J Korean Med Assoc.
2009 Apr;52(4):375-381. 10.5124/jkma.2009.52.4.375.
Surgical Management of Acute Stroke
- Affiliations
-
- 1Department of Neurology, Ulsan University College of Medicine, Korea. jhkwon-or@hanmail.net
- KMID: 2137722
- DOI: http://doi.org/10.5124/jkma.2009.52.4.375
Abstract
- Stroke is a most common neurological disease leading to mortality and morbidity. Many clinical evidences confirm that medical treatment including thrombolytic and antithrombotic therapy may improve the clinical outcome in patients with acute ischemic stroke. However, little information exists about effectiveness and safety of reperfusion surgery such as emergency carotid endarterectomy and extracranial-intracranial bypass surgery in patients with acute ischemic stroke and limits its wide application. Recent pooled analysis of three randomized controlled clinical trials-DECIMAL (decompressive craniectomy in malignant middle cerebral artery infarcts) trial; DESTINY (decompressive surgery for the treatment of malignant infarction of the middle cerebral artery) trial; and HAMLET (hemicraniectomy after middle cerebral artery infarction with life-threatening edema trial) reported decompressive surgery undertaken within 48 hours of stroke onset in patients with malignant middle cerebral artery infarction reduced mortality and morbidity. However, decompressive surgery in patients with malignant middle cerebral artery infarction should be done according to the clinical conditions of individual patients. No clear evidences are present on that craniotomy, minimally invasive surgery, and early clot evacuation are effective on functional outcome of patients with spontaneous intracerebral hemorrhage compared with initial conservative therapy. In conclusion, a lot of well-designed studies are needed to recommend appropriate surgical management in patients with acute ischemic and hemorrhagic stroke.
MeSH Terms
Figure
Reference
-
1. Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, Grubb RL, Higashida RT, Jauch EC, Kidwell C, Lyden PD, Morgenstern LB, Qureshi AI, Rosenwasser RH, Scott PA, Wijdicks EF. American Heart Association; American Stroke Association Stroke Council; Clinical Cardiology Council; Cardiovascular Radiology and Intervention Council; Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007. 38:1655–1711.
Article2. Meyer FB, Sundt TM Jr, Piepgras DG, Sandok BA, Forbes G. Emergency carotid endarterectomy for patients with acute carotid occlusion and profound neurological deficits. Ann Surg. 1986. 203:82–89.
Article3. Kasper GC, Wladis AR, Lohr JM, Roedersheimer LR, Reed RL, Miller TJ, et al. Carotid thromboendarterectomy for recent total occlusion of the internal carotid artery. J Vasc Surg. 2001. 33:242–249.
Article4. Gay JL, Curtil A, Buffiere S, Favre JP, Barral X. Urgent carotid artery repair: retrospective study of 21 cases. Ann Vasc Surg. 2002. 16:401–406.
Article5. Heros RC. Carotid endarterectomy in patients with intraluminal thrombus. Stroke. 1988. 19:667–668.
Article6. Buchan A, Gates P, Pelz D, Barnett HJ. Intraluminal thrombus in the cerebral circulation. Implications for surgical management. Stroke. 1988. 19:681–687.
Article7. BT A. Treatment of acute traumatic internal carotid artery occlusion with extracranial-to-intracranial arterial bypass: case report. Neurosurgery. 1989. 25:90–92.
Article8. Kakinuma K, Ezuka I, Takai N, Yamamoto K, Sasaki O. The simple indicator for revascularization of acute middle cerebral artery occlusion using angiogram and ultra-early embolectomy. Surg Neurol. 1999. 51:332–341.
Article9. Linskey ME, Sekhar LN, Hecht ST. Emergency embolectomy for embolic occlusion of the middle cerebral artery after internal carotid artery balloon test occlusion. Case report. J Neurosurg. 1992. 77:134–138.
Article10. Frank JI. Large hemispheric infarction, deterioration, and intracranial pressure. Neurology. 1995. 45:1286–1290.
Article11. Qureshi AI, Suarez JI, Yahia AM, Mohammad Y, Uzun G, Suri MF, et al. Timing of neurologic deterioration in massive middle cerebral artery infarction: a multicenter review. Crit Care Med. 2003. 31:272–277.
Article12. Manno EM, Nichols DA, Fulgham JR, Wijdicks EF. Computed tomographic determinants of neurologic deterioration in patients with large middle cerebral artery infarctions. Mayo Clin Proc. 2003. 78:156–160.
Article13. Heinsius T, Bogousslavsky J, Van Melle G. Large infarcts in the middle cerebral artery territory. Etiology and outcome patterns. Neurology. 1998. 50:341–350.
Article14. Wijdicks EF, Diringer MN. Middle cerebral artery territory infarction and early brain swelling: progression and effect of age on outcome. Mayo Clin Proc. 1998. 73:829–836.
