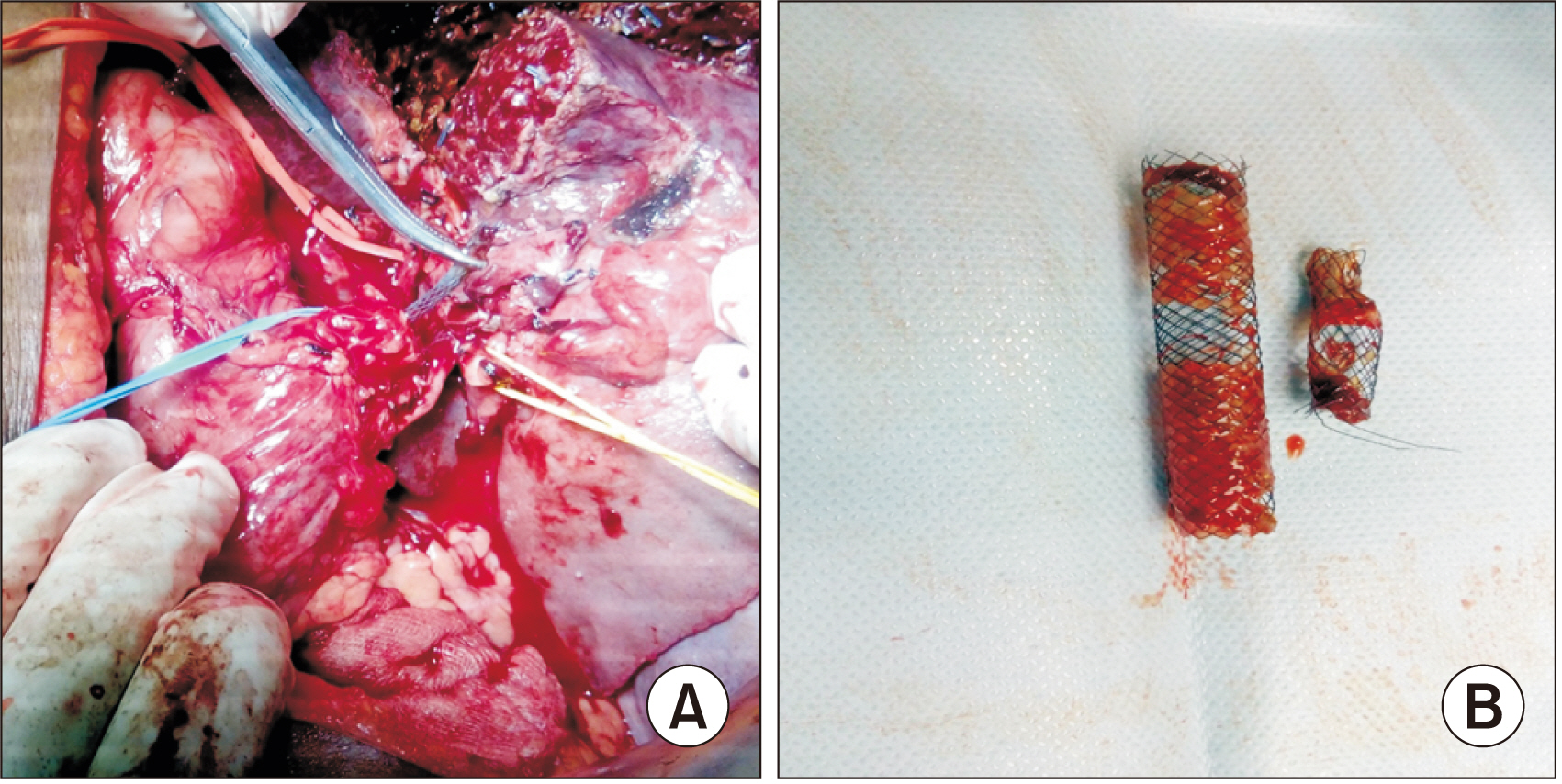
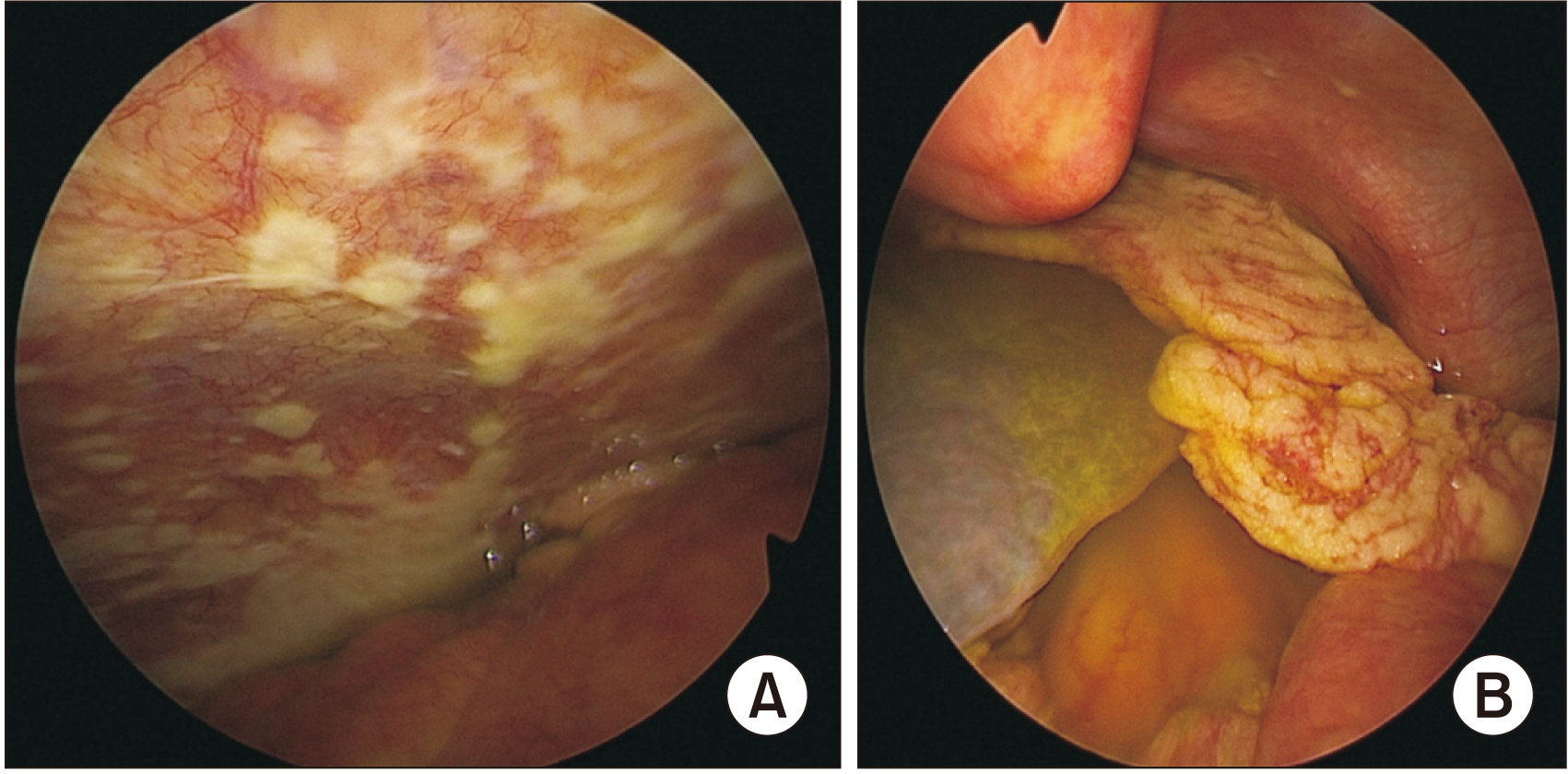
- Hilar cholangiocarcinomas are highly aggressive malignancies. They are usually at an advanced stage at initial presentation. Surgical resection with negative margins is the standard of management. It provides the only chance of cure. Liver transplantation has increased the number of ‘curative’ procedures for cases previously considered to be unresectable. Meticulous and thorough preoperative planning is required to prevent fatal post-operative complications. Extended resection procedures, including hepatic trisectionectomy for Bismuth type IV tumors, hepatopancreaticoduodenectomy for tumors with extensive longitudinal spread, and combined vascular resection with reconstruction for tumors involving hepatic vascular structures, are challenging procedures with surgical indications expanded. Liver transplantation after the standardization of a neoadjuvant protocol described by the Mayo Clinic has increased the number of patients who can undergo operation.
