J Korean Acad Nurs.
2009 Jun;39(3):422-432. 10.4040/jkan.2009.39.3.422.
Rest-Activity Rhythm, Sleep Pattern and Quality of Life in Patients with Restless Legs Syndrome
- Affiliations
-
- 1Department of Nursing, Andong Science College, Andong, Korea. vinuslee@kmu.ac.kr
- KMID: 999312
- DOI: http://doi.org/10.4040/jkan.2009.39.3.422
Abstract
-
PURPOSE: In this study rest-activity rhythm, sleep pattern and quality of life of patients with restless legs syndrome were compared with those of a normal group.
METHODS
The participants in this study were 36 patients with restless legs syndrome diagnosed by a neurologist and 36 participants in the normal group. An actigraph, sleep diary, Pittsburgh Sleep Quality Index and Insomnia Severity Index scale were used as measurement tools for the study. Chi-square test, Lamda test, t-test and Kendall's correlation with SPSS 12.0 program were used to analyze the data.
RESULTS
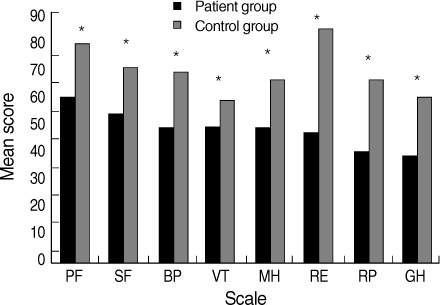
Patients with restless legs syndrome had a higher rest-activity rhythm curve of Least 5 hr's activity (L5) and Most 10 hr's activity (M10) than those of normal group and sleep problems included decreased sleep efficiency and increased sleep latency, wake time and number of awakenings. The scores for the subscales of quality of life in patients with restless legs syndrome were lower than the normal group for general health, physical functioning, role limitations due to emotional problems, role limitation due to physical problems, social functioning, bodily pain, vitality and mental health.
CONCLUSION
The results suggest that further studies are needed to identify rest-activity rhythm according to symptom severity and to develop nursing interventions which consider rest-activity rhythm.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Metabolic Syndrome and Health-Related Quality of Life among Patients with Liver Transplantation
Suejin Kim, Jina Choo
Korean J Health Promot. 2022;22(3):153-164. doi: 10.15384/kjhp.2022.22.3.153.
Reference
-
1. Abetz L, Allen R, Follet A, Washburn T, Earley C, Kirsch J, et al. Evaluating the quality of life of patients with restless legs syndrome. Clinical Therapeutics. 2004. 26:925–935.2. Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisi J. Restless legs syndrome: Diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Medicine. 2003. 4:101–119.3. Barriere G, Cazalets JR, Bioulac B, Tison F, Ghorayeb I. The restless legs syndrome. Progress in Neurobiology. 2005. 77:139–165.4. Bastien BH, Vallieres C, Morin CM. Validation of the Insomnia Severity Index as an outcome for insomnia research. Sleep Medicine. 2001. 2:297–307.5. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kuper DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1998. 28:193–213.6. Cho YW, Lee H, Lee JW, Han SY, Lee MY. Sleep disorders in maintenance dialysis patients with end-stage renal disease. Journal of the Korean Neurological Association. 2003. 21:492–498.7. Cho YW, Yun CH, Shin YC, Hong SB. Prevalence of restless legs syndrome. 2006. 04. In : Paper presented at the annual meeting of the Korean Sleep Research Society; Seoul.8. Cohen J. A power primer. Psychological Bulletin. 1992. 112:155–159.9. Ekbom KA. Restless legs. Journal of Internal Medicine. 1945. 158:121–123.10. Ekbom KA. Restless legs syndrome. Neurology. 1960. 10:868–874.11. Enomoto M, Li L, Aritake S, Nagase Y, Kaji T, Tagaya H, et al. Restless legs syndrome and its correlation with other sleep problem in the general adult population of Japan. Sleep and biological rhythm. 2006. 4:153–159.12. Fichten CS, Creti L, Amsel R, Brender W, Weinstein N, Libman E. Poor sleepers who do not complain of insomnia: Myths and realities about psychological and lifestyle characteristics of older good and poor sleepers. Journal of Behavioral Medicine. 