Yonsei Med J.
2011 Sep;52(5):803-808. 10.3349/ymj.2011.52.5.803.
Results from Over One Year of Follow-Up for Absorbable Mesh Insertion in Partial Mastectomy
- Affiliations
-
- 1Division of Breast and Endocrine Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jeongeon.lee@samsung.com
- KMID: 1108074
- DOI: http://doi.org/10.3349/ymj.2011.52.5.803
Abstract
- PURPOSE
Recently, several clinicians have reported the advantages of simplicity and cosmetic satisfaction of absorbable mesh insertion. However, there is insufficient evidence regardint its long-term outcomes. We have investigated the surgical complications and postoperative examination from the oncologic viewpoint.
MATERIALS AND METHODS
From February 2008 to March 2009, 34 breast cancer patients underwent curative surgery with absorbable mesh insertion in Samsung Medical Center. Patient characteristics and follow up results including complications, clinical and radiological findings were retrospectively investigated.
RESULTS
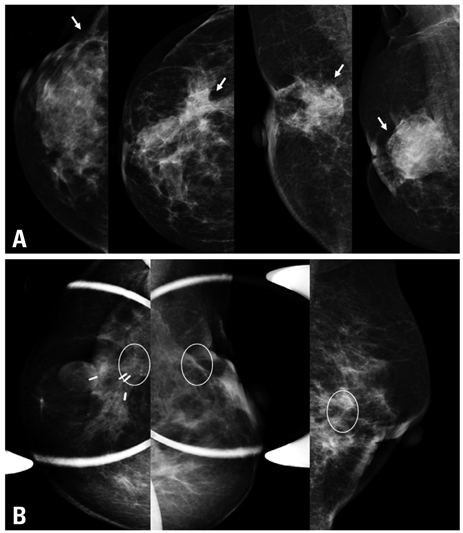
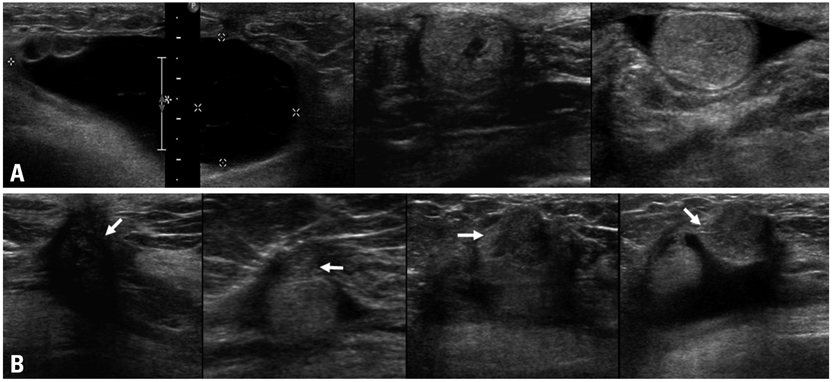
The mean age of the study population was 50.1+/-8.9 years old (range 31-82) with a mean tumor size of 3+/-1.8 cm (range 0.8-10.5), and the excised breast tissue showed a mean volume of 156.1+/-99.8 mL (range 27-550). Over the median follow-up period of 18+/-4.6 months (range 3-25), mesh associated complications, including severe pain or discomfort, edema, and recurrent fluid collection, occurred in nine patients (26.5%). In three cases (8.8%), recurrent mastitis resulted in mesh removal or surgical intervention. In the postoperative radiologic survey, the most common finding was fluid collection, which occurred in five patients (16.1%), including one case with organizing hematoma. Fat necrosis and microcalcifications were found in three patients (9.7%).
CONCLUSION
Absorbable mesh insertion has been established as a technically feasible, time-saving procedure after breast excision. However, the follow-up results showed some noticeable side effects and the oncologic safety of the procedure is unconfirmed. Therefore, we suggest that mesh insertion should be considered only in select cases and should be followed-up carefully.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Edema/etiology
Female
Follow-Up Studies
Granuloma, Foreign-Body/etiology/ultrasonography
Humans
Mammaplasty/adverse effects/methods
Mastectomy, Segmental/adverse effects/*methods
Mastitis/etiology
Middle Aged
Pain/etiology
Postoperative Complications/etiology
Retrospective Studies
*Surgical Mesh/adverse effects
Figure
Cited by 1 articles
-
The Suitability of Absorbable Mesh Insertion for Oncoplastic Breast Surgery in Patients with Breast Cancer Scheduled to Be Irradiated
Taehyun Kim, Heunglae Cho
J Breast Cancer. 2013;16(1):84-89. doi: 10.4048/jbc.2013.16.1.84.
Reference
-
1. Sanuki J, Fukuma E, Wadamori K, Higa K, Sakamoto N, Tsunoda Y. Volume replacement with polyglycolic acid mesh for correcting breast deformity after endoscopic conservative surgery. Clin Breast Cancer. 2005. 6:175.
