J Breast Cancer.
2009 Sep;12(3):151-155. 10.4048/jbc.2009.12.3.151.
The Use of Absorbable Surgical Mesh after Partial Mastectomy for Improving the Cosmetic Outcome
- Affiliations
-
- 1Department of Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. yonglai.park@samsung.com
- KMID: 2242005
- DOI: http://doi.org/10.4048/jbc.2009.12.3.151
Abstract
- PURPOSE
Partial mastectomy without immediate volume replacement can be associated with cosmetic failure. The aim of the present study was to assess cosmesis achieved in patients who underwent partial mastectomy and reconstruction using absorbable surgical mesh.
METHODS
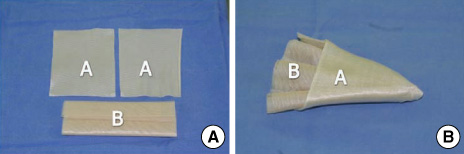
We used absorbable surgical mesh (Polyglactin 910, Vicryl(R)) to repair defects after performing partial mastectomy in 25 patients. Endoscopy-assisted partial mastectomy was performed with conservation of the whole skin of the breast and areola. A tailored fan-shape mesh was inserted into the postoperative defect. The cosmetic appearance was evaluated using a simplified five-grade for five-items scoring system at 3 and 6 months after the operation.
RESULTS
An excellent or good cosmetic result was obtained in 82.6% of the patients (19/23) after 3 and 6 months, and no major complications were noted.
CONCLUSION
This procedure can be easily performed by general surgeons. Insertion of an absorbable surgical mesh into the postoperative defect could be an effective modality for reconstructing a defect after breast surgery.
MeSH Terms
Figure
Cited by 2 articles
-
Results from Over One Year of Follow-Up for Absorbable Mesh Insertion in Partial Mastectomy
Min Young Koo, Se Kyung Lee, Sung Mo Hur, Soo Youn Bae, Min-Young Choi, Dong Hui Cho, Sangmin Kim, Jun-Ho Choe, Jung-Han Kim, Jee Soo Kim, Jeong Eon Lee, Seok Jin Nam, Jung-Hyun Yang
Yonsei Med J. 2011;52(5):803-808. doi: 10.3349/ymj.2011.52.5.803.The Suitability of Absorbable Mesh Insertion for Oncoplastic Breast Surgery in Patients with Breast Cancer Scheduled to Be Irradiated
Taehyun Kim, Heunglae Cho
J Breast Cancer. 2013;16(1):84-89. doi: 10.4048/jbc.2013.16.1.84.
Reference
-
1. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002. 347:1233–1241.
Article2. Raja MA, Straker VF, Rainsbury RM. Extending the role of breast-conserving surgery by immediate volume replacement. Br J Surg. 1997. 84:101–105.
Article3. Sanuki J, Higa K, Wadamori K, Fukuma E. Filling method to defect part of mammary gland after breast-conserving therapy by using polyglycol mesh. J Jpn Surg Soc. 2003. 104:243.4. Sanuki J, Fukuma E, Wadamori K, Higa K, Sakamoto N, Tsunoda Y. Volume replacement with polyglycolic acid mesh for correcting breast deformity after endoscopic conservative surgery. Clin Breast Cancer. 2005. 6:175.
Article5. Yamashita K, Shimizu K. Video-assisted breast surgery: reconstruction after resection of more than 33% of the breast. J Nippon Med Sch. 2006. 73:320–327.
Article6. Takahito S, Tatsuya T, Jun M, Toshinobu A, Junkichi K, Satoshi K. Endoscopic partial mastectomy and breast reconstruction using 3-dimentional mash. Geka. 2007. 69:230–232.7. Lee EK, Kook SH, Park YL, Bae WG. Endoscopy-assisted breast-conserving surgery for early breast cancer. World J Surg. 2006. 30:957–964.
Article8. Yamashita K. Cosmetic assessment. J Jpn Soc Endosc Surg. 2005. 10:165–170.9. Veronesi U, Banfi A, Salvadori B, Luini A, Saccozzi R, Zucali R, et al. Breast conservation is the treatment of choice in small breast cancer: long-term results of a randomized trial. Eur J Cancer. 1990. 26:668–670.
Article10. Fujishiro S, Mitsumori M, Kokubo M, Nagata Y, Sasai K, Mise K, et al. Cosmetic results and complications after breast conserving therapy for early breast cancer. Breast Cancer. 2000. 7:57–63.
Article11. Lindsey I, Serpell JW, Johnson WR, Rodger A. Cosmesis following complete local excision of breast cancer. Aust N Z J Surg. 1997. 67:428–432.
Article12. Beauchamp PJ, Guzick DS, Held B, Schmidt WA. Histologic response to microsuture materials. J Reprod Med. 1988. 33:615–623.13. Klinge U, Schumpelick V, Klosterhalfen B. Functional assessment and tissue response of short- and long-term absorbable surgical meshes. Biomaterials. 2001. 22:1415–1424.
Article14. Bourne RB, Bitar H, Andreae PR, Martin LM, Finlay JB, Marquis F. In-vivo comparison of four absorbable sutures: Vicryl, Dexon Plus, Maxon and PDS. Can J Surg. 1988. 31:43–45.15. Craig PH, Williams JA, Davis KW, Magoun AD, Levy AJ, Bogdansky S, et al. A biologic comparison of polyglactin 910 and polyglycolic acid synthetic absorbable sutures. Surg Gynecol Obstet. 1975. 141:1–10.16. Hatada T, Ishii H, Ichii S, Ashida H, Yamamura T. Late infection after mesh-plug inguinal hernioplasty. Am J Surg. 2000. 179:76–77.
Article17. Yamamoto S, Maeda T, Uchida Y, Yabe S, Nakano M, Sakano S, et al. Open tension-free mesh repair for adult inguinal hernia: eight years of experience in a community hospital. Asian J Surg. 2002. 25:121–125.
Article18. Spear SL, Mardini S, Ganz JC. Resource cost comparison of implant-based breast reconstruction versus TRAM flap breast reconstruction. Plast Reconstr Surg. 2003. 112:101–105.
Article19. Blondeel N, Vanderstraeten GG, Monstrey SJ, Van Landuyt K, Tonnard P, Lysens R, et al. The donor site morbidity of free DIEP flaps and free TRAM flaps for breast reconstruction. Br J Plast Surg. 1997. 50:322–330.
Article20. Son BH, Lee TJ, Lee SW, Hwang UK, Kwak BS, Ahn SH. Increase of fat necrosis after radiation therapy following mastectomy and immediate TRAM flap reconstruction in high-risk breast cancer patients. J Korean Breast Cancer Soc. 2004. 7:17–21.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Suitability of Absorbable Mesh Insertion for Oncoplastic Breast Surgery in Patients with Breast Cancer Scheduled to Be Irradiated
- Ultrasonographic Findings of an Implanted Absorbable Mesh in Patients with Breast Partial Resection: a Preliminary Study
- Imaging Findings of Implanted Absorbable Mesh in Patients with Breast Partial Resection
- The Use of a Corrective Procedure with Vicryl Mesh for Oncoplastic Surgery of the Breast
- Results from Over One Year of Follow-Up for Absorbable Mesh Insertion in Partial Mastectomy