Article15. Maramattom BV, Bahn MM, Wijdicks EF. Which patient fares worse after early deterioration due to swelling from hemispheric stroke? Neurology. 2004. 63:2142–2145.
Article16. Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Kummer R. 'Malignant' middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol. 1996. 53:309–315.
Article17. Berrouschot J, Sterker M, Bettin S, Koster J, Schneider D. Mortality of space-occupying ('malignant') middle cerebral artery infarction under conservative intensive care. Intensive Care Med. 1998. 24:620–623.
Article18. H J, vdW HB, K LJ. Treatment of space-occupying cerebral infarction. Crit Care Med. 2003. 31:617–625.
Article19. Rieke K, Schwab S, Krieger D, von Kummer R, Aschoff A, Schuchardt V, Hacke W. Decompressive surgery in space-occupying hemispheric infarction: results of an open, prospective trial. Crit Care Med. 1995. 23:1576–1587.20. Schwab S, Steiner T, Aschoff A, Schwarz S, Steiner HH, Jansen O, Hacke W. Early hemicraniectomy in patients with complete middle cerebral artery infarction. Stroke. 1998. 29:1888–1893.
Article21. Morley N, Berge E, Cruz-Flores S, Whittle I. Surgical decompression for cerebral edema in acute ischemic stroke. Stroke. 2003. 34:1337.
Article22. Gupta R, Connolly ES, Mayer S, Elkind MS. Hemicraniectomy for massive middle cerebral artery territory infarction: a systematic review. Stroke. 2004. 35:539–543.
Article23. H J, A GJ, A A, vG J, M MR, K LJ, et al. Hemicraniectomy after middle cerebral artery infarction with life-threatening Edema trial (HAMLET). Protocol for a randomised controlled trial of decompressive surgery in space-occupying hemispheric infarction. Trials. 2006. 7:29.
Article24. Jüttler E, Schwab S, Schmiedek P, Unterberg A, Hennerici M, Woitzik J, Witte S, Jenetzky E, Hacke W. DESTINY Study Group. Decompressive Surgery for the Treatment of Malignant Infarction of the Middle Cerebral Artery (DESTINY): a randomized, controlled trial. Stroke. 2007. 38:2518–2525.
Article25. Vahedi K, Vicaut E, Mateo J, Kurtz A, Orabi M, Guichard JP, Boutron C, Couvreur G, Rouanet F, Touzé E, Guillon B, Carpentier A, Yelnik A, George B, Payen D, Bousser MG. DECIMAL Investigators. Sequential-design, multicenter, randomized, controlled trial of early decompressive craniectomy in malignant middle cerebral artery infarction (DECIMAL Trial). Stroke. 2007. 38:2506–2517.
Article26. Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A, Amelink GJ, Schmiedeck P, Schwab S, Rothwell PM, Bousser MG, van der Worp HB, Hacke W. DECIMAL, DESTINY, and HAMLET investigators. Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol. 2007. 6:215–222.
Article27. Hornig CR, Rust DS, Busse O, Jauss M, Laun A. Space-occupying cerebellar infarction. Clinical course and prognosis. Stroke. 1994. 25:372–374.
Article28. Mathew P, Teasdale G, Bannan A, Oluoch-Olunya D. Neurosurgical management of cerebellar haematoma and infarct. J Neurol Neurosurg Psychiatry. 1995. 59:287–292.
Article29. E JA, N-T DE, S SI. Diagnosis and initial management of cerebellar infarction. Lancet Neurol. 2008. 7:951–964.
Article30. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 2008. 25:457–507.31. Chen HJ, Lee TC, Wei CP. Treatment of cerebellar infarction by decompressive suboccipital craniectomy. Stroke. 1992. 23:957–961.
Article32. Broderick JP, Brott T, Tomsick T, Miller R, Huster G. Intracerebral hemorrhage more than twice as common as subarachnoid hemorrhage. J Neurosurg. 1993. 78:188–191.
Article33. Anderson CS, Chakera TM, Stewart-Wynne EG, Jamrozik KD. Spectrum of primary intracerebral haemorrhage in Perth, Western Australia, 1989-90: incidence and outcome. J Neurol Neurosurg Psychiatry. 1994. 57:936–940.
Article34. Bamford J, Dennis M, Sandercock P, Burn J, Warlow C. The frequency, causes and timing of death within 30 days of a first stroke: the Oxfordshire Community Stroke Project. J Neurol Neurosurg Psychiatry. 1990. 53:824–829.
Article35. Broderick J, Connolly S, Feldmann E, Hanley D, Kase C, Krieger D, Mayberg M, Morgenstern L, Ogilvy CS, Vespa P, Zuccarello M. American Heart Association; American Stroke Association Stroke Council; High Blood Pressure Research Council; Quality of Care and Outcomes in Research Interdisciplinary Working Group. Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Stroke. 2007. 38:2001–2023.
