Korean J Gastroenterol.
2009 Oct;54(4):201-204. 10.4166/kjg.2009.54.4.201.
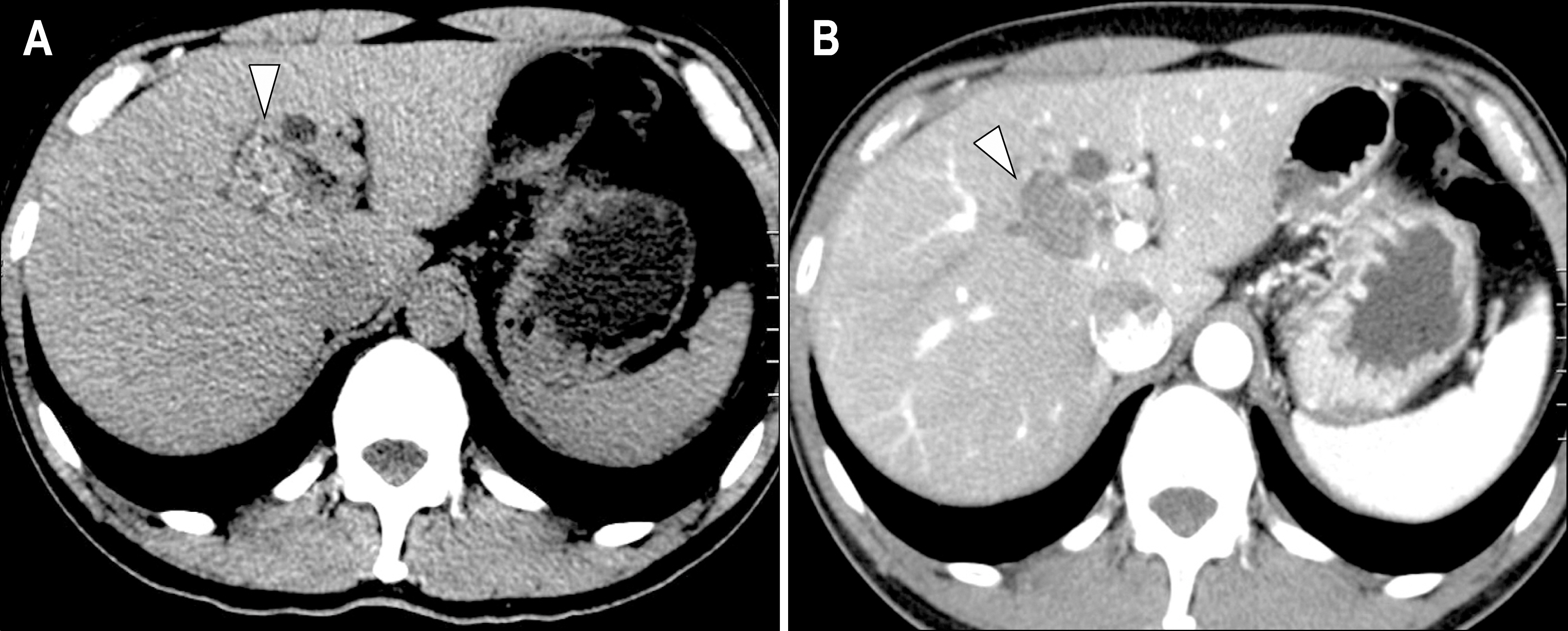
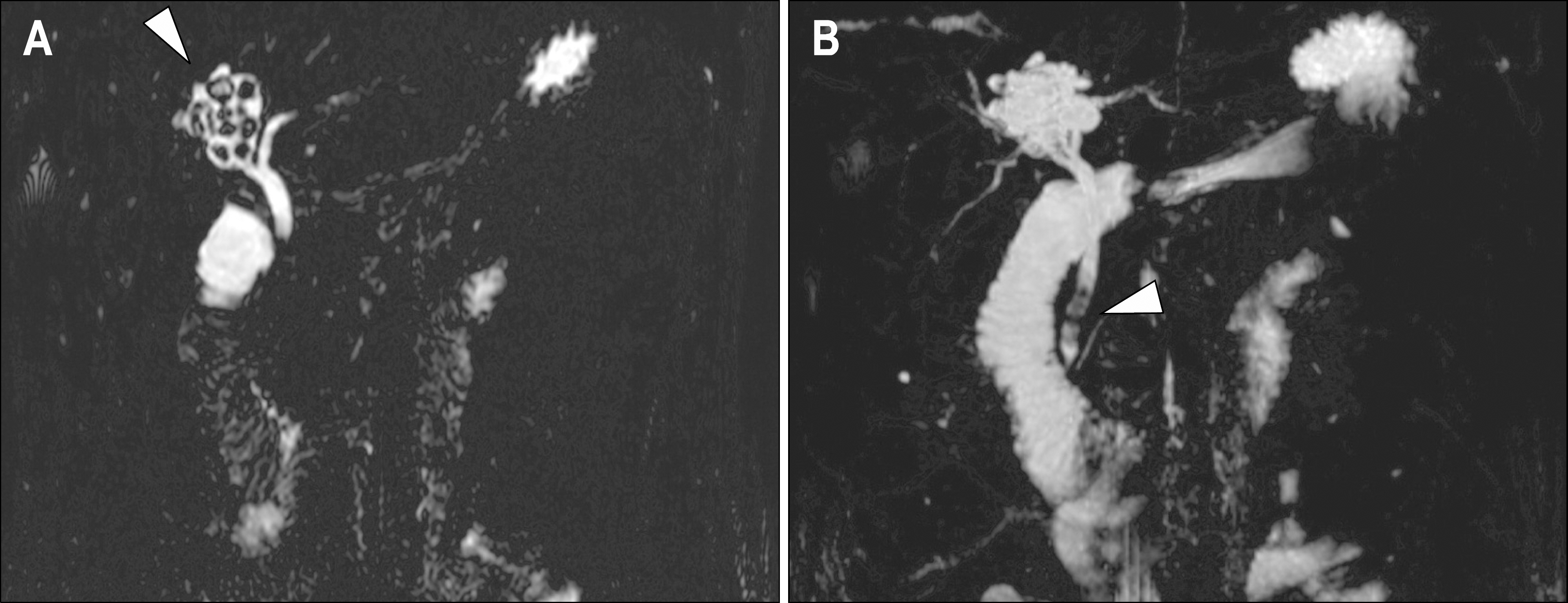
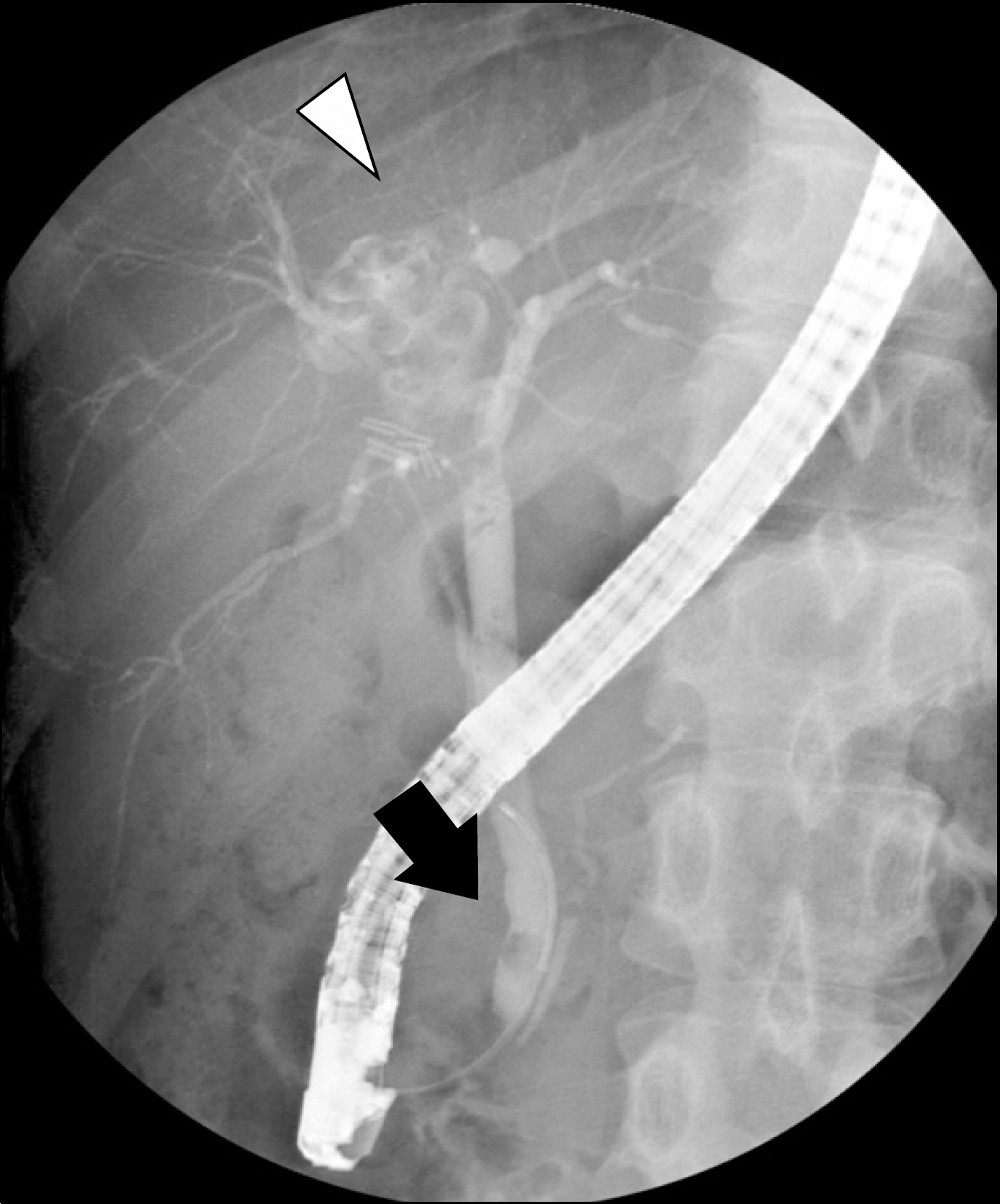
A Case of Caroli Disease with Biliary Stones
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. gidoctor@snubh.org
- 2Department of Radiology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 3Department of Pathology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 783224
- DOI: http://doi.org/10.4166/kjg.2009.54.4.201
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
1. Caroli J, Couinaud C, Soupault R, Porcher P, Eteve J. A new disease, undoubtedly congenital, of the bile ducts: unilobar cystic dilation