Korean J Radiol.
2003 Mar;4(1):61-65. 10.3348/kjr.2003.4.1.61.
Acute Necrotizing Encephalopathy: Diffusion MR Imaging and Localized Proton MR Spectroscopic Findings in Two Infants
- Affiliations
-
- 1Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. cgchoi@www.amc.seoul.kr
- 2Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 754044
- DOI: http://doi.org/10.3348/kjr.2003.4.1.61
Abstract
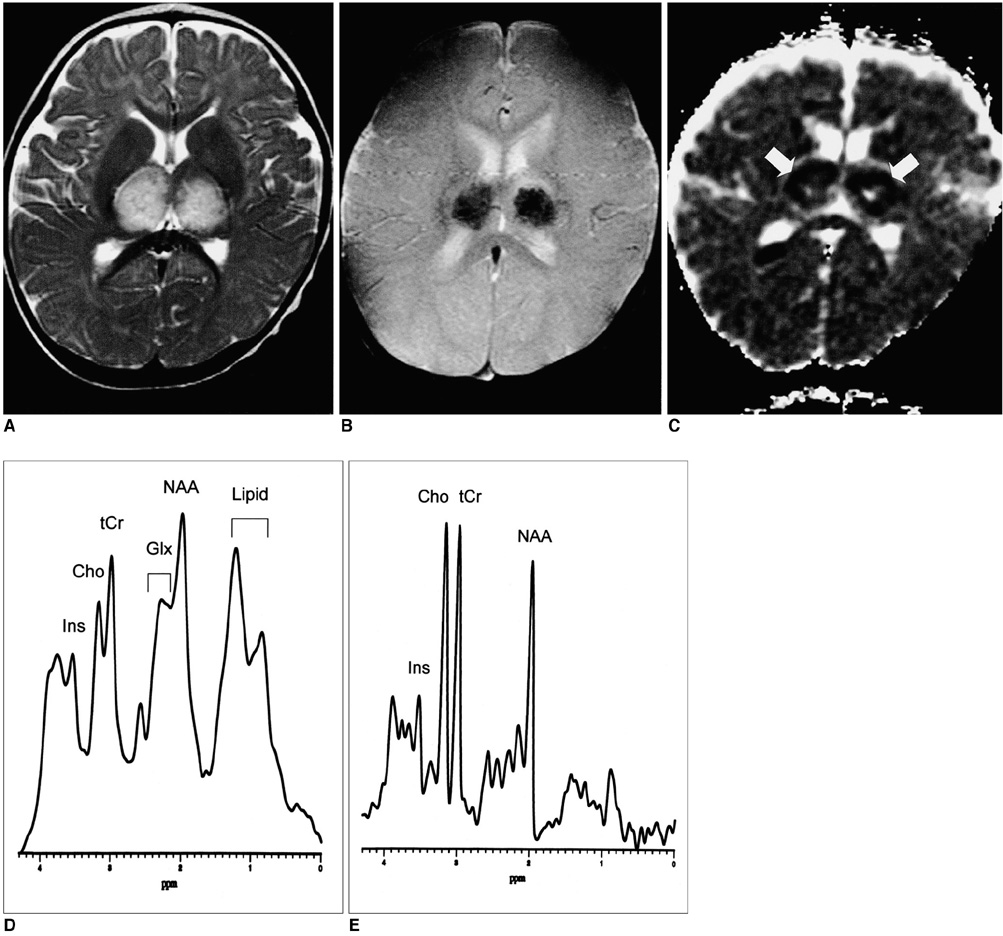
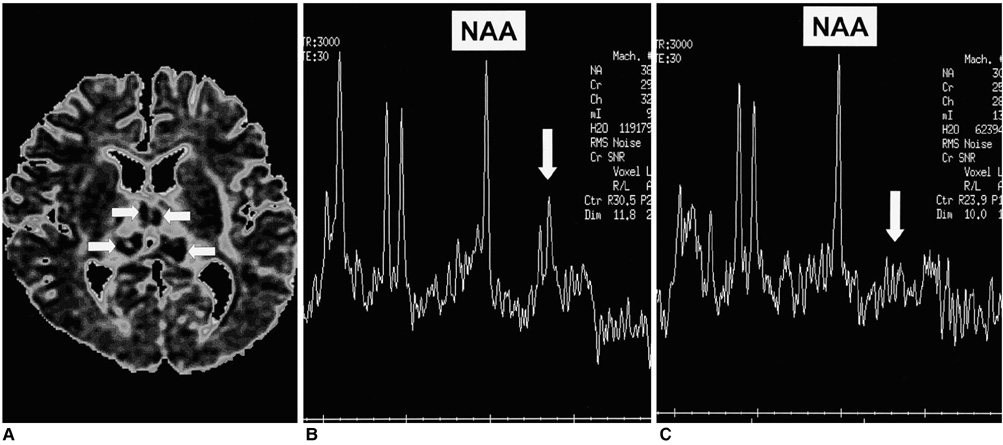
- In this report, we describe the findings of diffusion MR imaging and proton MR spectroscopy in two infants with acute necrotizing encephalopathy in which there was characteristic symmetrical involvement of the thalami. Diffusion MR images of the lesions showed that the observed apparent diffusion coefficient (ADC) decrease was more prominent in the first patient, who had more severe brain damage and a poorer clinical outcome, than in the second. Proton MR spectroscopy detected an increase in the glutamate/glutamine complex and mobile lipids in the first case but only a small increase of lactate in the second. Diffusion MR imaging and proton MR spectroscopy may provide useful information not only for diagnosis but also for estimating the severity and clinical outcome of acute necrotizing encephalopathy.