1995. 18:189–223.13. Fossey M, Libman E, Bailes S, Baltzan M, Schondorf R, Amsel R, et al. Sleep quality and psychological adjustment in chronic fatigue syndrome. Journal of Behavioral Medicine. 2004. 27:581–603.14. Garcia-Borreguero D, Larrosa O, Llave YD, Granizo JJ, Allen R. Correlation between rating scales and sleep laboratory measurements in restless legs syndrome. Sleep Medicine. 2004. 5:561–565.15. Hening WA, Walters AS, Wagner M, Rosen R, Chen V, Kim S, et al. Circadian rhythm of motor restlessness and sensory symptoms in the idiopathic restless legs syndrome. Sleep. 1999. 22:901–912.16. Huang YL, Liu RY, Wang QS, Van Someren EJ, Xu H, Zhou JN. Age-associated difference in circadian sleep-wake and rest-activity rhythms. Physiology & Behavior. 2002. 76:597–603.17. Jean-Louis G, Zizi F, Von Gizycki H, Hauri P. Actigraphic assessment of sleep in insomnia: Application of the Actigraph Data Analysis Software (ADAS). Physiology & Behavior. 1999. 65:659–663.18. Kim J, Choi C, Shin K, Yi H, Park M, Cho N, et al. Prevalence of restless legs syndrome and associated factors in the Korean adult population: The Korean health and genome study. Psychiatry and Clinical Neurosciences. 2005. 59:350–353.19. Kim OS, Kim AJ, Kim SW, Baik SH, Yang KM. Fatigue, depression and sleep in young adult and middle-aged. Journal of Korean Academy of Nursing. 2003. 33:618–624.20. Kim SM, Oh JJ, Song MS, Park YH. Comparison of sleep and related variables between young and old adults. Journal of Korean Academy of Nursing. 1997. 27:820–830.21. Koh SB, Chang SJ, Kang MG, Cha BS, Park JK. Reliability and validity on measurement instrument for health status assessment in occupational workers. Journal of Preventive Medicine and Public Health. 1997. 30:251–265.22. Kushida CA, Allen RP, Atkinson MJ. Modeling the causal relationships between symptoms associated with restless legs syndrome and the patient-reported impact of RLS. Sleep Medicine. 2004. 5:485–488.23. Lee JY. Sleep patterns of patients with restless legs syndrome measured by actigraph. 2006. Daegu: Keimyung University;Unpublished master's thesis.24. Michaud M, Dumont M, Selmaoui B, Paquet J, Fantini ML, Montplaisir J. Circadian rhythm of restless legs syndrome: Relationship with biological markers. Annals of Neurology. 2004. 55:372–380.25. Nicolas A, Michaud M, Lavigne G, Montplaisir J. The influence of sex, age and sleep/wake state on characteristics of periodic leg movements in restless legs syndrome patients. Clinical Neurophysiology. 1999. 110:1168–1174.26. Sforza E, Jouny C, Ibanez V. Time course of arousal response during periodic leg movements in patients with periodic leg movements and restless legs syndrome. Clinical Neurophysiology. 2003. 114:1116–1124.27. Shin KR, Yi HR, Kim JY, Shin C. Prevalence and associated factors of excessive daytime sleepiness in adults. Journal of Korean Academy of Nursing. 2006. 36:829–836.28. Tryon WW. Issues of validity in actigraphic sleep assessment. Sleep. 2004. 27:158–165.29. Van Someren EJ, Swaab DF, Colenda CC, Cohen W, McCall WV, Rosenquist PB. Bright light therapy: Improved sensitivity to its effects on rest-activity rhythms in Alzheimer patients by application of nonparametric methods. Chronobiology International. 1999. 16:505–518.30. Ware JJ, Sherboume C. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992. 30:473–483.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Introduction for the Questionnaires for Restless Legs Syndrome
- Dopamine Agonists in the Treatment of Restless Legs Syndrome: Too Much of a Good Thing?
- Sleep Disorders in Patients with Parkinson's Disease
- Diagnosis and Treatment of Restless Leg Syndrome and Periodic Limb Movement of Sleep
- Quality of Sleep and Serum Lipid Profile in Patients with Restless Legs Syndrome