Korean J Radiol.
2012 Aug;13(4):450-457. 10.3348/kjr.2012.13.4.450.
Assessment of Collagen-Induced Arthritis Using Cyanine 5.5 Conjugated with Hydrophobically Modified Glycol Chitosan Nanoparticles: Correlation with 18F-Fluorodeoxyglucose Positron Emission Tomography Data
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea. shlee@amc.seoul.kr
- 2Korea Institute of Science and Technology, Biomedical Research Center, Seoul 136-791, Korea.
- 3Department of Nuclear Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea.
- 4Department of Radiology, Division of Musculoskeletal Imaging, Stanford University School of Medicine, Stanford, CA 94305, USA.
- KMID: 1383857
- DOI: http://doi.org/10.3348/kjr.2012.13.4.450
Abstract
OBJECTIVE
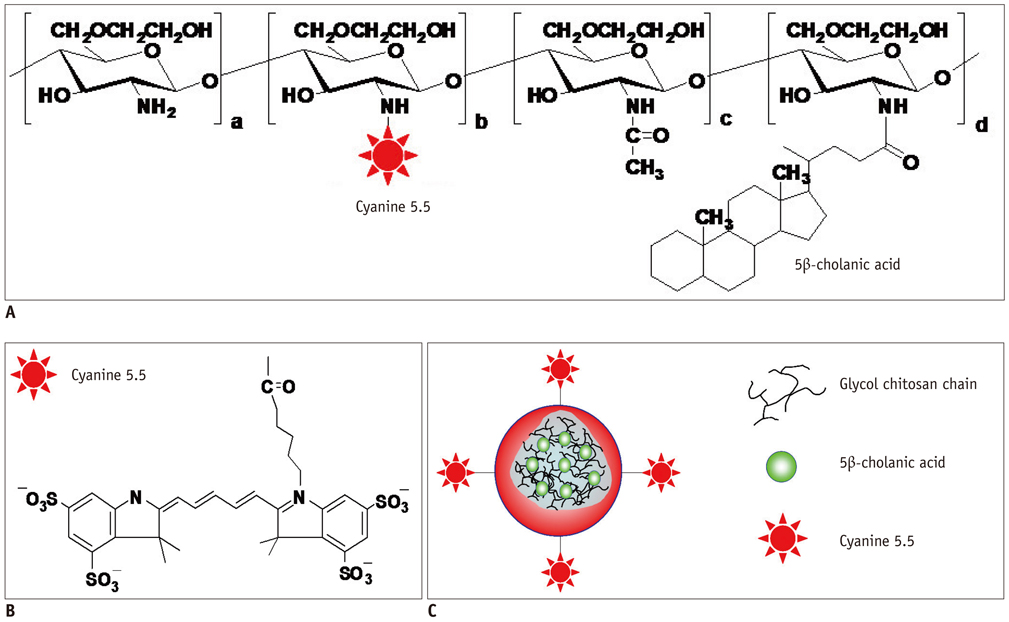
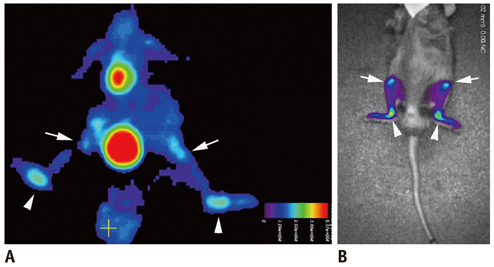
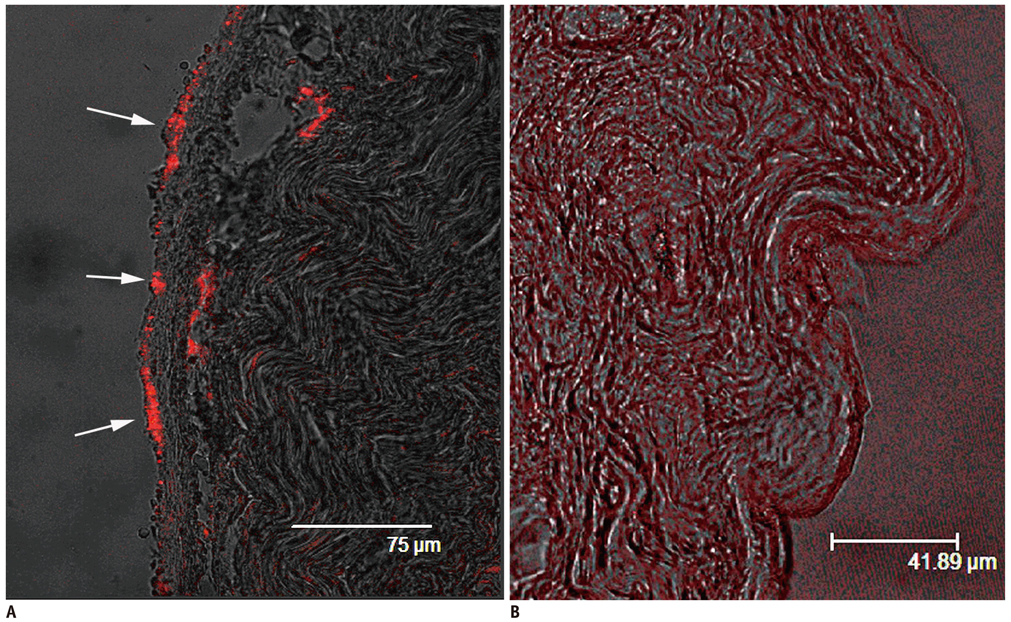
To evaluate the potential and correlation between near-infrared fluorescence (NIRF) imaging using cyanine 5.5 conjugated with hydrophobically modified glycol chitosan nanoparticles (HGC-Cy5.5) and 18F-fluorodeoxyglucose-positron emission tomography (18F-FDG-PET) imaging of collagen-induced arthritis (CIA).
MATERIALS AND METHODS
