Korean J Ophthalmol.
2010 Apr;24(2):126-130. 10.3341/kjo.2010.24.2.126.
A Case of Optic Neuritis Complicating Herpes Zoster Ophthalmicus in a Child
- Affiliations
-
- 1Department of Ophthalmology, Wonkwang University School of Medicine, Iksan, Korea. ysyang@wonkwang.ac.kr
- KMID: 946006
- DOI: http://doi.org/10.3341/kjo.2010.24.2.126
Abstract
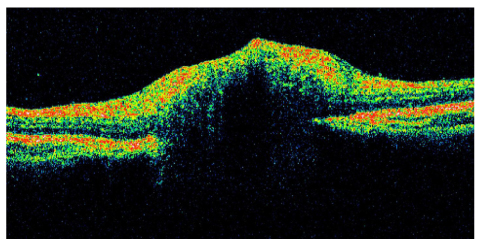
- Here we report a case of optic neuritis in the setting of herpes zoster ophthalmicus (HZO) in a child. A six-year-old girl presented with HZO in the right eye. During the hospitalization, her visual acuity decreased. Fluorescein angiography (FAG) and optical coherence tomography revealed optic neuritis in the affected eye. Visual acuity improved with one month of treatment with acyclovir and steroids. FAG analysis showed no evidence of leakage at the optic disc. At one year post treatment, the patient's fundus exam and vision were normal. Therapy with antivirals and steroids may be effective in patients with childhood HZO optic neuritis
Keyword
MeSH Terms
Figure
Reference
-
1. Weller TH. Varicella and herpes zoster: changing concept of the natural history, control, and importance of a not-so-benign virus. N Engl J Med. 1983. 309:1362–1368.2. Pavan-Langston D. Foster CS, Azar D, Dohlman CH, editors. Viral disease of the ocular anterior segment: basic science and clinical disease. The cornea. 2005. Philadelphia: Lippincott Williams & Wilkins;297–397.3. Culbertson WW, Blemenkranz MS, Pepose JS, et al. varicella zoster virus is a cause of the acute retinal necrosis syndrome. Ophthalmology. 1986. 93:559–569.4. Hope-Simpson RE. The nature of herpes zoster: a long term study and a new hypothesis. Proc R Soc Med. 1965. 58:9–20.5. Juel-Jensen BE, MacCallum FO. Herpes simplex varicella and zoster. 1972. Philadelphia: Lippincott;109.6. Kattah JC, Kennerdell JS. Orbital apex syndrome secondary to herpes zoster ophthalmicus. Am J Ophthalmol. 1978. 85:378–382.7. Paton L. The trigeminal and its ocular lesions. Br J Ophthalmol. 1926. 10:305–321.8. Hamard H, Chevaleraud J, Rondot P. Neuropathies optiques Inflammatoires et infectieuses. Neuropathies optiques. 1986. Paris: Masson;281.9. Edgerton AE. Herpes zoster ophthalmicus: report of cases and review of literature. Arch Ophthal. 1945. 34:114–153.10. Liang MG, Heidelberg KA, Jacobson RM, McEvoy MT. Herpes zoster after varicella immunization. J Am Acad Dermatol. 1998. 38:761–763.11. Straus SE, Reinhold W, Smith HA, et al. Endonuclease analysis of viral DNA from varicella and subsequent zoster infections in the same patient. N Engl J Med. 1984. 311:1362–1364.12. Burke BL, Steele RW, Beard OW, et al. Immune responses to varicella-zoster in the aged. Arch Intern Med. 1982. 142:291–293.13. Baba K, Yabuuchi H, Takahashi M, Ogra PL. Increased incidence of herpes zoster in normal children infected with varicella zoster virus during infancy: community-based follow-up study. J Pediatr. 1986. 108:372–377.14. David TJ, Williams ML. Herpes zoster in infancy. Scand J Infect Dis. 1979. 11:185–186.15. Uebe B, Sauerbrei A, Burdach S, Horneff G. Herpes zoster by reactivated vaccine varicella zoster virus in a healthy child. Eur J Pediatr. 2002. 161:442–444.16. Gilden DH, Cohrs RJ, Mahalingam R. VZV vasculopathy and postherpetic neuralgia: progress and perspective on antiviral therapy. Neurology. 2005. 64:21–25.17. Shaikh S, Ta CN. Evaluation and management of herpes zoster ophthalmicus. Am Fam Physician. 2002. 66:1723–1730.18. Monroe LD. Optic neuritis in a child with herpes zoster. Ann Ophthalmol. 1979. 11:405–406.19. Gündüz K, Ozdemir O. Bilateral retrobulbar neuritis following unilateral herpes zoster ophthalmicus. Ophthalmologica. 1994. 208:61–64.20. Mori T, Terai T, Hatano M, et al. Stellate ganglion block improved loss of visual acuity caused by retrobulbar optic neuritis after herpes zoster. Anesth Analg. 1997. 85:870–871.21. Scharf Y, Kraus E, Zonis S. Optic neuropathy and central retinal artery occlusion in a case of herpes zoster ophthalmicus. Ann Ophthalmol. 1987. 19:77–78.22. Tyring S, Engst R, Corriveau C, et al. Famciclovir for ophthalmic zoster: a randomized aciclovir controlled study. Br J Ophthalmol. 2001. 85:576–581.23. Whitley RJ, Gnann JW Jr. Acyclovir: a decade later. N Engl J Med. 1992. 327:782–789.24. Davis LE, King MK. Shingles (herpes zoster) and post-herpetic neuralgia. Curr Treat Options Neurol. 2001. 3:401–411.25. Marsh RJ, Cooper M. Ophthalmic herpes zoster. Eye. 1993. 7:350–370.26. Wood MJ, Johnson RW, McKendrick MW, et al. A randomized trial of acyclovir for 7 days or 21 days with and without prednisolone for treatment of acute herpes zoster. N Engl J Med. 1994. 330:896–900.27. Ramsell TG. Complications of herpes zoster ophthalmicus. Am J Ophthalmol. 1967. 63:1796–1798.28. Caroll WM, Mastaglia FL. Optic neuropathy and ophthalmoplegia in herpes zoster oticus. Neurology. 1979. 29:726–729.29. Schmidt P. Herpes zoster ophthalmicus with retrobulbar neuritis. A case report. Acta Ophthalmol. 1983. 61:501–509.30. Tunis SW, Tapert MJ. Acute retrobulbar neuritis complicating herpes zoster ophthalmicus. Ann Ophthalmol. 1987. 19:453–456.31. Atmaca LS, Ozmert E. Optic neuropathy and central retinal artery occlusion in a patient with herpes zoster ophthalmicus. Ann Ophthalmol. 1992. 24:50–53.32. Wang AG, Liu JH, Hsu WM, et al. Optic neuritis in herpes zoster ophthalmicus. Jpn J Ophthalmol. 2000. 44:550–554.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Herpes Zoster Ophthalmicus Complicated by Abducens Palsy
- Two Cases of Optic Neuritis in Herpes Zoster Ophthalmicus
- Acute Vestibular Neuritis Associated with Herpes Zoster Ophthalmicus
- Complicated Ophthalmopathy in Herpes Zoster Ophthalmicus Including Vitreous Opacity, Retinal Hemorrhage and Optic Neuropathy
- Ophthalmoplegia in Herpes Zoster Ophthalmicus