Korean J Radiol.
2002 Sep;3(3):163-170. 10.3348/kjr.2002.3.3.163.
Multiphasic Perfusion CT in Acute Middle Cerebral Artery Ischemic Stroke: Prediction of Final Infarct Volume and Correlation with Clinical Outcome
- Affiliations
-
- 1Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dgna@smc.samsung.co.kr
- 2Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 754058
- DOI: http://doi.org/10.3348/kjr.2002.3.3.163
Abstract
OBJECTIVE
To assess the utility of multiphasic perfusion CT in the prediction of final infarct volume, and the relationship between lesion volume revealed by CT imaging and clinical outcome in acute ischemic stroke patients who have not undergone thrombolytic therapy.
MATERIALS AND METHODS
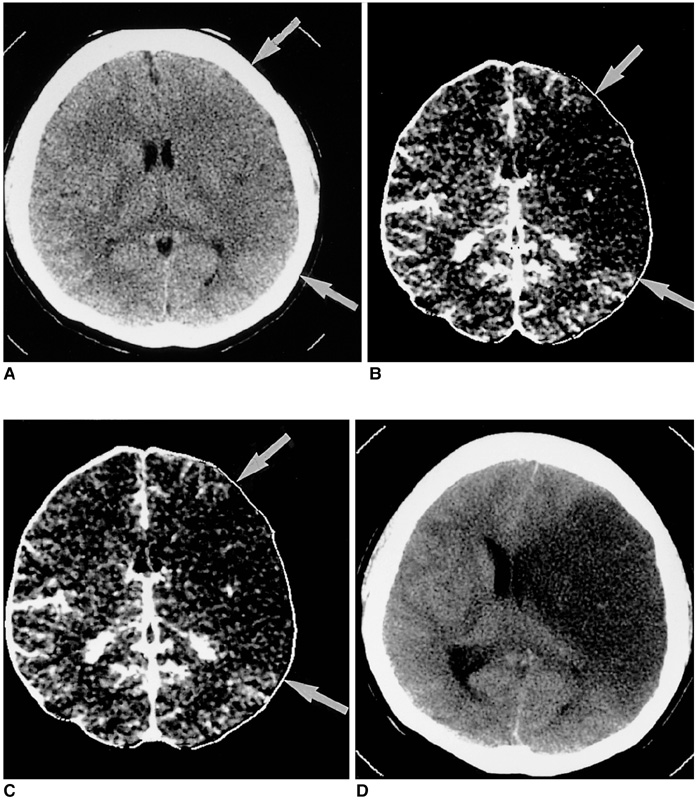
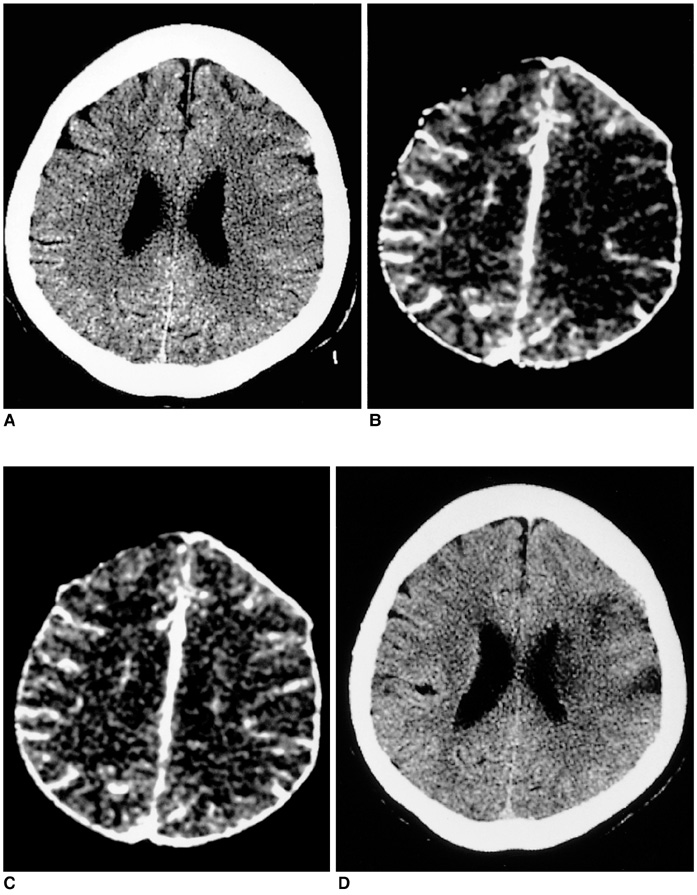
Thirty-five patients underwent multiphasic perfusion CT within six hours of stroke onset. After baseline unenhanced helical CT scanning, contrast-enhanced CT scans were obtained 20, 34, 48, and 62 secs after the injection of 90 mL contrast medium at a rate of 3 mL/sec. CT peak and total perfusion maps were obtained from serial CT images, and the initial lesion volumes revealed by CT were compared with final infarct volumes and clinical scores.