Keyword
Figure
Reference
-
1. de Jong MC, Marques H, Clary BM, Bauer TW, Marsh JW, Ribero D, et al. 2012; The impact of portal vein resection on outcomes for hilar cholangiocarcinoma: a multi-institutional analysis of 305 cases. Cancer. 118:4737–4747. DOI: 10.1002/cncr.27492. PMID: 22415526.2. Altemeier WA, Gall EA, Zinninger MM, Hoxworth PI. 1957; Sclerosing carcinoma of the major intrahepatic bile ducts. AMA Arch Surg. 75:450–460. discussion 460–461. DOI: 10.1001/archsurg.1957.01280150140015. PMID: 13457619.3. Klatskin G. 1965; Adenocarcinoma of the hepatic duct at its bifurcation within the porta hepatis. An unusual tumor with distinctive clinical and pathological features. Am J Med. 38:241–256. DOI: 10.1016/0002-9343(65)90178-6. PMID: 14256720.4. Saxena A, Chua TC, Chu FC, Morris DL. 2011; Improved outcomes after aggressive surgical resection of hilar cholangiocarcinoma: a critical analysis of recurrence and survival. Am J Surg. 202:310–320. DOI: 10.1016/j.amjsurg.2010.08.041. PMID: 21871986.5. Choi JY, Kim MJ, Lee JM, Kim KW, Lee JY, Han JK, et al. 2008; Hilar cholangiocarcinoma: role of preoperative imaging with sonography, MDCT, MRI, and direct cholangiography. AJR Am J Roentgenol. 191:1448–1457. DOI: 10.2214/AJR.07.3992. PMID: 18941084.6. Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BSJ, et al. 2001; Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 234:507–517. discussion 517–519. DOI: 10.1097/00000658-200110000-00010. PMID: 11573044. PMCID: PMC1422074.7. Xiang S, Lau WY, Chen XP. 2015; Hilar cholangiocarcinoma: controversies on the extent of surgical resection aiming at cure. Int J Colorectal Dis. 30:159–171. DOI: 10.1007/s00384-014-2063-z. PMID: 25376337. PMCID: PMC4304009.8. Bismuth H, Nakache R, Diamond T. 1992; Management strategies in resection for hilar cholangiocarcinoma. Ann Surg. 215:31–38. DOI: 10.1097/00000658-199201000-00005. PMID: 1309988. PMCID: PMC1242367.9. Blechacz BR, Sanchez W, Gores GJ. 2009; A conceptual proposal for staging ductal cholangiocarcinoma. Curr Opin Gastroenterol. 25:238–239. DOI: 10.1097/MOG.0b013e3283292383. PMID: 19387257. PMCID: PMC2898128.10. Deoliveira ML, Schulick RD, Nimura Y, Rosen C, Gores G, Neuhaus P, et al. 2011; New staging system and a registry for perihilar cholangiocarcinoma. Hepatology. 53:1363–1371. DOI: 10.1002/hep.24227. PMID: 21480336.11. Gaspersz MP, Buettner S, van Vugt JLA, de Jonge J, Polak WG, Doukas M, et al. 2020; Evaluation of the New American Joint Committee on Cancer staging manual 8th edition for perihilar cholangiocarcinoma. J Gastrointest Surg. 24:1612–1618. DOI: 10.1007/s11605-019-04127-x. PMID: 30756314. PMCID: PMC7359130.12. Fausto N, Campbell JS, Riehle KJ. 2006; Liver regeneration. Hepatology. 43(2 Suppl 1):S45–S53. DOI: 10.1002/hep.20969. PMID: 16447274. PMCID: PMC10368377.13. Schweizer W, Duda P, Tanner S, Balsiger D, Höflin F, Blumgart LH, et al. 1995; Experimental atrophy/hypertrophy complex (AHC) of the liver: portal vein, but not bile duct obstruction, is the main driving force for the development of AHC in the rat. J Hepatol. 23:71–78. DOI: 10.1016/0168-8278(95)80313-0. PMID: 8530812.14. May BJ, Madoff DC. 2012; Portal vein embolization: rationale, technique, and current application. Semin Intervent Radiol. 29:81–89. DOI: 10.1055/s-0032-1312568. PMID: 23729977. PMCID: PMC3444878.15. Maundura M, Koea JB. Abdeldayem HM, editor. 2017. Assessment and optimization of the future liver remnant. Updates in liver cancer. IntechOpen;p. 165. DOI: 10.5772/66139.16. Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunvén P, et al. 1990; Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery. 107:521–527. PMID: 2333592.17. Ikeda K, Kinoshita H, Hirohashi K, Kubo S, Kaneda K. 1995; The ultrastructure, kinetics and intralobular distribution of apoptotic hepatocytes after portal branch ligation with special reference to their relationship to necrotic hepatocytes. Arch Histol Cytol. 58:171–184. DOI: 10.1679/aohc.58.171. PMID: 7576869.18. Di Stefano DR, de Baere T, Denys A, Hakime A, Gorin G, Gillet M, et al. 2005; Preoperative percutaneous portal vein embolization: evaluation of adverse events in 188 patients. Radiology. 