Korean J Ophthalmol.
2010 Jun;24(3):179-181. 10.3341/kjo.2010.24.3.179.
Progression of Impending Central Retinal Vein Occlusion to the Ischemic Variant Following Intravitreal Bevacizumab
- Affiliations
-
- 1Department of Ophthalmology, Inha University School of Medicine, Incheon, Korea. hschin@inha.ac.kr
- KMID: 945991
- DOI: http://doi.org/10.3341/kjo.2010.24.3.179
Abstract
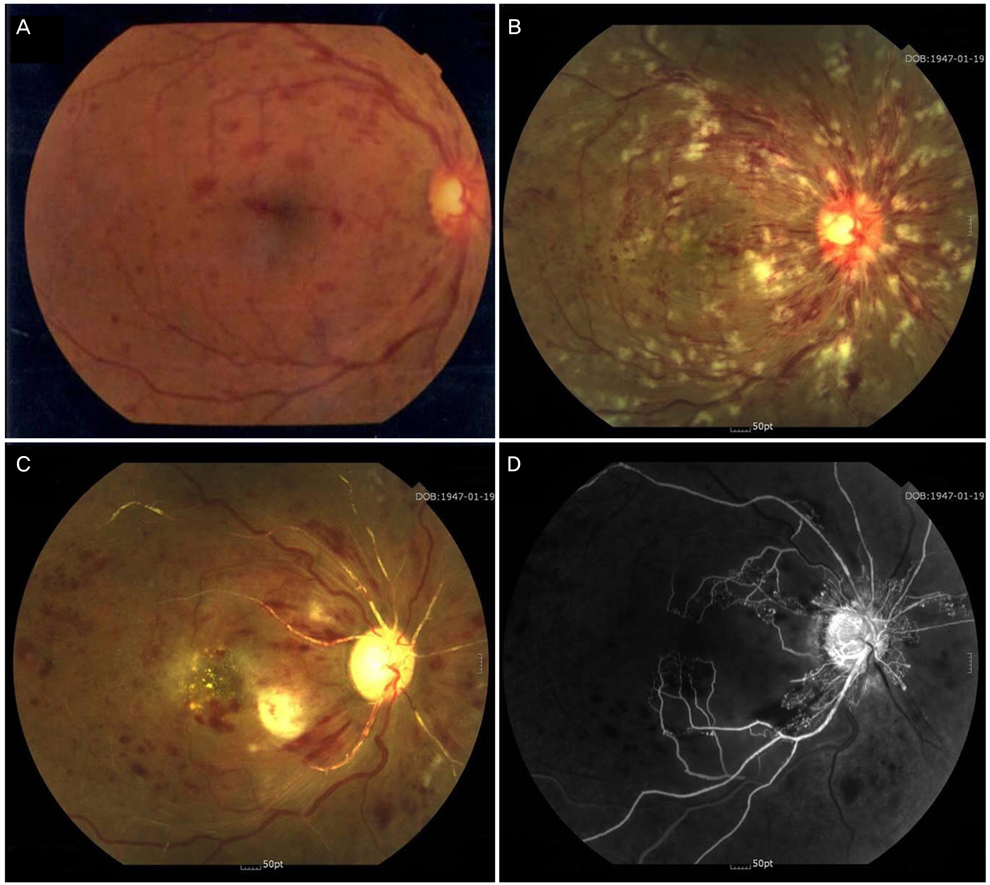
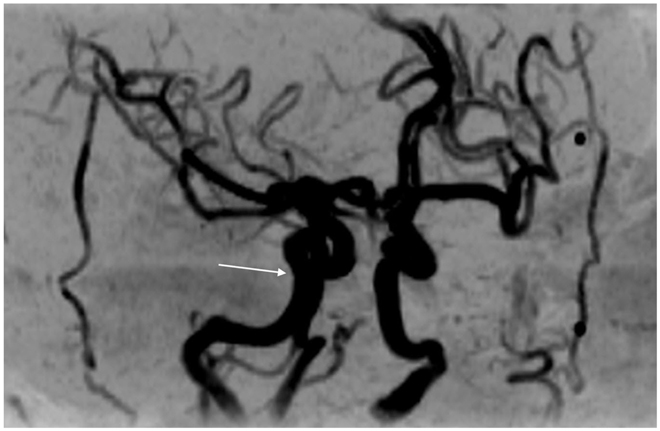
- A 60-year-old woman who had experienced two episodes of amaurosis fugax in her right eye presented with vision loss. Two weeks earlier, at a private clinic, she was diagnosed with impending central retinal vein occlusion (CRVO) of the right eye and received an intravitreal injection of bevacizumab. Two weeks after this injection she was diagnosed with ischemic CRVO. At 11-weeks post-presentation, extremely ischemic features were observed with fluorescein angiographic findings of severe vascular attenuation and extensive retinal capillary obliteration. At 22-weeks post-presentation she was diagnosed with neovascular glaucoma; she experienced no visual improvement over the following several months.
MeSH Terms
-
Antibodies, Monoclonal/*administration & dosage
Disease Progression
Female
Fluorescein Angiography
Glaucoma, Neovascular/complications
Humans
Injections, Intraocular
Ischemia/diagnosis/*etiology/physiopathology
Middle Aged
Retinal Vein Occlusion/*complications/*drug therapy/physiopathology
*Retinal Vessels
Vascular Endothelial Growth Factor A/antagonists & inhibitors
Visual Acuity/drug effects
Vitreous Body
Figure
Cited by 2 articles
-
Ocular and Systemic Manifestation of Amaurosis Fugax: Six-Year Observational Study
Tae Hwan Moon, Ju Byung Chae
J Korean Ophthalmol Soc. 2015;56(5):732-736. doi: 10.3341/jkos.2015.56.5.732.Amaurosis Fugax Associated with Ipsilateral Internal Carotid Artery Agenesis
Jae Yun Sung, Kyoung Nam Kim, Hye Seon Jeong, Yeon Hee Lee
J Korean Ophthalmol Soc. 2016;57(9):1484-1488. doi: 10.3341/jkos.2016.57.9.1484.
Reference
-
1. Gass JD. Stereoscopic atlas of macular diseases: diagnosis and treatment. 1997. 4th ed. St Louis: Mosby;546–555.2. Ziemssen F, Luke M, Messias A, et al. Safety monitoring in bevacizumab (Avastin) treatment: retinal function assessed by psychophysical (visual fields, colour vision) and electrophysiological (ERG/EOG) tests in two subgroups of patients. Int Ophthalmol. 2008. 28:101–109.3. Kim KS, Chang HR, Song S. Ischaemic change after intravitreal bevacizumab (Avastin) injection for macular oedema secondary to non-ischemic central retinal vein occlusion. Acta Ophthalmol. 2008. 86:925–927.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Bevacizumab and Combined Low-dose Bevacizumab and Triamcinolone in Central Retinal Vein Occlusion
- Intravitreal Bevacizumab Treatment of Macular Edema in Central Retinal Vein Occlusion
- The Efficacy of Intravitreal Bevacizumab in the Treatment of Macular Edema
- Intravitreal Bevacizumab Injection for Macular Edema Secondary to Branch Retinal Vein Occlusion: Long-Term Results
- A Case of Retinal Hemorrhage Following a Dexamethasone Intravitreal Implant