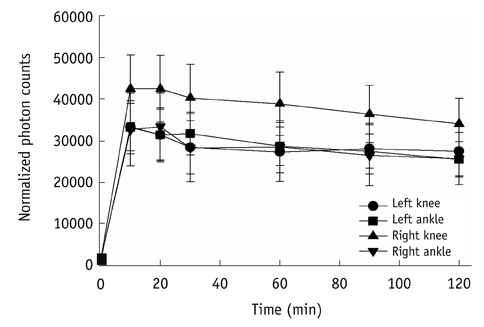
We used 10 CIA and 3 normal mice. Nine days after the injecting collagen twice, microPET imaging was performed 40 minutes after the intravenous injection of 9.3 MBq 18F-FDG in 200 microL PBS. One day later, NIRF imaging was performed two hours after the intravenous injection of HGC-cy5.5 (5 mg/kg). We assessed the correlation between these two modalities in the knees and ankles of CIA mice.
RESULTS
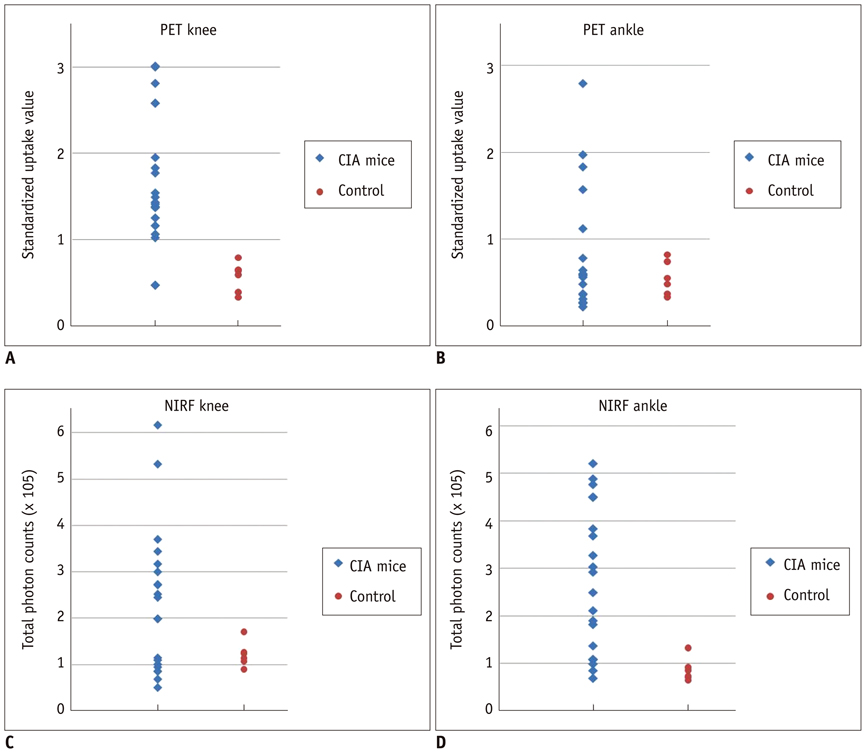
The mean standardized uptake values of 18F-FDG for knees and ankles were 1.68 +/- 0.76 and 0.79 +/- 0.71, respectively, for CIA mice; and 0.57 +/- 0.17 and 0.54 +/- 0.20 respectively for control mice. From the NIRF images, the total photon counts per 30 mm2 for knees and ankles were 2.32 +/- 1.54 x 10(5) and 2.75 +/- 1.51 x 10(5), respectively, for CIA mice, and 1.22 +/- 0.27 x 10(5) and 0.88 +/- 0.24 x 10(5), respectively, for control mice. These two modalities showed a moderate correlation for knees (r = 0.604, p = 0.005) and ankles (r = 0.464, p = 0.039). Moreover, both HGC-Cy5.5 (p = 0.002) and 18F-FDG-PET (p = 0.005) imaging also showed statistically significant differences between CIA and normal mice.