234:625–630. DOI: 10.1148/radiol.2342031996. PMID: 15591428.19. Kokudo N, Tada K, Seki M, Ohta H, Azekura K, Ueno M, et al. 2001; Proliferative activity of intrahepatic colorectal metastases after preoperative hemihepatic portal vein embolization. Hepatology. 34:267–272. DOI: 10.1053/jhep.2001.26513. PMID: 11481611.20. van Gulik TM, van den Esschert JW, de Graaf W, van Lienden KP, Busch OR, Heger M, et al. 2008; Controversies in the use of portal vein embolization. Dig Surg. 25:436–444. DOI: 10.1159/000184735. PMID: 19212116.21. van Lienden KP, van den Esschert JW, de Graaf W, Bipat S, Lameris JS, van Gulik TM, et al. 2013; Portal vein embolization before liver resection: a systematic review. Cardiovasc Intervent Radiol. 36:25–34. DOI: 10.1007/s00270-012-0440-y. PMID: 22806245. PMCID: PMC3549243.22. Hayashi S, Baba Y, Ueno K, Nakajo M, Kubo F, Ueno S, et al. 2007; Acceleration of primary liver tumor growth rate in embolized hepatic lobe after portal vein embolization. Acta Radiol. 48:721–727. DOI: 10.1080/02841850701424514. PMID: 17729001.23. Nagino M, Ando M, Kamiya J, Uesaka K, Sano T, Nimura Y. 2001; Liver regeneration after major hepatectomy for biliary cancer. Br J Surg. 88:1084–1091. DOI: 10.1046/j.0007-1323.2001.01832.x. PMID: 11488794.24. Kishi Y, Madoff DC, Abdalla EK, Palavecino M, Ribero D, Chun YS, et al. 2008; Is embolization of segment 4 portal veins before extended right hepatectomy justified? Surgery. 144:744–751. DOI: 10.1016/j.surg.2008.05.015. PMID: 19081016. PMCID: PMC5901738.25. van den Esschert JW, de Graaf W, van Lienden KP, Busch OR, Heger M, van Delden OM, et al. 2009; Volumetric and functional recovery of the remnant liver after major liver resection with prior portal vein embolization: recovery after PVE and liver resection. J Gastrointest Surg. 13:1464–1469. DOI: 10.1007/s11605-009-0929-0. PMID: 19475462. PMCID: PMC2710489.26. Schadde E, Ardiles V, Robles-Campos R, Malago M, Machado M, Hernandez-Alejandro R, et al. ALPPS Registry Group. 2014; Early survival and safety of ALPPS: first report of the International ALPPS Registry. Ann Surg. 260:829–836. discussion 836–838. DOI: 10.1097/SLA.0000000000000947. PMID: 25379854.27. Olthof PB, Coelen RJS, Wiggers JK, Groot Koerkamp B, Malago M, Hernandez-Alejandro R, et al. 2017; High mortality after ALPPS for perihilar cholangiocarcinoma: case-control analysis including the first series from the international ALPPS registry. HPB (Oxford). 19:381–387. DOI: 10.1016/j.hpb.2016.10.008. PMID: 28279621. PMCID: PMC5662942.28. Hernandez-Alejandro R, Bertens KA, Pineda-Solis K, Croome KP. 2015; Can we improve the morbidity and mortality associated with the associating liver partition with portal vein ligation for staged hepatectomy (ALPPS) procedure in the management of colorectal liver metastases? Surgery. 157:194–201. DOI: 10.1016/j.surg.2014.08.041. PMID: 25282528.29. Petrowsky H, Györi G, de Oliveira M, Lesurtel M, Clavien PA. 2015; Is partial-ALPPS safer than ALPPS? A single-center experience. Ann Surg. 261:e90–e92. DOI: 10.1097/SLA.0000000000001087. PMID: 25706390.30. Alvarez FA, Ardiles V, Sanchez Claria R, Pekolj J, de Santibañes E. 2013; Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): tips and tricks. J Gastrointest Surg. 17:814–821. DOI: 10.1007/s11605-012-2092-2. PMID: 23188224.31. Gauzolino R, Castagnet M, Blanleuil ML, Richer JP. 2013; The ALPPS technique for bilateral colorectal metastases: three "variations on a theme". Updates Surg. 65:141–148. DOI: 10.1007/s13304-013-0214-3. PMID: 23690242.32. Li J, Kantas A, Ittrich H, Koops A, Achilles EG, Fischer L, et al. 2016; Avoid "all-touch" by hybrid ALPPS to achieve oncological efficacy. Ann Surg. 263:e6–e7. DOI: 10.1097/SLA.0000000000000845. PMID: 25072445.33. Robles R, Parrilla P, López-Conesa A, Brusadin R, de la Peña J, Fuster M, et al. 2014; Tourniquet modification of the associating liver partition and portal ligation for staged hepatectomy procedure. Br J Surg. 101:1129–1134. discussion 1134DOI: 10.1002/bjs.9547. PMID: 24947768.34. Gall TM, Sodergren MH, Frampton AE, Fan R, Spalding