Keyword
Figure
Cited by 2 articles
-
Clinical Spectrum and Prognostic Factors of Acute Necrotizing Encephalopathy in Children
Hye-Eun Seo, Su-Kyeong Hwang, Byung Ho Choe, Min-Hyun Cho, Sung-Pa Park, Soonhak Kwon
J Korean Med Sci. 2010;25(3):449-453. doi: 10.3346/jkms.2010.25.3.449.Arterial Spin Labelling Perfusion, Proton MR Spectroscopy and Susceptibility-Weighted MR Findings of Acute Necrotizing Encephalopathy: a Case Report
Hwanwoong Kwon, Dae Seob Choi, Jungho Jang
Investig Magn Reson Imaging. 2019;23(2):157-161. doi: 10.13104/imri.2019.23.2.157.
Reference
-
1. Mizuguchi M. Acute necrotizing encephalopathy of childhood: a novel form of acute encephalopathy prevalent in Japan and Taiwan. Brain Dev. 1997. 19:81–92.2. Mizuguchi M, Abe J, Mikkaichi K, et al. Acute necrotizing encephalopathy of childhood: a new syndrome presenting with multifocal, symmetric brain lesions. J Neurol Neurosurg Psychiatry. 1995. 58:555–561.3. Yagishita A, Nakano I, Ushioda T, Otsuki N, Hasegawa A. Acute encephalopathy with bilateral thalamotegmental involvement in infants and children: imaging and pathology findings. AJNR Am J Neuroradiol. 1995. 16:439–447.4. Fujimoto Y, Shibata M, Tsuyuki M, Okada M, Tsuzuki K. Influenza A virus encephalopathy with symmetrical thalamic lesions. Eur J Pediatr. 2000. 159:319–321.5. Porto L, Lanferman H, Moller-Hartmann W, Jacobi G, Zanella F. Acute necrotizing encephalopathy of childhood after exanthema subitum outside Japan or Taiwan. Neuroradiology. 1999. 41:732–734.6. Campistol J, Gassio R, Pineda M, Fernandez-Alvarez E. Acute necrotizing encephalopathy of childhood (infantile bilateral thalamic necrosis): two non-Japanese cases. Dev Med Child Neurol. 1998. 40:771–774.7. Kim YJ, Chun KA, Kim KT, Choi KH, Kim YH. MR imaging of acute necrotizing encephalopathy: a report of two cases. J Korean Radiol Soc. 2001. 44:633–636.8. Harada M, Hisaoka S, Mori K, Yoneda K, Noda SN, Nishitani H. Differences in water diffusion and lactate production in two different types of postinfectious encephalopathy. J Magn Reson Imaging. 2000. 11:559–563.9. Mizuguchi M, Hayashi M, Nakano I, et al. Concentric structure of thalamic lesions in acute necrotizing encephalopathy. Neuroradiology. 2002. 44:489–493.10. Kang BK, Na DG, Ryoo JW, Byun HS, Roh HG, Pyeun YS. Diffusion-weighted MR imaging of intracerebral hemorrhage. Korean J Radiol. 2001. 2:183–191.11. de Graaf AA, Deutz NE, Bosman DK, Chamuleau RA, de Haan JG, Bovee WM. The use of in-vivo proton NMR to study the effects of hyperammonemia in the rat cerebral cortex. NMR Biomed. 1991. 4:31–37.12. Munakata M, Kato R, Yokoyama H, et al. Combined therapy with hypothermia and anticytokine agents in influenza A encephalopathy. Brain Dev. 2000. 22:373–377.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arterial Spin Labelling Perfusion, Proton MR Spectroscopy and Susceptibility-Weighted MR Findings of Acute Necrotizing Encephalopathy: a Case Report
- MR Imaging of Acute Necrotizing Encephalopathy:A Report of Two Cases
- Diffusion-Weighted MR Imaging in Acute Wernicke's Encephalopathy Associated with Pseudomembranous Colitis: A Case Report and Review of the Literature
- Localized Proton MR Spectroscopic Detection of Nonketotic Hyperglycinemia in an Infant
- Uremic Encephalopathy with Atypical Magnetic Resonance Features on Diffusion-Weighted Images