of the hepatic ducts. Sem Hop. 1958; 34:496–502. /SP.2. Giovanardi RO. Monolobar Caroli's disease in an adult. Case report. Hepatogastroenterology. 2003; 50:2185–2187.3. Parada LA, Hallen M, Hagerstrand I, Tranberg KG, Johansson B. Clonal chromosomal abnormalities in congenital bile duct dilatation (Caroli's disease). Gut. 1999; 45:780–782.
Article4. Levy AD, Rohrmann CA Jr, Murakata LA, Lonergan GJ. Caroli's disease: radiologic spectrum with pathologic correlation. AJR Am J Roentgenol. 2002; 179:1053–1057.
Article5. Asselah T, Ernst O, Sergent G, L'Hermine C, Paris JC. Caroli's disease: a magnetic resonance cholangiopancreatography diagnosis. Am J Gastroenterol. 1998; 93:109–110.
Article6. Yilmaz S, Kirimlioglu H, Kirimlioglu V, et al. Partial hepatectomy is curative for the localized type of Caroli's disease: a case report and review of the literature. Surgeon. 2006; 4:101–105.
Article7. Bockhorn M, Malago M, Lang H, et al. The role of surgery in Caroli's disease. J Am Coll Surg. 2006; 202:928–932.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diffuse-Type Caroli Disease with Characteristic Central Dot Sign Complicated by Multiple Intrahepatic and Common Bile Duct Stones
- Unexpectedly Diagnosed Caroli's Disease on HIDA Scintigraphy in a Patient with Calculous Cholecystitis
- Monolobar Caroli's Disease in Left Lobe of the Liver: A Case Report
- A case of Caroli's disease
- A Case Report of Caroli's Disease