DR, Habib NA, et al. 2015; Radio-frequency-assisted liver partition with portal vein ligation (RALPP) for liver regeneration. Ann Surg. 261:e45–e46. DOI: 10.1097/SLA.0000000000000607. PMID: 24670841.35. Gringeri E, Boetto R, D'Amico FE, Bassi D, Cillo U. 2015; Laparoscopic microwave ablation and portal vein ligation for staged hepatectomy (LAPS): a minimally invasive first-step approach. Ann Surg. 261:e42–e43. DOI: 10.1097/SLA.0000000000000606. PMID: 24651131.36. Teng F, Tang YY, Dai JL, Li Y, Chen ZY. 2020; The effect and safety of preoperative biliary drainage in patients with hilar cholangiocarcinoma: an updated meta-analysis. World J Surg Oncol. 18:174. DOI: 10.1186/s12957-020-01904-w. PMID: 32682432. PMCID: PMC7368977.37. Nimura Y, Hayakawa N, Kamiya J, Kondo S, Shionoya S. 1990; Hepatic segmentectomy with caudate lobe resection for bile duct carcinoma of the hepatic hilus. World J Surg. 14:535–543. discussion 544DOI: 10.1007/BF01658686. PMID: 2166381.38. Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunvén P, et al. 1990; Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery. 107:521–527. PMID: 2333592.39. Wiggers JK, Groot Koerkamp B, Cieslak KP, Doussot A, van Klaveren D, Allen PJ, et al. 2016; Postoperative mortality after liver resection for perihilar cholangiocarcinoma: development of a risk score and importance of biliary drainage of the future liver remnant. J Am Coll Surg. 223:321–331.e1. DOI: 10.1016/j.jamcollsurg.2016.03.035. PMID: 27063572. PMCID: PMC4961586.40. Kennedy TJ, Yopp A, Qin Y, Zhao B, Guo P, Liu F, et al. 2009; Role of preoperative biliary drainage of liver remnant prior to extended liver resection for hilar cholangiocarcinoma. HPB (Oxford). 11:445–451. DOI: 10.1111/j.1477-2574.2009.00090.x. PMID: 19768150. PMCID: PMC2742615.41. Wronka KM, Grąt M, Stypułkowski J, Bik E, Patkowski W, Krawczyk M, et al. 2019; Relevance of preoperative hyperbilirubinemia in patients undergoing hepatobiliary resection for hilar cholangiocarcinoma. J Clin Med. 8:458. DOI: 10.3390/jcm8040458. PMID: 30959757. PMCID: PMC6517893.42. Paik WH, Loganathan N, Hwang JH. 2014; Preoperative biliary drainage in hilar cholangiocarcinoma: when and how? World J Gastrointest Endosc. 6:68–73. DOI: 10.4253/wjge.v6.i3.68. PMID: 24634710. PMCID: PMC3952162.43. Hartog H, Ijzermans JN, van Gulik TM, Groot Koerkamp B. 2016; Resection of perihilar cholangiocarcinoma. Surg Clin North Am. 96:247–267. DOI: 10.1016/j.suc.2015.12.008. PMID: 27017863.44. Bird N, Elmasry M, Jones R, Elniel M, Kelly M, Palmer D, et al. 2017; Role of staging laparoscopy in the stratification of patients with perihilar cholangiocarcinoma. Br J Surg. 104:418–425. DOI: 10.1002/bjs.10399. PMID: 27861766.45. Coelen RJ, Ruys AT, Wiggers JK, Nio CY, Verheij J, Gouma DJ, et al. 2016; Development of a risk score to predict detection of metastasized or locally advanced perihilar cholangiocarcinoma at staging laparoscopy. Ann Surg Oncol. 23(Suppl 5):904–910. DOI: 10.1245/s10434-016-5531-6. PMID: 27586005. PMCID: PMC5149561.46. Mantel HT, Westerkamp AC, Sieders E, Peeters PM, de Jong KP, Boer MT, et al. 2016; Intraoperative frozen section analysis of the proximal bile ducts in hilar cholangiocarcinoma is of limited value. Cancer Med. 5:1373–1380. DOI: 10.1002/cam4.693. PMID: 27062713. PMCID: PMC4944862.47. Ribero D, Amisano M, Lo Tesoriere R, Rosso S, Ferrero A, Capussotti L. 2011; Additional resection of an intraoperative margin-positive proximal bile duct improves survival in patients with hilar cholangiocarcinoma. Ann Surg. 254:776–781. discussion 781–83. DOI: 10.1097/SLA.0b013e3182368f85. PMID: 22042470.48. Ke Q, Chen Y, Huang Q, Lin N, Wang L, Liu J. 2020; Does additional resection of a positive microscopic ductal margin benefit patients with perihilar cholangiocarcinoma: a systematic review and meta-analysis. PLoS One. 15:e0232590. DOI: 10.1371/journal.pone.0232590. PMID: 32379819. PMCID: PMC7205232.49. Nooijen LE, Franken LC, de Boer MT, Buttner S, van Dieren S, Koerkamp BG, et al. 2022; Value of routine intraoperative frozen sections of proximal bile duct margins in perihilar cholangiocarcinoma, a retrospective multicenter and matched case-control study. Eur J Surg Oncol. 