CONCLUSION
NIRF imaging using HGC-Cy5.5 was moderately correlated with 18F-FDG-PET imaging in the CIA model. As such, HGC-Cy5.5 imaging can be used for the early detection of rheumatoid arthritis.
MeSH Terms
-
Animals
Ankle Joint/radionuclide imaging
Arthritis, Experimental/*radionuclide imaging
Carbocyanines/administration & dosage/*diagnostic use
Chitosan/administration & dosage/*diagnostic use
Fluorodeoxyglucose F18/administration & dosage/diagnostic use
Injections, Intravenous
Knee Joint/radionuclide imaging
Male
Mice
Microscopy, Confocal
Nanoparticles
Positron-Emission Tomography/*methods
Radiopharmaceuticals/administration & dosage/diagnostic use
Statistics, Nonparametric
Figure
Reference
-
1. Sommer OJ, Kladosek A, Weiler V, Czembirek H, Boeck M, Stiskal M. Rheumatoid arthritis: a practical guide to state-of-the-art imaging, image interpretation, and clinical implications. Radiographics. 2005. 25:381–398.2. Wunder A, Straub RH, Gay S, Funk J, Müller-Ladner U. Molecular imaging: novel tools in visualizing rheumatoid arthritis. Rheumatology (Oxford). 2005. 44:1341–1349.3. Holmdahl R, Andersson ME, Goldschmidt TJ, Jansson L, Karlsson M, Malmström V, et al. Collagen induced arthritis as an experimental model for rheumatoid arthritis. Immunogenetics, pathogenesis and autoimmunity. APMIS. 1989. 97:575–584.4. Williams RO. Collagen-induced arthritis as a model for rheumatoid arthritis. Methods Mol Med. 2004. 98:207–216.5. Elzinga EH, van der Laken CJ, Comans EF, Lammertsma AA, Dijkmans BA, Voskuyl AE. 2-Deoxy-2-[F-18]fluoro-D-glucose joint uptake on positron emission tomography images: rheumatoid arthritis versus osteoarthritis. Mol Imaging Biol. 2007. 9:357–360.6. Beckers C, Ribbens C, André B, Marcelis S, Kaye O, Mathy L, et al. Assessment of disease activity in rheumatoid arthritis with (18)F-FDG PET. J Nucl Med. 2004. 45:956–964.7. Brenner W. 18F-FDG PET in rheumatoid arthritis: there still is a long way to go. J Nucl Med. 2004. 45:927–929.8. Hansch A, Frey O, Hilger I, Sauner D, Haas M, Schmidt D, et al. Diagnosis of arthritis using near-infrared fluorochrome Cy5.5. Invest Radiol. 2004. 39:626–632.9. Fischer T, Gemeinhardt I, Wagner S, Stieglitz DV, Schnorr J, Hermann KG, et al. Assessment of unspecific near-infrared dyes in laser-induced fluorescence imaging of experimental arthritis. Acad Radiol. 2006. 13:4–13.10. Chen WT, Mahmood U, Weissleder R, Tung CH. Arthritis imaging using a near-infrared fluorescence folate-targeted probe. Arthritis Res Ther. 2005. 7:R310–R317.11. Kaş HS. Chitosan: properties, preparations and application to microparticulate systems. J Microencapsul. 1997. 14:689–711.12. Hansch A, Frey O, Sauner D, Hilger I, Haas M, Malich A, et al. In vivo imaging of experimental arthritis with near-infrared fluorescence. Arthritis Rheum. 2004. 50:961–967.13. Sugimoto K, Nishimoto N, Kishimoto T, Yoshizaki K, Nishimura T. Imaging of lesions in a murine rheumatoid arthritis model with a humanized anti-interleukin-6 receptor antibody. Ann Nucl Med. 2005. 19:261–266.14. Frost H. Antibody-mediated side effects of recombinant proteins. Toxicology. 2005. 209:155–160.15. Licha K, Hessenius C, Becker A, Henklein P, Bauer M, Wisniewski S, et al. Synthesis, characterization, and biological properties of cyanine-labeled somatostatin analogues as receptor-targeted fluorescent probes. Bioconjug Chem. 2001. 