Korean J Gastroenterol.
2012 Mar;59(3):211-217. 10.4166/kjg.2012.59.3.211.
Clinicopathologic Features of Cases with Negative Pathologic Results after Endoscopic Submucosal Dissection
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Guro Hospital, Korea University College of Medicine, Seoul, Korea. gi7pjj@yahoo.co.kr
- 2Department of Pathology, Guro Hospital, Korea University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Kangwon National University Hospital, Kangwon National University College of Medicine, Chuncheon, Korea.
- KMID: 1245205
- DOI: http://doi.org/10.4166/kjg.2012.59.3.211
Abstract
- BACKGROUND/AIMS
Endoscopic submucosal dissection (ESD) is accepted as a standard treatment of early gastric cancer (EGC) and gastric adenoma. Occasionally, tumorous lesion is not found and pathologic discrepancies can occur after ESD. The aim of this study was to analyze the factors affecting the negative pathologic results after ESD.
METHODS
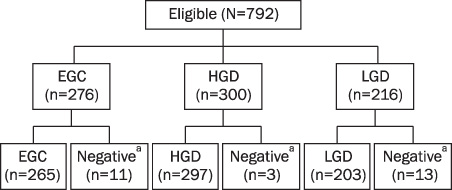
We retrospectively reviewed the data from all patients with gastric neoplasm (276 EGC and 516 gastric adenomas) who were treated with ESD during past 3 years and enrolled the patients who had negative pathologic results.
RESULTS
Out of 792 patients treated with ESD, 27 patients (3.4%) were eligible for inclusion. Among the 27 patients, factors affecting the negative pathologic results were, most commonly, the focal lesion (n=13, 48.2%) which was small enough to be removed completely during pre-ESD biopsy, followed by pathologic discrepancies (n=11, 40.7%) between pathologists and lastly the operator factor (n=3, 11.1%) dissecting incorrect lesions. Of the focal lesions, the initial pathologic diagnoses were adenocarcinoma in 11 cases (84.6%). In cases with pathologic discrepancies, all the pretreatment diagnoses were adenoma with low grade dysplasia. In cases caused by operator factors, intestinal metaplasia was accompanied by elevated adenoma in all cases.
CONCLUSIONS
To decrease negative pathologic results after ESD, an endoscopist should perform ESD after sufficient communication with pathologists, especially for adenoma with low grade dysplasia, and choose correct lesion, especially located at the antrum and associated with intestinal metaplasia. The possibility of total removal of small lesions even by forcep biopsy should be considered.
Keyword
MeSH Terms
Figure
Reference
-
1. Lee HJ, Yang HK, Ahn YO. Gastric cancer in Korea. Gastric Cancer. 2002. 5:177–182.2. Ishikawa S, Togashi A, Inoue M, et al. Indications for EMR/ESD in cases of early gastric cancer: relationship between histological type, depth of wall invasion, and lymph node metastasis. Gastric Cancer. 2007. 10:35–38.3. Gotoda T, Yamamoto H, Soetikno RM. Endoscopic submucosal dissection of early gastric cancer. J Gastroenterol. 2006. 41:929–942.4. Ono H, Kondo H, Gotoda T, et al. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001. 48:225–229.5. Rembacken BJ, Gotoda T, Fujii T, Axon AT. Endoscopic mucosal resection. Endoscopy. 2001. 33:709–718.6. Soetikno RM, Gotoda T, Nakanishi Y, Soehendra N. Endoscopic mucosal resection. Gastrointest Endosc. 2003. 57:567–579.7. Muehldorfer SM, Stolte M, Martus P, Hahn EG, Ell C. Multicenter Study Group "Gastric Polyps". Diagnostic accuracy of forceps biopsy versus polypectomy for gastric polyps: a prospective multicentre study. Gut. 2002. 50:465–470.8. Yoon WJ, Lee DH, Jung YJ, et al. Histologic characteristics of gastric polyps in Korea: emphasis on discrepancy between endoscopic forceps biopsy and endoscopic mucosal resection specimen. World J Gastroenterol. 2006. 12:4029–4032.9. Park EH, Kang KT, Kim BH, et al. The histologic discrepancy before and after endoscopic submucosal dissection of gastric adenoma and early gastric cancer. Korean J Gastrointest Endosc. 2007. 34:125–131.10. Kim ES, Jeon SW, Park SY, et al. Where has the tumor gone? The characteristics of cases of negative pathologic diagnosis after endoscopic mucosal resection. Endoscopy. 2009. 41:739–745.11. Muto M, Miyamoto S, Hosokawa A, et al. Endoscopic mucosal resection in the stomach using the insulated-tip needle-knife. Endoscopy. 2005. 37:178–182.12. Kim JJ, Lee JH, Jung HY, et al. EMR for early gastric cancer in Korea: a multicenter retrospective study. Gastrointest Endosc. 2007. 66:693–700.13. Kim JJ, Kim BJ. Current status of endoscopic mucosal resection for early gastric cancer in Korea. Korean J Med. 2009. 76:291–295.14. Ichiro O, Takuji G, Hisanao H, et al. Endoscopic submucosal dissection for early gastric cancer: technical feasibility, operation time and complications from a large consecutive series. Digestive Endoscopy. 2005. 17:54–58.15. Mannen K, Tsunada S, Hara M, et al. Risk factors for complications of endoscopic submucosal dissection in gastric tumors: analysis of 478 lesions. J Gastroenterol. 2010. 45:30–36.16. Hakim NS, Sarr MG, van Heerden JA. Does endoscopy really help the surgeon evaluate gastric cancer? Can J Surg. 1989. 32:175–177.17. Lee SH, Jung JH, Song JH, et al. Local Recurrence of EGC after ESD. Korean J Gastrointest Endosc. 2011. 42:90–93.18. Sohn YJ, Jang JS, Choi SR, et al. Early detection of recurrence after endoscopic treatment for early gastric cancer. Scand J Gastroenterol. 2009. 44:1109–1114.19. Ichiyoshi Y, Toda T, Minamisono Y, Nagasaki S, Yakeishi Y, Sugimachi K. Recurrence in early gastric cancer. Surgery. 1990. 107:489–495.20. Palli D, Bianchi S, Cipriani F, et al. Reproducibility of histologic classification of gastric cancer. Br J Cancer. 1991. 63:765–768.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- History and Development of Accessories for Endoscopic Submucosal Dissection
- The Clinical Accuracy of Endoscopic Ultrasonography and White Light Imaging in Gastric Endoscopic Submucosal Dissection
- Pathology of Endoscopic Submucosal Dissection; How Do We Interpret?
- Debates on Colorectal Endoscopic Submucosal Dissection - Traction for Effective Dissection: Gravity Is Enough
- A Case of Pneumorrhachis and Pneumoscrotum Following Colon Endoscopic Submucosal Dissection