48:2424–2431. DOI: 10.1016/j.ejso.2022.06.011. PMID: 35729016.50. DeOliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, et al. 2007; Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 245:755–762. DOI: 10.1097/01.sla.0000251366.62632.d3. PMID: 17457168. PMCID: PMC1877058.51. Endo I, House MG, Klimstra DS, Gönen M, D'Angelica M, Dematteo RP, et al. 2008; Clinical significance of intraoperative bile duct margin assessment for hilar cholangiocarcinoma. Ann Surg Oncol. 15:2104–2112. DOI: 10.1245/s10434-008-0003-2. PMID: 18543039.52. Seyama Y, Kubota K, Sano K, Noie T, Takayama T, Kosuge T, et al. 2003; Long-term outcome of extended hemihepatectomy for hilar bile duct cancer with no mortality and high survival rate. Ann Surg. 238:73–83. DOI: 10.1097/01.SLA.0000074960.55004.72. PMID: 12832968. PMCID: PMC1422671.53. Sakamoto E, Nimura Y, Hayakawa N, Kamiya J, Kondo S, Nagino M, et al. 1998; The pattern of infiltration at the proximal border of hilar bile duct carcinoma: a histologic analysis of 62 resected cases. Ann Surg. 227:405–411. DOI: 10.1097/00000658-199803000-00013. PMID: 9527064. PMCID: PMC1191279.54. Launois B, Terblanche J, Lakehal M, Catheline JM, Bardaxoglou E, Landen S, et al. 1999; Proximal bile duct cancer: high resectability rate and 5-year survival. Ann Surg. 230:266–275. DOI: 10.1097/00000658-199908000-00018. PMID: 10450742. PMCID: PMC1420870.55. Otani K, Chijiiwa K, Kai M, Ohuchida J, Nagano M, Kondo K. 2012; Role of hilar resection in the treatment of hilar cholangiocarcinoma. Hepatogastroenterology. 59:696–700. DOI: 10.5754/hge09725. PMID: 22469711.56. Ikeyama T, Nagino M, Oda K, Ebata T, Nishio H, Nimura Y. 2007; Surgical approach to bismuth type I and II hilar cholangiocarcinomas: audit of 54 consecutive cases. Ann Surg. 246:1052–1057. DOI: 10.1097/SLA.0b013e318142d97e. PMID: 18043110.57. Lim JH, Choi GH, Choi SH, Kim KS, Choi JS, Lee WJ. 2013; Liver resection for Bismuth type I and type II hilar cholangiocarcinoma. World J Surg. 37:829–837. DOI: 10.1007/s00268-013-1909-9. PMID: 23354922.58. Hosokawa I, Shimizu H, Yoshidome H, Ohtsuka M, Kato A, Yoshitomi H, et al. 2014; Surgical strategy for hilar cholangiocarcinoma of the left-side predominance: current role of left trisectionectomy. Ann Surg. 259:1178–1185. DOI: 10.1097/SLA.0000000000000584. PMID: 24509210.59. Nagino M, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, et al. 2013; Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann Surg. 258:129–140. DOI: 10.1097/SLA.0b013e3182708b57. PMID: 23059502.60. Jo HS, Kim DS, Yu YD, Kang WH, Yoon KC. 2020; Right-side versus left-side hepatectomy for the treatment of hilar cholangiocarcinoma: a comparative study. World J Surg Oncol. 18:3. DOI: 10.1186/s12957-019-1779-1. PMID: 31901228. PMCID: PMC6942359.61. Bengmark S, Ekberg H, Evander A, Klofver-Stahl B, Tranberg KG. 1988; Major liver resection for hilar cholangiocarcinoma. Ann Surg. 207:120–125. DOI: 10.1097/00000658-198802000-00002. PMID: 2829760. PMCID: PMC1493364.62. Yang M, Li WW, Chen JH, Cui MH, Liu JL. 2021; The value of caudate lobectomy in hilar cholangiocarcinoma treatment: a meta-analysis. Medicine (Baltimore). 100:e24727. DOI: 10.1097/MD.0000000000024727. PMID: 33607815. PMCID: PMC7899860.63. Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, Nimura Y, et al. 2012; Hepatopancreatoduodenectomy for cholangiocarcinoma: a single-center review of 85 consecutive patients. Ann Surg. 256:297–305. DOI: 10.1097/SLA.0b013e31826029ca. PMID: 22750757.64. Neuhaus P, Thelen A, Jonas S, Puhl G, Denecke T, Veltzke-Schlieker W, et al. 2012; Oncological superiority of hilar en bloc resection for the treatment of hilar cholangiocarcinoma. Ann Surg Oncol. 