12:44–50.16. Weissleder R. A clearer vision for in vivo imaging. Nat Biotechnol. 2001. 19:316–317.17. Kim JH, Kim YS, Park K, Kang E, Lee S, Nam HY, et al. Self-assembled glycol chitosan nanoparticles for the sustained and prolonged delivery of antiangiogenic small peptide drugs in cancer therapy. Biomaterials. 2008. 29:1920–1930.18. Park K, Kim JH, Nam YS, Lee S, Nam HY, Kim K, et al. Effect of polymer molecular weight on the tumor targeting characteristics of self-assembled glycol chitosan nanoparticles. J Control Release. 2007. 122:305–314.19. Caesar J, Shaldon S, Chiandussi L, Guevara L, Sherlock S. The use of indocyanine green in the measurement of hepatic blood flow and as a test of hepatic function. Clin Sci. 1961. 21:43–57.20. Brancato R, Trabucchi G. Fluorescein and indocyanine green angiography in vascular chorioretinal diseases. Semin Ophthalmol. 1998. 13:189–198.21. Licha K, Riefke B, Ntziachristos V, Becker A, Chance B, Semmler W. Hydrophilic cyanine dyes as contrast agents for near-infrared tumor imaging: synthesis, photophysical properties and spectroscopic in vivo characterization. Photochem Photobiol. 2000. 72:392–398.22. Storm G, Roerdink FH, Steerenberg PA, de Jong WH, Crommelin DJ. Influence of lipid composition on the antitumor activity exerted by doxorubicin-containing liposomes in a rat solid tumor model. Cancer Res. 1987. 47:3366–3372.23. Takeuchi H, Kojima H, Toyoda T, Yamamoto H, Hino T, Kawashima Y. Prolonged circulation time of doxorubicin-loaded liposomes coated with a modified polyvinyl alcohol after intravenous injection in rats. Eur J Pharm Biopharm. 1999. 48:123–129.24. Hwang HY, Kim IS, Kwon IC, Kim YH. Tumor targetability and antitumor effect of docetaxel-loaded hydrophobically modified glycol chitosan nanoparticles. J Control Release. 2008. 128:23–31.25. Weissleder R, Ntziachristos V. Shedding light onto live molecular targets. Nat Med. 2003. 9:123–128.26. Goerres GW, Forster A, Uebelhart D, Seifert B, Treyer V, Michel B, et al. F-18 FDG whole-body PET for the assessment of disease activity in patients with rheumatoid arthritis. Clin Nucl Med. 2006. 31:386–390.27. Palmer WE, Rosenthal DI, Schoenberg OI, Fischman AJ, Simon LS, Rubin RH, et al. Quantification of inflammation in the wrist with gadolinium-enhanced MR imaging and PET with 2-[F-18]-fluoro-2-deoxy-D-glucose. Radiology. 1995. 196:647–655.28. Bresnihan B. Pathogenesis of joint damage in rheumatoid arthritis. J Rheumatol. 1999. 26:717–719.29. Andersson SE, Johansson A, Lexmüller K, Ekström GM. Physiological characterization of mBSA antigen induced arthritis in the rat. II. Joint blood flow, glucose metabolism, and cell proliferation. J Rheumatol. 1998. 25:1778–1784.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Verification of the Dystonic Muscles Using 18F-Fluorodeoxyglucose Positron Emission Tomography in a Patient with Cervical Dystonia: A case report
- Supraclavicular Lymph Node Metastasis from Various Malignancies: Assessment with 18F-Fluorodeoxyglucose Positron Emission Tomography/CT, Contrast-Enhanced CT and Ultrasound
- The importance of 18F-fluorodeoxyglucose positron emission tomography and carbohydrate antigen 19-9 in patients with periampullary tumors
- Lymphocytic Thyroiditis Presenting as a Focal Uptake on 18F-Fluorodeoxyglucose Positron Emission Tomography: A Case Report
- Perirenal 18F-FDG Uptake in a Patient with a Pheochromocytoma