RESULTS
Overall, the lesion volumes seen on CT peak perfusion maps correlated most strongly with final infarct volumes (R2=0.819, p<0.001, slope of regression line=1.016), but individual data showed that they were less than final infarct volume in 31.4% of patients. In those who showed early clinical improvement (n=6), final infarct volume tended to be overestimated by CT peak perfusion mapping and only on total perfusion maps was there significant correlation between lesion volume and final infarct volume (R2=0.854, p=0.008). The lesion volumes depicted by CT maps showed moderate correlation with baseline clinical scores and clinical outcomes (R=0.445-0.706, p<=0.007).
CONCLUSION
CT peak perfusion maps demonstrate strong correlation between lesion volume and final infarct volume, and accurately predict final infarct volume in about two-thirds of the 35 patients. The lesion volume seen on CT maps shows moderate correlation with clinical outcome.
MeSH Terms
-
Acute Disease
Adult
Aged
Aged, 80 and over
Blood Volume/*physiology
Cerebrovascular Circulation/physiology
Contrast Media
Female
Human
Infarction, Middle Cerebral Artery/*physiopathology/*radiography
Male
Middle Age
Middle Cerebral Artery/*physiopathology/*radiography
Predictive Value of Tests
Prognosis
Retrospective Studies
Tomography, X-Ray Computed
Figure
Reference
-
1. Shrier DA, Tanaka H, Numaguchi Y, Konno S, Patel U, Shibata D. CT angiography in the evaluation of acute stroke. Am J Neuroradiol. 1997. 18:1011–1020.2. Knauth M, von Kummer R, Jansen O, Hahnel S, Dorfler A, Sartor K. Potential of CT angiography in acute ischemic stroke. Am J Neuroradiol. 1997. 18:1001–1010.3. Hunter GJ, Hamberg LM, Ponzo JA, et al. Assessment of cerebral perfusion and arterial anatomy in hyperacute stroke with three-dimensional functional CT: early clinical results. Am J Neuroradiol. 1998. 19:29–37.4. Na DG, Byun HS, Lee KH, et al. Acute occlusion of the middle cerebral artery: early evaluation with triphasic helical CT-preliminary results. Radiology. 1998. 207:113–122.5. Lee KH, Cho SJ, Byun HS, et al. Triphasic perfusion computed tomography in acute middle cerebral artery stroke: correlation with angiographic findings. Arch Neurol. 2000. 57:990–999.6. Lee KH, Lee SJ, Cho SJ, et al. Usefulness of triphasic perfusion computed tomography for intravenous thrombolysis with tissue-type plasminogen activator in acute ischemic stroke. Arch Neurol. 2000. 57:1000–1008.7. Lev MH, Farkas J, Rodriguez VR, et al. CT angiography in the rapid triage of patients with hyperacute stroke to intraarterial thrombolysis: accuracy in the detection of large vessel thrombus. J Comput Assist Tomogr. 2001. 25:520–528.8. Lev MH, Segal AZ, Farkas J, et al. Utility of perfusion-weighted CT imaging in acute middle cerebral artery stroke treated with intra-arterial thrombolysis: prediction of final infarct volume and clinical outcome. Stroke. 2001. 32:2021–2028.9. Kidwell CS, Saver JL, Mattiello J, et al. Thrombolytic reversal of acute human cerebral ischemic injury shown by diffusion/perfusion magnetic resonance imaging. Ann Neurol. 2000. 