J Cerebrovasc Endovasc Neurosurg.
2012 Dec;14(4):309-314. 10.7461/jcen.2012.14.4.309.
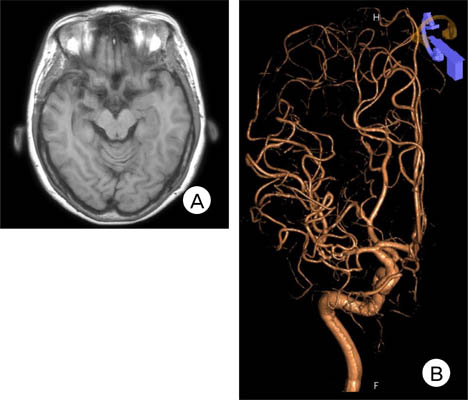
Spontaneous Complete Occlusion of Middle Cerebral Artery Aneurysm: Case Report
- Affiliations
-
- 1Department of Neurosurgery, Busan Paik Hospital, Inje university College of Medicine, Busan, Korea.
- 2Department of Neurosurgery, Haeundae Paik Hopspital, Inje university College of Medicine, Busan, Korea. nssunlee@inje.ac.kr
- KMID: 1431286
- DOI: http://doi.org/10.7461/jcen.2012.14.4.309
Abstract
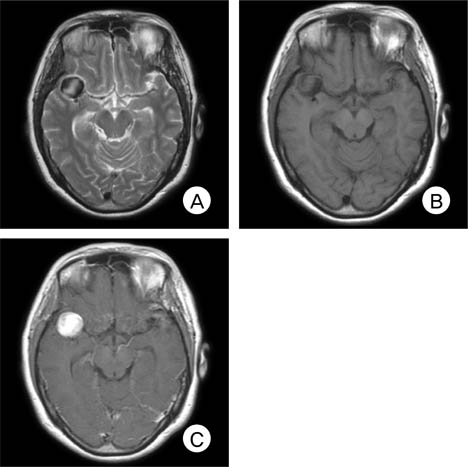
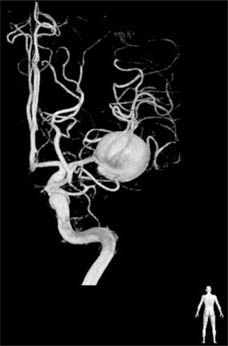
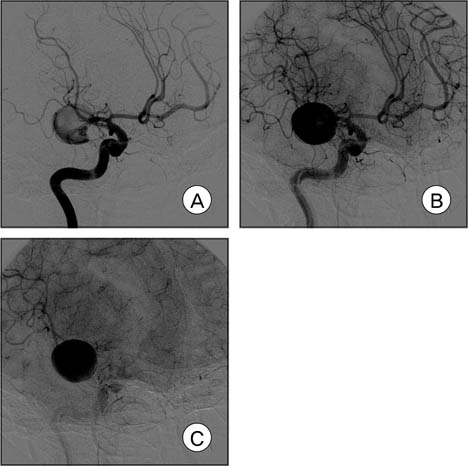
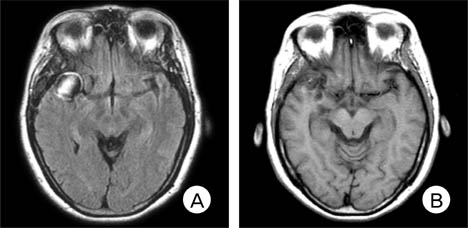
- There are few observation papers regarding the natural history of an aneurysm. We report on a case of a completely occluded middle cerebral artery (MCA) aneurysm. A 47-year-old female patient presented with a headache and was diagnosed with rupture of a right MCA aneurysm. Due to a high risk of direct neck clipping, she received conservative treatment after craniotomy and wrapping of her aneurysm. The patient's condition showed improvement, with complete occlusion of the aneurysm and considerable reduction of the aneurysm in size after approximately three years. This is a rare case of an aneurysm of MCA that showed spontaneous resolution. Finally, on the angiogram, characteristics of an aneurysm to occlude spontaneously will be presumed based on literature reviews.
MeSH Terms
Figure
Cited by 1 articles
-
Thrombosis and Recanalization of Small Saccular Cerebral Aneurysm : Two Case Reports and a Suggestion for Possible Mechanism
Hyung Jun Kim, Jae Hoon Kim, Duk Ryung Kim, Hee In Kang
J Korean Neurosurg Soc. 2014;55(5):280-283. doi: 10.3340/jkns.2014.55.5.280.
