Korean J Ophthalmol.
2011 Aug;25(4):243-247. 10.3341/kjo.2011.25.4.243.
Macular Gradient Measurement in Myopic Posterior Staphyloma Using Optical Coherence Tomography
- Affiliations
-
- 1Department of Ophthalmology, Chungbuk National University College of Medicine, Cheongju, Korea.
- 2Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. dropkim@dreamwiz.com
- 3Department of Ophthalmology, Gangneung Asan Medical Center, University of Ulsan College of Medicine, Gangneung, Korea.
- KMID: 1018411
- DOI: http://doi.org/10.3341/kjo.2011.25.4.243
Abstract
- PURPOSE
To evaluate clinical characteristics and the macular gradient in myopic posterior staphyloma with time domain (TD) optical coherence tomography (OCT).
METHODS
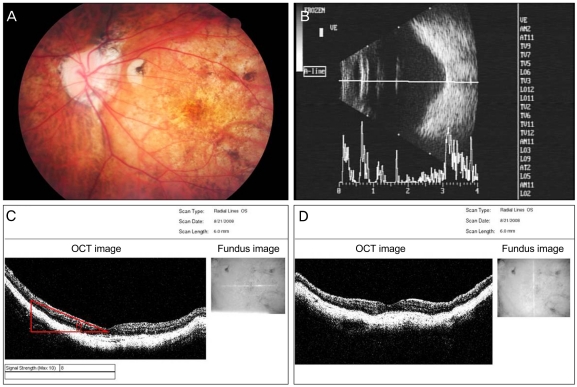
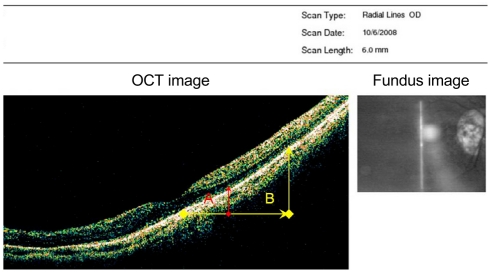
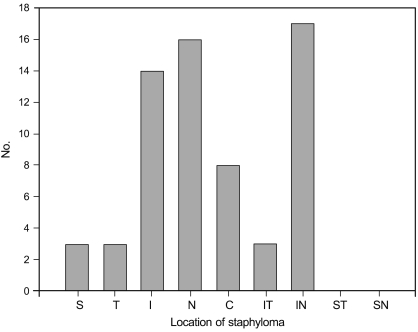
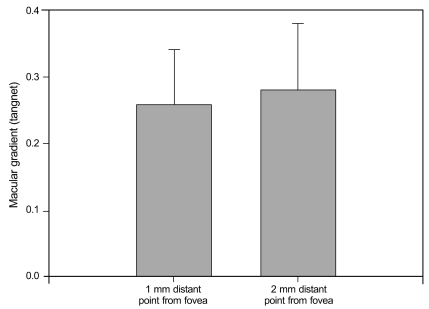
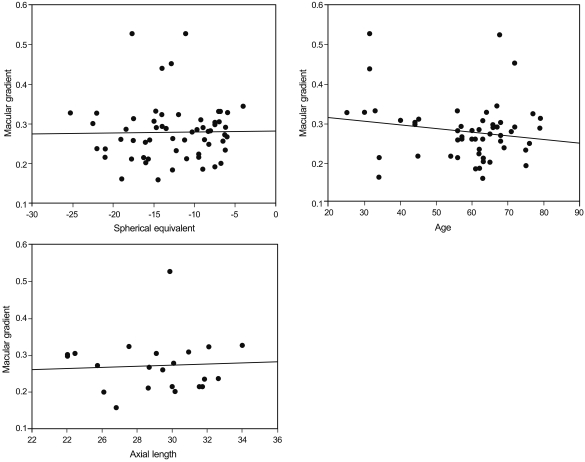
Sixty-four staphyloma eyes of 40 patients were examined. Macular gradient (tangent theta) and the location of staphyloma were assessed with OCT imaging. The macular gradient was measured at points 1 mm and 2 mm distant from the fovea. The relationships of the macular gradient with age, axial length, and spherical equivalent were analyzed.