19:1602–1608. DOI: 10.1245/s10434-011-2077-5. PMID: 21964888.65. Wu XS, Dong P, Gu J, Li ML, Wu WG, Lu JH, et al. 2013; Combined portal vein resection for hilar cholangiocarcinoma: a meta-analysis of comparative studies. J Gastrointest Surg. 17:1107–1115. DOI: 10.1007/s11605-013-2202-9. PMID: 23592188.66. Anderson B, Doyle MBM. 2019; Surgical considerations of hilar cholangiocarcinoma. Surg Oncol Clin N Am. 28:601–617. DOI: 10.1016/j.soc.2019.06.003. PMID: 31472908.67. Nagino M, Nimura Y, Nishio H, Ebata T, Igami T, Matsushita M, et al. 2010; Hepatectomy with simultaneous resection of the portal vein and hepatic artery for advanced perihilar cholangiocarcinoma: an audit of 50 consecutive cases. Ann Surg. 252:115–123. DOI: 10.1097/SLA.0b013e3181e463a7. PMID: 20531001.68. Rela M, Rajalingam R, Shanmugam V, O' Sullivan A, Reddy MS, Heaton N. 2014; Novel en-bloc resection of locally advanced hilar cholangiocarcinoma: the Rex recess approach. Hepatobiliary Pancreat Dis Int. 13:93–97. DOI: 10.1016/S1499-3872(14)60013-8. PMID: 24463086.69. Li J, Zhou MH, Ma WJ, Li FY, Deng YL. 2020; Extended lymphadenectomy in hilar cholangiocarcinoma: what it will bring? World J Gastroenterol. 26:3318–3325. DOI: 10.3748/wjg.v26.i24.3318. PMID: 32655260. PMCID: PMC7327786.70. Bagante F, Tran T, Spolverato G, Ruzzenente A, Buttner S, Ethun CG, et al. 2016; Perihilar cholangiocarcinoma: number of nodes examined and optimal lymph node prognostic scheme. J Am Coll Surg. 222:750–759.e2. DOI: 10.1016/j.jamcollsurg.2016.02.012. PMID: 27113512. PMCID: PMC5450030.71. Kitagawa Y, Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H, et al. 2001; Lymph node metastasis from hilar cholangiocarcinoma: audit of 110 patients who underwent regional and paraaortic node dissection. Ann Surg. 233:385–392. DOI: 10.1097/00000658-200103000-00013. PMID: 11224627. PMCID: PMC1421255.72. Aoba T, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, et al. 2013; Assessment of nodal status for perihilar cholangiocarcinoma: location, number, or ratio of involved nodes. Ann Surg. 257:718–725. DOI: 10.1097/SLA.0b013e3182822277. PMID: 23407295.73. Mantel HT, Wiggers JK, Verheij J, Doff JJ, Sieders E, van Gulik TM, et al. 2015; Lymph node micrometastases are associated with worse survival in patients with otherwise node-negative hilar cholangiocarcinoma. Ann Surg Oncol. 22 Suppl 3:S1107–S1115. DOI: 10.1245/s10434-015-4723-9. PMID: 26178761. PMCID: PMC4686550.74. Fretland ÅA, Dagenborg VJ, Bjørnelv GMW, Kazaryan AM, Kristiansen R, Fagerland MW, et al. 2018; Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg. 267:199–207. DOI: 10.1097/SLA.0000000000002353. PMID: 28657937.75. Yu H, Wu SD, Chen DX, Zhu G. 2011; Laparoscopic resection of Bismuth type I and II hilar cholangiocarcinoma: an audit of 14 cases from two institutions. Dig Surg. 28:44–49. DOI: 10.1159/000322398. PMID: 21293131.76. Gumbs AA, Jarufe N, Gayet B. 2013; Minimally invasive approaches to extrapancreatic cholangiocarcinoma. Surg Endosc. 27:406–414. DOI: 10.1007/s00464-012-2489-8. PMID: 22926892.77. Zhang Y, Dou C, Wu W, Liu J, Jin L, Hu Z, et al. 2020; Total laparoscopic versus open radical resection for hilar cholangiocarcinoma. Surg Endosc. 34:4382–4387. DOI: 10.1007/s00464-019-07211-0. PMID: 31664578.78. Ratti F, Fiorentini G, Cipriani F, Catena M, Paganelli M, Aldrighetti L. 2020; Perihilar cholangiocarcinoma: are we ready to step towards minimally invasiveness? Updates Surg. 72:423–433. DOI: 10.1007/s13304-020-00752-3. PMID: 32221907.79. He YG, Huang W, Ren Q, Li J, Yang FX, Deng CL, et al. 2022; Comparison of efficacy and safety between laparoscopic and open radical resection for hilar cholangiocarcinoma-a propensity score-matching analysis. Front Oncol. 12:1004974. DOI: 10.3389/fonc.2022.1004974. PMID: 36226051. PMCID: PMC9549331.80. Xu Y, Wang H, Ji W, Tang M, Li H, Leng J, et al. 2016; Robotic radical resection for hilar cholangiocarcinoma: perioperative and long-term outcomes of an initial series. Surg Endosc. 30:3060–3070. DOI: 10.1007/s00464-016-4925-7. PMID: 27194255.81. Jacoby H, Rayman S, Ross S, Crespo K, Syblis C, Rosemurgy A, et al. 2022; Robotic resection of hilar cholangiocarcinoma: a single institution experience. Mini-invasive Surg. 6:58. DOI: 10.20517/2574-1225.2022.58.82. Mansour JC, Aloia TA, Crane CH, Heimbach JK, Nagino M, Vauthey JN. 2015; Hilar cholangiocarcinoma: expert consensus statement. HPB (Oxford). 