Korean J Radiol.
2012 Apr;13(2):244-248. 10.3348/kjr.2012.13.2.244.
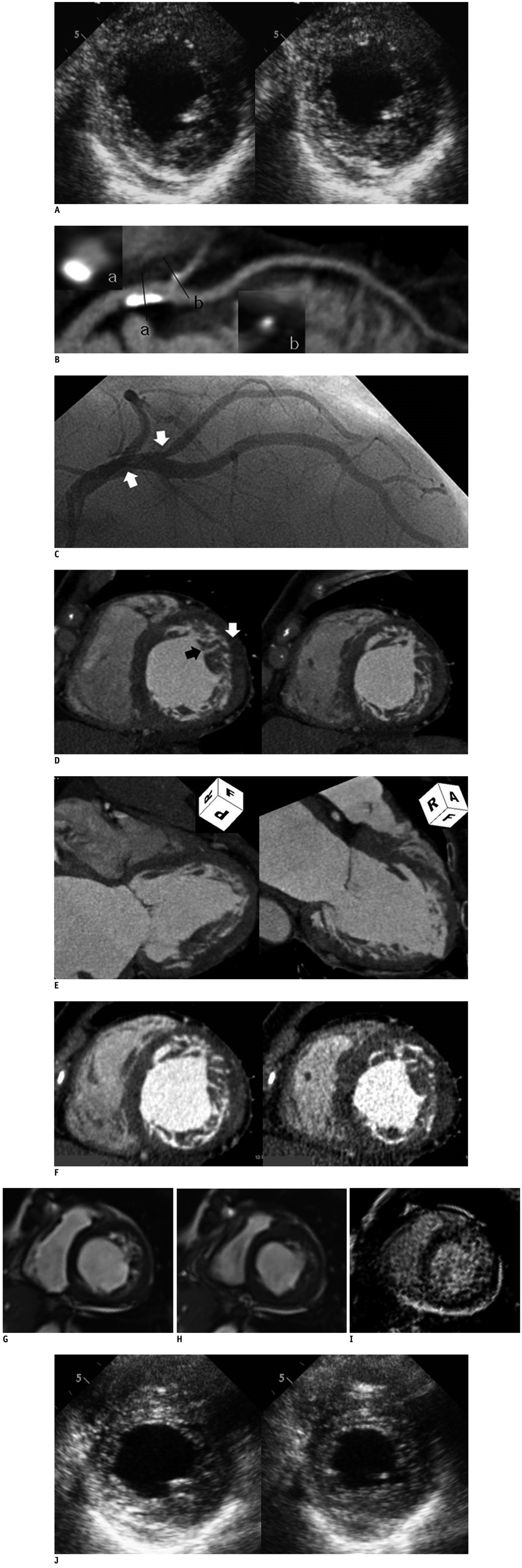
Isolated Non-Compaction of the Left Ventricle in a Patient with New-Onset Heart Failure: Morphologic and Functional Evaluation with Cardiac Multidetector Computed Tomography
- Affiliations
-
- 1Department of Radiology, Soonchuhyang University Bucheon Hospital, Bucheon 420-767, Korea.
- 2Department of Cardiology, Seoul Medical Center, Seoul 138-160, Korea.
- 3Department of Radiology and Radiological Science and Division of Cardiology, Department of Medicine, Medical University of South Carolina, SC 29401, USA. schoepf@musc.edu
- KMID: 1245391
- DOI: http://doi.org/10.3348/kjr.2012.13.2.244
Abstract
- We describe a case of new-onset heart failure in a patient in whom cardiac CT enabled the non-invasive diagnosis of isolated non-compaction and associated functional abnormalities of the left ventricle with the concomitant evaluation of coronary arteries. This case highlights the utility of cardiac CT for the morphological and functional evaluation of the heart as a single imaging modality.
MeSH Terms
-
Aged
Cardiac-Gated Imaging Techniques
Contrast Media/diagnostic use
Diagnosis, Differential
Disease Progression
Echocardiography
Electrocardiography
Heart Failure/*diagnosis
Humans
Image Interpretation, Computer-Assisted
Iohexol/analogs & derivatives/diagnostic use
Isolated Noncompaction of the Ventricular Myocardium/*diagnosis
Magnetic Resonance Imaging
Male
*Tomography, X-Ray Computed
Figure
Reference
-
1. Dusek J, Ostádal B, Duskova M. Postnatal persistence of spongy myocardium with embryonic blood supply. Arch Pathol. 1975. 99:312–317.2. Zenooz NA, Zahka KG, Siwik ES, Gilkeson RC. Noncompaction syndrome of the myocardium: pathophysiology and imaging pearls. J Thorac Imaging. 2010. 25:326–332.3. Bladt O, Vanhoenacker R, Bevernage C, Leyman P. Isolated noncompaction of ventricular myocardium. Diagnosis with multidetector computed tomography. JBR-BTR. 2008. 91:153–154.4. Kirsch J, Williamson EE, Araoz PA. Non-compaction visualization using ECG-gated dual-source CT. Int J Cardiol. 2007. 118:e46–e47.5. Hendel RC, Patel MR, Kramer CM, Poon M, Hendel RC, Carr JC, et al. ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol. 2006. 48:1475–1497.6. Moreira FC, Miglioransa MH, Mautone MP, Müller KR, Lucchese F. Noncompaction of the left ventricle: a new cardiomyopathy is presented to the clinician. Sao Paulo Med J. 2006. 124:31–35.7. Murphy RT, Thaman R, Blanes JG, Ward D, Sevdalis E, Papra E, et al. Natural history and familial characteristics of isolated left ventricular non-compaction. Eur Heart J. 2005. 26:187–192.8. Chin TK, Perloff JK, Williams RG, Jue K, Mohrmann R. Isolated noncompaction of left ventricular myocardium. A study of eight cases. Circulation. 1990. 82:507–513.9. Jenni R, Oechslin E, Schneider J, Attenhofer Jost C, Kaufmann PA. Echocardiographic and pathoanatomical characteristics of isolated left ventricular non-compaction: a step towards classification as a distinct cardiomyopathy. Heart. 2001. 86:666–671.10. Lee H, Ruzsics B, Schoepf UJ, Stewart EA, Costello P, Glenn JL, et al. New-onset heart failure caused by spontaneous papillary muscle rupture: diagnosis with dual-source computed tomographic coronary angiography. J Thorac Cardiovasc Surg. 2009. 137:e19–e21.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three-Dimensional Endo-Cardiovascular Volume-Rendered Cine Computed Tomography of Isolated Left Ventricular Apical Hypoplasia: A Case Report and Literature Review
- Noncompaction of Ventricular Myocardium Involving the Right Ventricle
- A Case Report of Congenitally Corrected Transposition of Great Arteries: Morphologic and Functional Evaluation with Cardiac CT
- Left Ventricular Noncompaction Associated with Hypertrophic Cardiomyopathy: Morphologic and Functional Evaluation with Multidetector CT
- Unusual Cardiac Metastasis of Nonvisceral Soft Tissue Leiomyosarcoma in the Right Ventricle:A Case Report and Literature Review