RESULTS
In 8 eyes (12.5%), the bottoms of the staphylomas were in the fovea, and there was no macular gradient. However, in the other 56 eyes (87.5%), the bottoms of the staphylomas were not in the foveal area, and macular gradients existed. Staphylomas were commonly located in the infero-nasal retinal area. The mean macular gradient (tangent theta) was 0.26 +/- 0.08 at 1 mm distance from the fovea and 0.28 +/- 0.10 at 2 mm. No significant relationships were observed between macular gradient and axial length, patient age, or spherical equivalent.
CONCLUSIONS
TD OCT reveals staphyloma location. If the location is outside of the fovea, a macular gradient exists and can be measured by OCT. Axial length measurement error may occur in eyes with poor visual fixation and steep macular gradients.
Keyword
MeSH Terms
Figure
Reference
-
1. Hsiang HW, Ohno-Matsui K, Shimada N, et al. Clinical characteristics of posterior staphyloma in eyes with pathologic myopia. Am J Ophthalmol. 2008; 146:102–110. PMID: 18455142.
Article2. Grossniklaus HE, Green WR. Pathologic findings in pathologic myopia. Retina. 1992; 12:127–133. PMID: 1439243.
Article3. Wong TY, Foster PJ, Hee J, et al. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci. 2000; 41:2486–2494. PMID: 10937558.4. Curtin BJ. The pathogenesis of congenital myopia. A study of 66 cases. Arch Ophthalmol. 1963; 6:166–173. PMID: 14024344.5. Curtin BJ. The posterior staphyloma of pathologic myopia. Trans Am Ophthalmol Soc. 1977; 75:67–86. PMID: 613534.6. Gaucher D, Erginay A, Lecleire-Collet A, et al. Dome-shaped macula in eyes with myopic posterior staphyloma. Am J Ophthalmol. 2008; 145:909–914. PMID: 18342827.
Article7. Takano M, Kishi S. Foveal retinoschisis and retinal detachment in severely myopic eyes with posterior staphyloma. Am J Ophthalmol. 1999; 128:472–476. PMID: 10577588.
Article8. Toranzo J, Cohen SY, Erginay A, Gaudric A. Peripapillary intrachoroidal cavitation in myopia. Am J Ophthalmol. 2005; 140:731–732. PMID: 16226529.
Article9. Sayanagi K, Ikuno Y, Gomi F, Tano Y. Retinal vascular microfolds in highly myopic eyes. Am J Ophthalmol. 2005; 139:658–663. PMID: 15808161.
Article10. Nakanishi H, Tsujikawa A, Gotoh N, et al. Macular complications on the border of an inferior staphyloma associated with tilted disc syndrome. Retina. 2008; 28:1493–1501. PMID: 18667957.
Article11. Leys AM, Cohen SY. Subretinal leakage in myopic eyes with a posterior staphyloma or tilted disk syndrome. Retina. 2002; 22:659–665. PMID: 12441740.
Article12. Tsuboi S, Uchihori Y, Manabe R. Subretinal neovascularisation in eyes with localised inferior posterior staphylomas. Br J Ophthalmol. 1984; 68:869–872. PMID: 6210100.
Article13. Prost M, De Laey JJ. Choroidal neovascularization in tilted disc syndrome. Int Ophthalmol. 1988; 12:131–135. PMID: 2466011.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Shortest Radius of Curvature of Bruch's Membrane in Macular Optical Coherence Tomography
- Macular Buckling Surgery Using a Novel L-shaped Buckle for Patients with Myopic Tractional Maculopathy
- Use of Spectral-Domain Optical Coherence Tomography to Analyze Macular Thickness According to Refractive Error
- Incidence and Risk Factors of Cystoid Macular Edema after Vitrectomy with Silicone Oil Tamponade for Retinal Detachment
- The Correlation between Visual Acuity and Patterns of Diabetic Macular Edema in OCT Images