17:691–699. DOI: 10.1111/hpb.12450. PMID: 26172136. PMCID: PMC4527854.83. Iwatsuki S, Todo S, Marsh JW, Madariaga JR, Lee RG, Dvorchik I, et al. 1998; Treatment of hilar cholangiocarcinoma (Klatskin tumors) with hepatic resection or transplantation. J Am Coll Surg. 187:358–364. DOI: 10.1016/S1072-7515(98)00207-5. PMID: 9783781. PMCID: PMC2991118.84. De Vreede I, Steers JL, Burch PA, Rosen CB, Gunderson LL, Haddock MG, et al. 2000; Prolonged disease-free survival after orthotopic liver transplantation plus adjuvant chemoirradiation for cholangiocarcinoma. Liver Transpl. 6:309–316. DOI: 10.1053/lv.2000.6143. PMID: 10827231.85. Rea DJ, Heimbach JK, Rosen CB, Haddock MG, Alberts SR, Kremers WK, et al. 2005; Liver transplantation with neoadjuvant chemoradiation is more effective than resection for hilar cholangiocarcinoma. Ann Surg. 242:451–458. discussion 458–461. DOI: 10.1097/01.sla.0000179678.13285.fa. PMID: 16135931. PMCID: PMC1357753.86. Gores GJ, Gish RG, Sudan D, Rosen CB. MELD Exception Study Group. 2006; Model for end-stage liver disease (MELD) exception for cholangiocarcinoma or biliary dysplasia. Liver Transpl. 12(12 Suppl 3):S95–S97. DOI: 10.1002/lt.20965. PMID: 17123289.87. Zaydfudim VM, Rosen CB, Nagorney DM. 2014; Hilar cholangiocarcinoma. Surg Oncol Clin N Am. 23:247–263. DOI: 10.1016/j.soc.2013.10.005. PMID: 24560109.88. Ethun CG, Lopez-Aguiar AG, Anderson DJ, Adams AB, Fields RC, Doyle MB, et al. 2018; Transplantation versus resection for hilar cholangiocarcinoma: an argument for shifting treatment paradigms for resectable disease. Ann Surg. 267:797–805. DOI: 10.1097/SLA.0000000000002574. PMID: 29064885. PMCID: PMC6002861.89. Cambridge WA, Fairfield C, Powell JJ, Harrison EM, Søreide K, Wigmore SJ, et al. 2021; Meta-analysis and meta-regression of survival after liver transplantation for unresectable perihilar cholangiocarcinoma. Ann Surg. 273:240–250. DOI: 10.1097/SLA.0000000000003801. PMID: 32097164.90. Croome KP, Rosen CB, Heimbach JK, Nagorney DM. 2015; Is liver transplantation appropriate for patients with potentially resectable de novo hilar cholangiocarcinoma? J Am Coll Surg. 221:130–139. DOI: 10.1016/j.jamcollsurg.2015.01.064. PMID: 25872685.91. Gores GJ, Gish RG, Sudan D, Rosen CB. MELD Exception Study Group. 2006; Model for end-stage liver disease (MELD) exception for cholangiocarcinoma or biliary dysplasia. Liver Transpl. 12(12 Suppl 3):S95–S97. DOI: 10.1002/lt.20965. PMID: 17123289.92. Umgelter A, Hapfelmeier A, Kopp W, van Rosmalen M, Rogiers X, Guba M. Eurotransplant Liver Advisory Committee. 2017; Disparities in Eurotransplant liver transplantation wait-list outcome between patients with and without model for end-stage liver disease exceptions. Liver Transpl. 23:1256–1265. DOI: 10.1002/lt.24805. PMID: 28650098.93. Lang SA, Bednarsch J, Czigany Z, Joechle K, Kroh A, Amygdalos I, et al. 2021; Liver transplantation in malignant disease. World J Clin Oncol. 12:623–645. DOI: 10.5306/wjco.v12.i8.623. PMID: 34513597. PMCID: PMC8394155.94. Soares KC, Jarnagin WR. 2021; The landmark series: hilar cholangiocarcinoma. Ann Surg Oncol. 28:4158–4170. DOI: 10.1245/s10434-021-09871-6. PMID: 33829358. PMCID: PMC9273057.95. Kim KB, Choi DW, Heo JS, Han IW, Shin SH, You Y, et al. 2021; The impact of portal vein resection on outcome of hilar cholangiocarcinoma. Ann Hepatobiliary Pancreat Surg. 25:221–229. DOI: 10.14701/ahbps.2021.25.2.221. PMID: 34053925. PMCID: PMC8180392.96. Rebelo A, Friedrichs J, Grilli M, Wahbeh N, Partsakhashvili J, Ukkat J, et al. 2022; Systematic review and meta-analysis of surgery for hilar cholangiocarcinoma with arterial resection. HPB (Oxford). 24:1600–1614. DOI: 10.1016/j.hpb.2022.04.002. PMID: 35490097.97. Fancellu A, Sanna V, Deiana G, Ninniri C, Turilli D, Perra T, et al. 2021; Current role of hepatopancreatoduodenectomy for the management of gallbladder cancer and extrahepatic cholangiocarcinoma: a systematic review. World J Gastrointest Oncol. 13:625–637. DOI: 10.4251/wjgo.v13.i6.625. PMID: 34163578. PMCID: PMC8204357.98. Dopazo C, Charco R. 2023; Liver transplantation for perihilar cholangiocarcinoma. Do we need to move forward? Hepatoma Res. 9:10. DOI: 10.20517/2394-5079.2022.75.