Article36. Juvela S, Heiskanen O, Poranen A, Valtonen S, Kuurne T, Kaste M, Troupp H. The treatment of spontaneous intracerebral hemorrhage. A prospective randomized trial of surgical and conservative treatment. J Neurosurg. 1989. 70:755–758.37. Zuccarello M, Brott T, Derex L, Kothari R, Sauerbeck L, Tew J, Van Loveren H, Yeh HS, Tomsick T, Pancioli A, Khoury J, Broderick J. Early surgical treatment for supratentorial intracerebral hemorrhage: a randomized feasibility study. Stroke. 1999. 30:1833–1839.
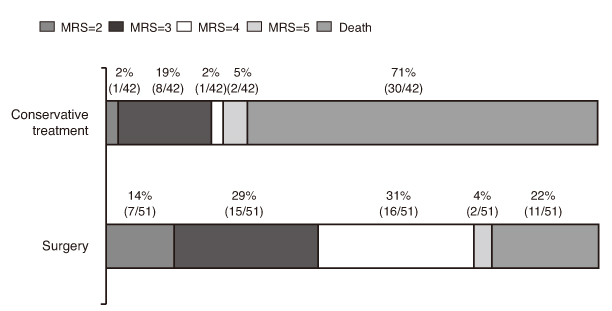
Article38. Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, Hope DT, Karimi A, Shaw MD, Barer DH. STICH investigators. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. The Lancet. 2005. 365:387–397.
Article39. van Loon J, Van Calenbergh F, Goffin J, Plets C. Controversies in the management of spontaneous cerebellar haemorrhage. A consecutive series of 49 cases and review of the literature. Acta Neurochir (Wien). 1993. 122:187–193.
Article40. Firsching R, Huber M, Frowein RA. Cerebellar haemorrhage: management and prognosis. Neurosurg Rev. 1991. 14:191–194.
Article41. Da Pian R, Bazzan A, Pasqualin A. Surgical versus medical treatment of spontaneous posterior fossa haematomas: a cooperative study on 205 cases. Neurol Res. 1984. 6:145–151.
Article42. Kirollos RW, Tyagi AK, Ross SA, van Hille PT, Marks PV. Management of spontaneous cerebellar hematomas: a prospective treatment protocol. Neurosurgery. 2001. 49:1378–1386.
Article43. Morioka J, Fujii M, Kato S, Fujisawa H, Akimura T, Suzuki M, Kobayashi S. Japan Standard Stroke Registry Group (JSSR). Surgery for spontaneous intracerebral hemorrhage has greater remedial value than conservative therapy. Surg Neurol. 2006. 65:67–72.
Article44. Auer LM, Deinsberger W, Niederkorn K, Gell G, Kleinert R, Schneider G, Holzer P, Bone G, Mokry M, K_rner E, et al. Endoscopic surgery versus medical treatment for spontaneous intracerebral hematoma: a randomized study. J Neurosurg. 1989. 70:530–535.
Article45. Teernstra OP, Evers SM, Lodder J, Leffers P, Franke CL, Blaauw G. Stereotactic treatment of intracerebral hematoma by means of a plasminogen activator: a multicenter randomized controlled trial (SICHPA). Stroke. 2003. 34:968–974.
Article46. Morgan T, Zuccarello M, Narayan R, Keyl P, Lane K, Hanley D. Preliminary findings of the minimally-invasive surgery plus rtPA for intracerebral hemorrhage evacuation (MISTIE) clinical trial. Acta Neurochir Suppl. 2008. 105:147–151.
Article47. Kaneko M, Tanaka K, Shimada T, Sato K, Uemura K. Long-term evaluation of ultra-early operation for hypertensive intracerebral hemorrhage in 100 cases. J Neurosurg. 1983. 58:838–842.
Article48. Morgenstern LB, Demchuk AM, Kim DH, Frankowski RF, Grotta JC. Rebleeding leads to poor outcome in ultra-early craniotomy for intracerebral hemorrhage. Neurology. 2001. 56:1294–1299.
Article49. Tan SH, Ng PY, Yeo TT, Wong SH, Ong PL, Venketasubramanian N. Hypertensive basal ganglia hemorrhage: a prospective study comparing surgical and nonsurgical management. Surg Neurol. 2001. 56:287–292.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Organization of Stroke Care System: Stroke Unit and Stroke Center
- General Management of Acute Stroke
- Surgical Treatment of Cerebral Ischemia
- Blood Pressure Management for Stroke Prevention and in Acute Stroke
- Pneumococcal meningitis complicated by otomastoiditis and pneumocephalus confounding an acute ischemic stroke diagnosis