47:462–469.10. Fiehler J, Foth M, Kucinski T, et al. Severe ADC decreases do not predict irreversible tissue damage in humans. Stroke. 2002. 33:79–86.11. Barber PA, Darby DG, Desmond PM, et al. Prediction of stroke outcome with echoplanar perfusion- and diffusion-weighted MRI. Neurology. 1998. 51:418–426.12. Neumann-Haefelin T, Wittsack HJ, et al. Diffusion- and perfusion-weighted MRI: influence of severe carotid artery stenosis on the DWI/PWI mismatch in acute stroke. Stroke. 2000. 31:1311–1317.13. Rohl L, Ostergaard L, Simonsen CZ, et al. Viability thresholds of ischemic penumbra of hyperacute stroke defined by perfusion-weighted MRI and apparent diffusion coefficient. Stroke. 2001. 32:1140–1146.14. Grandin CB, Duprez TP, Smith AM, et al. Usefulness of magnetic resonance-derived quantitative measurements of cerebral blood flow and volume in prediction of infarct growth in hyperacute stroke. Stroke. 2001. 32:1147–1153.15. Woods RP, Grafton ST, Holmes CJ, Cherry SR, Mazziotta JC. Automated image registration: I. General methods and intrasubject, intramodality validation. J Comput Assist Tomogr. 1998. 22:139–152.16. von Kummer R, Bourquain H, Bastianello S, et al. Early prediction of irreversible brain damage after ischemic stroke at CT. Radiology. 2001. 219:95–100.17. Patel SC, Levine SR, Tilley BC, et al. National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Lack of clinical significance of early ischemic changes on computed tomography in acute stroke. JAMA. 2001. 286:2830–2838.18. Marks MP, Holmgren EB, Fox AJ, Patel S, von Kummer R, Froehlich J. Evaluation of early computed tomographic findings in acute ischemic stroke. Stroke. 1999. 30:389–392.19. Lovblad KO, Baird AE, Schlaug G, et al. Ischemic lesion volumes in acute stroke by diffusion-weighted magnetic resonance imaging correlated with clinical outcome. Ann Neurol. 1997. 42:164–170.20. Tong DC, Yenari MA, Albers GW, O'Brien M, Marks MP, Moseley ME. Correlation of perfusion- and diffusion-weighted MR in patients with NIHSS score in acute (<6.5 hour) ischemic stroke. Neurology. 1998. 50:864–870.21. Schellinger PD, Fiebach JB, Jansen O, et al. Stroke magnetic resonance imaging within 6 hours after onset of hyperacute cerebral ischemia. Ann Neurol. 2001. 49:460–469.22. Beaulieu C, de Crespigny A, Tong DC, Moseley ME, Albers GW, Marks MP. Longitudinal magnetic resonance imaging study of perfusion and diffusion in stroke: evolution of lesion volume and correlation with clinical outcome. Ann Neurol. 1999. 46:568–578.23. Pantano P, Caramia F, Bozzao L, Dieler C, von Kummer R. Delayed increase in infarct volume after cerebral ischemia: correlations with thrombolytic treatment and clinical outcome. Stroke. 1999. 30:502–507.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Utility of First-Pass Perfusion CT in Hyperacute Ischemic Stroke: Early Experience
- Findings of Perfusion MR Imaging in Acute Middle Cerebral Artery Territory Ischemic Stroke
- Clinical Usefulness of Perfusion CT in Acute Ischemic Stroke
- Surgical Management of Acute Stroke
- The Usefulness of Perfusion CT in Acute Cerebral Ischemic Infarction