Reference
-
1. International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms-risk of rupture and risks of surgical intervention. N Engl J Med. 1998. 12. 339(24):1725–1733.2. De Lange SA. [A case of spontaneous thrombosis of a cerebral arteriovenous aneurysm]. Ned Tijdschr Geneeskd. 1955. 03. 99(13):944–946. Dutch.3. Vasconcellos LP, Flores JAC, Conti MLM, Veiga JCE, Lancellotti CLP. Spontaneous thrombosis of internal carotid artery: a natural history of giant carotid cavernous aneurysms. Arq Neuropsiquiatr. 2009. 06. 67(2A):278–283.
Article4. Deshmukh VR, Kakarla UK, Figueiredo EG, Zabramski JM, Spetzler RF. Long-term clinical and angiographic follow-up of unclippable wrapped intracranial aneurysms. Neurosurgery. 2006. 03. 58(3):434–442. discussion 434-42.
Article5. Fujiwara S, Fujii K, Nishio S, Fukui M. Long-term results of wrapping of intracranial ruptured aneurysms. Acta Neurochir (Wien). 1990. 103(1-2):27–29.6. Gerber S, Dormont D, Sahel M, Grob R, Foncin JF, Marsault C. Complete spontaneous thrombosis of a giant intracranial aneurysm. Neuroradiology. 1994. 05. 36(4):316–317.
Article7. Hay KL, Bull BS. Factors influencing the activation of platelets by nonionic contrast medium. J Vasc Interv Radiol. 1996. May-Jun. 7(3):401–407.
Article8. Heiskanen O. Risks of surgery for unruptured intracranial aneurysms. J Neurosurg. 1986. 10. 65(4):451–453.
Article9. Inagawa T. Surgical treatment of multiple intracranial aneurysms. Acta Neurochir (Wien). 1991. 108(1-2):22–29.
Article10. King JT Jr, Berlin JA, Flamm ES. Morbidity and mortality from elective surgery for asymptomatic, unruptured, intracranial aneurysms: a meta-analysis. J Neurosurg. 1994. 12. 81(6):837–842.
Article11. Krapf H, Schoning M, Petersen D, Kuker W. Complete asymptomatic thrombosis and resorption of a congenital giant intracranial aneurysm. J Neurosurg. 2002. 07. 97(1):184–189.
Article12. Loevner LA, Ting TY, Hurst RW, Goldberg HI, Schut L. Spontaneous thrombosis of a basilar artery traumatic aneurysm in a child. AJNR Am J Neuroradiol. 1998. 02. 19(2):386–388.13. Maruyama M, Asai T, Kuriyama Y, Sawada T, Ogata J, Nishimura T, et al. Positive platelet scintigram of a vertebral aneurysm presenting thromboembolic transient ischemic attacks. Stroke. 1989. 05. 20(5):687–690.
Article14. Moron F, Benndorf G, Akpek S, Dempsy R, Strother CM. Spontaneous thrombosis of a traumatic posterior cerebral artery aneurysm in a child. AJNR Am J Neuroradiol. 2005. 01. 26(1):58–60.15. Nakstad P. Spontaneous occlusion of traumatic pericallosal aneurysm and pericallosal artery. Neuroradiology. 1987. 29(3):312.
Article16. Sato K, Fujiwara S, Kameyama M, Ogawa A, Yoshimoto T, Suzuki J. Follow-up study on ruptured aneurysms treated by wrapping. Neurol Med Chir (Tokyo). 1990. 30(10):734–737.
Article17. Todd NV, Tocher JL, Jones PA, Miller JD. Outcome following aneurysm wrapping: a 10-year follow-up review of clipped and wrapped aneurysms. J Neurosurg. 1989. 06. 70(6):841–846.
Article18. Wardlaw JM, White PM. The detection and management of unruptured intracranial aneurysms. Brain. 2000. 02. 123(Pt 2):205–221.
Article19. Whittle IR, Dorsch NW, Besser M. Spontaneous thrombosis in giant intracranial aneurysms. J Neurol Neurosurg Psychiatry. 1982. 11. 45(11):1040–1047.
Article20. Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, et al. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003. 07. 362(9378):103–110.
Article21. Yasargil MG, Vise WM, Bader DC. Technical adjuncts in neurosurgery. Surg Neurol. 1977. 8(5):331–336.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Distal Middle Cerebral Artery M4 Aneurysm Surgery Using Navigation-CT Angiography
- Duplication of the Middle Cerebral Artery: Case Report
- Ruptured Distal Lenticulostriate Artery Aneurysm Associated with Ipsilateral Middle Cerebral Artery Occlusion : Case Report
- Spontaneous Dissecting Aneurysm of the Anterior Cerebral Artery: Report of 2 Cases
- Ruptured Dissecting Aneurysm of the Middle Cerebral Artery with Spontaneous Resolution: A Case Report