Article2. Klinge U, Schumpelick V, Klosterhalfen B. Functional assessment and tissue response of short- and long-term absorbable surgical meshes. Biomaterials. 2001. 22:1415–1424.
Article3. Morrow M, Strom EA, Bassett LW, Dershaw DD, Fowble B, Giuliano A, et al. Standard for breast conservation therapy in the management of invasive breast carcinoma. CA Cancer J Clin. 2002. 52:277–300.
Article4. Muss HB, Berry DA, Cirrincione CT, Theodoulou M, Mauer AM, Kornblith AB, et al. Adjuvant chemotherapy in older women with early-stage breast cancer. N Engl J Med. 2009. 360:2055–2065.
Article5. Kim KS, Park MY, Kim WJ, Na KY, Jung YS, Choi YJ, et al. Nationwide Survey of the Use of Absorbable Mesh in Breast Surgery in Korea. J Breast Cancer. 2009. 12:210–214.
Article6. Lee JH, Hong YI, Jeong JH, Lee JI, Lee JH, Moon HJ, et al. Volume replacement with polyglactin 910 mesh for breast reconstruction after endoscopy-assisted breast conserving surgery for treating early breast cancer: the early results. J Breast Cancer. 2009. 12:193–198.
Article7. Eom TI, Kim BS, Koo BY, Kim JW, Lim YA, Lee HH, et al. The Use of a Corrective Procedure with Vicryl Mesh for Oncoplastic Surgery of the Breast. J Breast Cancer. 2009. 12:36–40.
Article8. Kim HO, Hwang SI, Yom CK, Park YL, Bae WG. The use of absorbable surgical mesh after partial mastectomy for improving the cosmetic outcome. J Breast Cancer. 2009. 12:151–155.
Article9. Audretsch W, Rezai M, Kolotas C, Zamboglou N, Schnabel T, Bojar H. Tumor-Specific Immediate Reconstruction in Breast Cancer Patients. Perspect Plast Surg. 1998. 11:71–100.
Article10. Clough KB, Kaufman GJ, Nos C, Buccimazza I, Sarfati IM. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol. 2010. 17:1375–1391.
Article11. Fitoussi AD, Berry MG, Famà F, Falcou MC, Curnier A, Couturaud B, et al. Oncoplastic breast surgery for cancer: analysis of 540 consecutive cases [outcomes article]. Plast Reconstr Surg. 2010. 125:454–462.
Article12. Caruso F, Catanuto G, De Meo L, Ferrara M, Gallodoro A, Petrolito E, et al. Outcomes of bilateral mammoplasty for early stage breast cancer. Eur J Surg Oncol. 2008. 34:1143–1147.
Article13. Rietjens M, Urban CA, Rey PC, Mazzarol G, Maisonneuve P, Garusi C, et al. Long-term oncological results of breast conservative treatment with oncoplastic surgery. Breast. 2007. 16:387–395.
Article14. Cordeiro PG. Breast reconstruction after surgery for breast cancer. N Engl J Med. 2008. 359:1590–1601.
Article15. Kwag HJ. Imaging findings of implanted absorbable mesh in patients with breast partial resection. Yonsei Med J. 2008. 49:111–118.
Article16. Góes JC, Landecker A, Lyra EC, Henríquez LJ, Góes RS, Godoy PM. The application of mesh support in periareolar breast surgery: clinical and mammographic evaluation. Aesthetic Plast Surg. 2004. 28:268–274.
Article17. Góes JC. Periareolar mammaplasty: double skin technique with application of polyglactine or mixed mesh. Plast Reconstr Surg. 1996. 97:959–968.
Article18. Choi Y, Hong HP, Kwag HJ. Ultrasonographic findings of an implanted absorbable mesh in patients with breast partial resection: a preliminary study. J Korean Soc Ultrasound Med. 2007. 26:89–94.19. Harris JR, Lippman ME, Morrow M, Osborne CK. Disease of the breast. 2009. 4th ed. Philadelphia: Wolters Kluwer.20. Symmers W. Systemic pathology. 1978. Edinburgh: Churchill Livingstone.21. Ganau S, Tortajada L, Escribano F, Andreu X, Sentís M. The great mimicker: fat necrosis of the breast--magnetic resonance mammography approach. Curr Probl Diagn Radiol. 2009. 38:189–197.
Article22. Baillie M, Mok PM. Fat necrosis in the breast: review of the mammographic and ultrasound features, and a strategy for management. Australas Radiol. 2004. 48:288–295.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Use of Absorbable Surgical Mesh after Partial Mastectomy for Improving the Cosmetic Outcome
- The Suitability of Absorbable Mesh Insertion for Oncoplastic Breast Surgery in Patients with Breast Cancer Scheduled to Be Irradiated
- Imaging Findings of Implanted Absorbable Mesh in Patients with Breast Partial Resection
- Results of Absorbable Mesh Insertion and Patient Satisfaction in Breast-Conserving Surgery
- Reduction of Trapdoor Type Orbital Floor Fracture with Absorbable Mesh